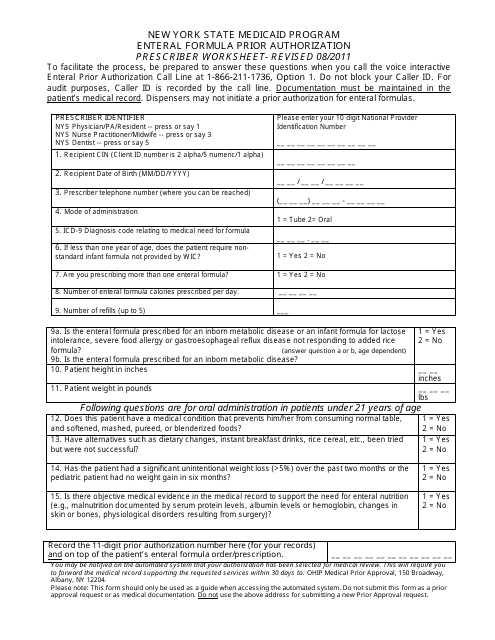
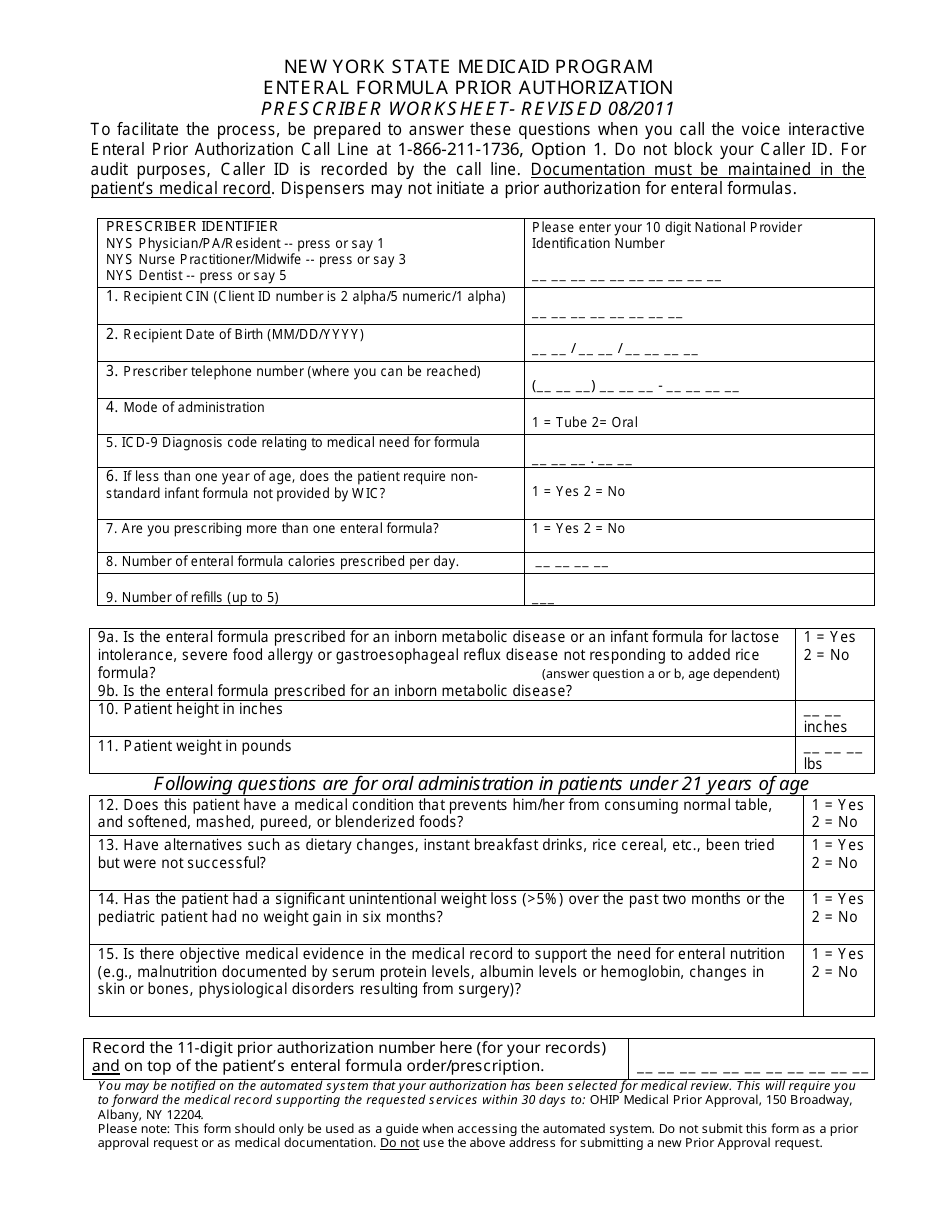
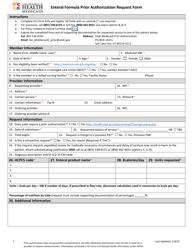
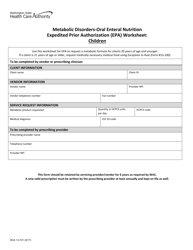
Enteral Formula Prior Authorization Prescriber Worksheet - New York State Medicaid Program - New York
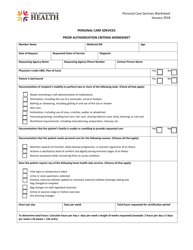
The Enteral Formula Prior Authorization Prescriber Worksheet is used in the New York State Medicaid Program to request prior authorization for enteral formula. Prior authorization is required to ensure that the prescribed formula is medically necessary and meets the program's coverage criteria.
The Enteral Formula Prior Authorization Prescriber Worksheet for the New York State Medicaid Program is typically filed by the prescribing healthcare provider or the authorized representative.
FAQ
Q: What is the Enteral Formula Prior Authorization Prescriber Worksheet?
A: The Enteral Formula Prior Authorization Prescriber Worksheet is a document used by healthcare providers to request prior authorization for enteral formula coverage under the New York State Medicaid Program.
Q: Who uses the Enteral Formula Prior Authorization Prescriber Worksheet?
A: Healthcare providers use the Enteral Formula Prior Authorization Prescriber Worksheet to request prior authorization for enteral formula coverage for their patients under the New York State Medicaid Program.
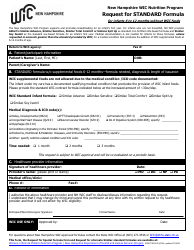
Q: What is enteral formula?
A: Enteral formula is a specialized liquid nutrition that is used for patients who are unable to eat or digest normal food.
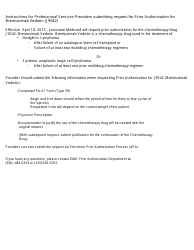
Q: What is prior authorization?
A: Prior authorization is a process where healthcare providers must obtain approval from the insurance provider, in this case, the New York State Medicaid Program, before certain medical services or medications are covered.
Q: Why do healthcare providers need to request prior authorization for enteral formula?
A: Healthcare providers need to request prior authorization for enteral formula to ensure that the cost of the formula is covered by the New York State Medicaid Program.