Prior Authorization Templates
Documents:
390
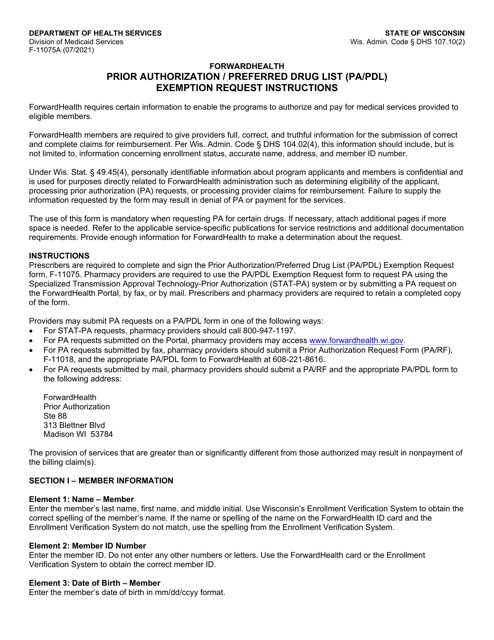
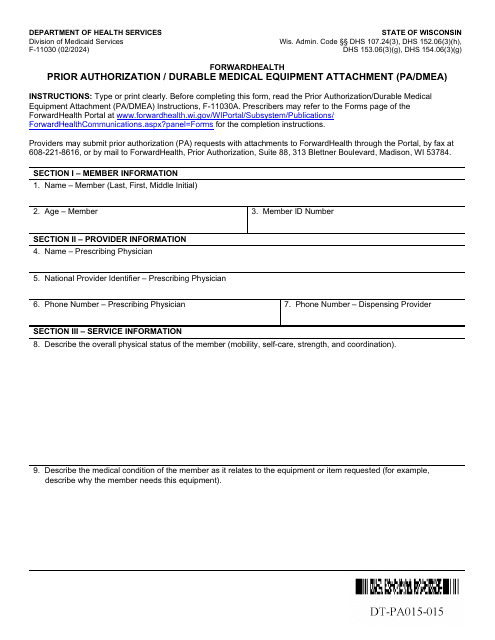
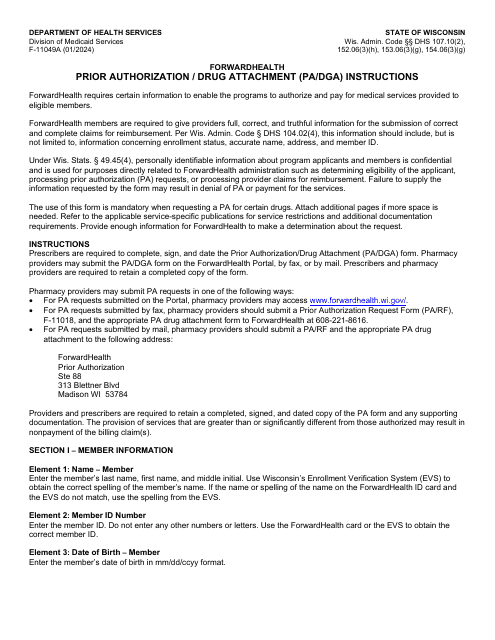
This Form is used for requesting a Prior Authorization or a Preferred Drug List exemption in Wisconsin. It provides instructions on how to complete the form and submit it for review.
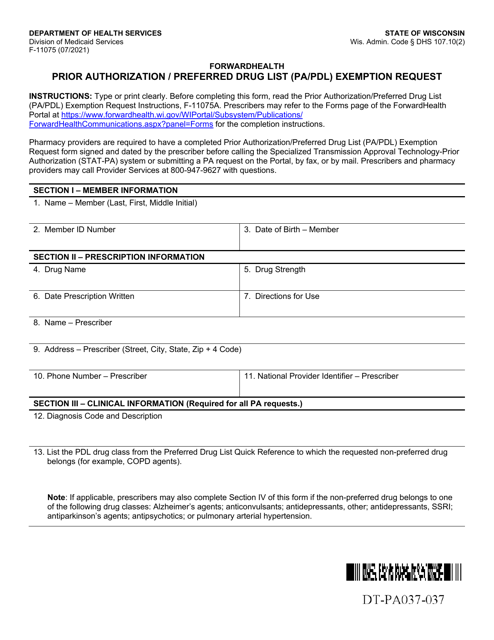
This Form is used to request an exemption from the Prior Authorization/Preferred Drug List (PA/PDL) requirement in Wisconsin.
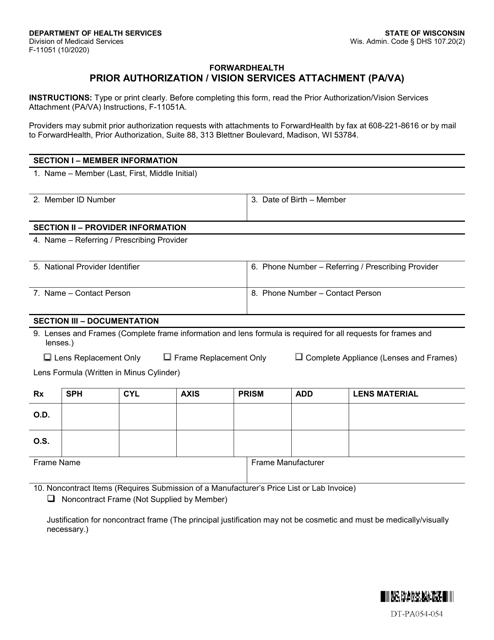
This Form is used for prior authorization of vision services in Wisconsin.
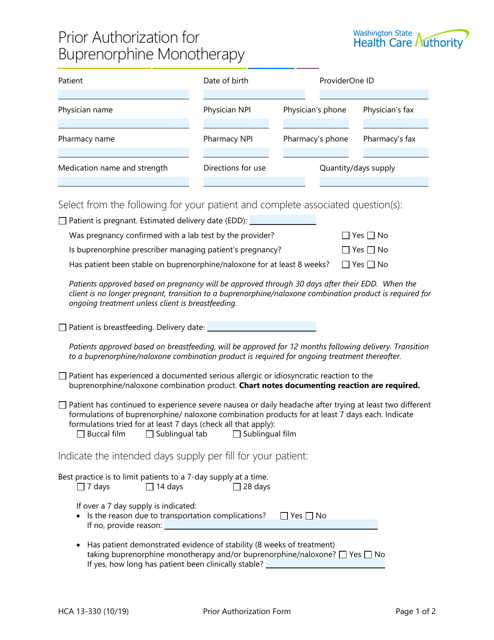
This form is used for requesting prior authorization for buprenorphine monotherapy in Washington.
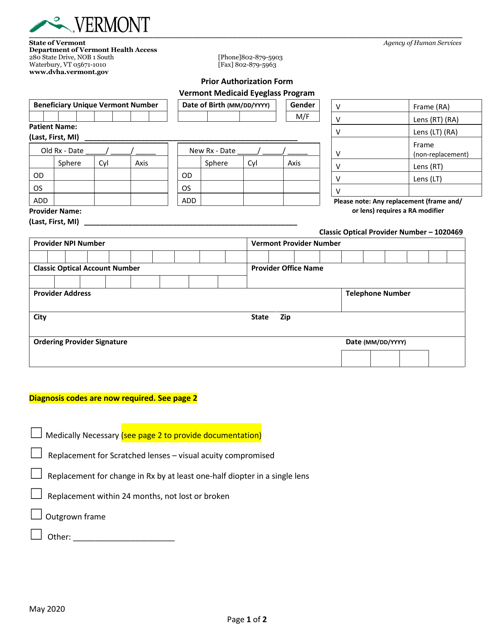
This form is used for requesting prior authorization for the Vermont Medicaid Eyeglass Program in Vermont.
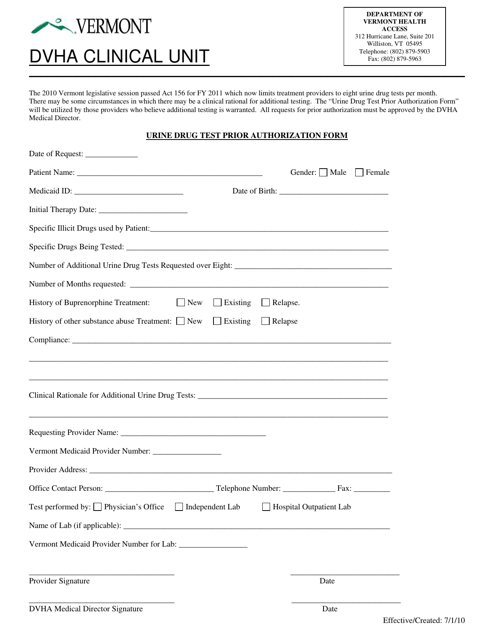
This form is used for requesting prior authorization for a urine drug test in the state of Vermont. It helps ensure that the test will be covered by insurance.
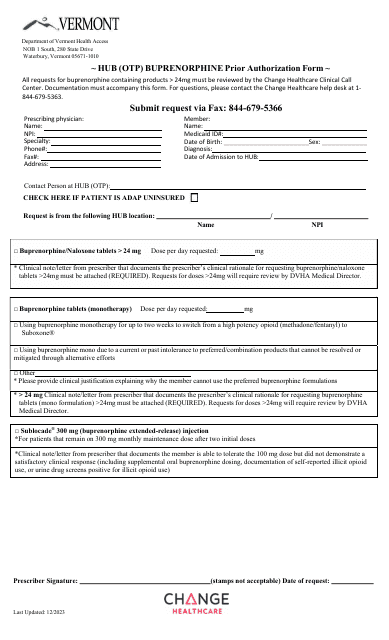
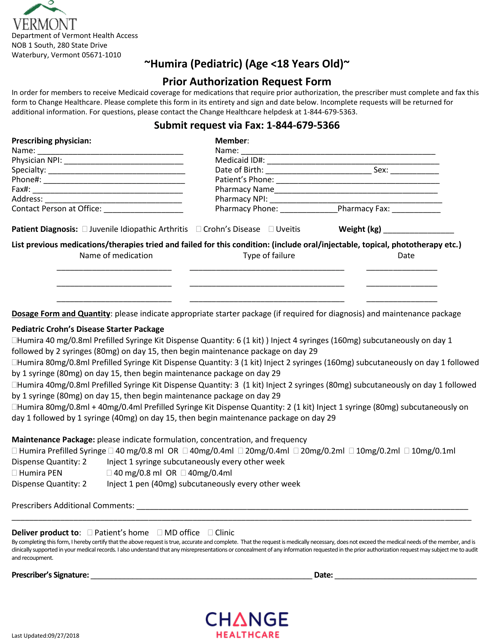
This form is used for requesting prior authorization for Humira (Pediatric) for patients who are 18 years old or younger in the state of Vermont.
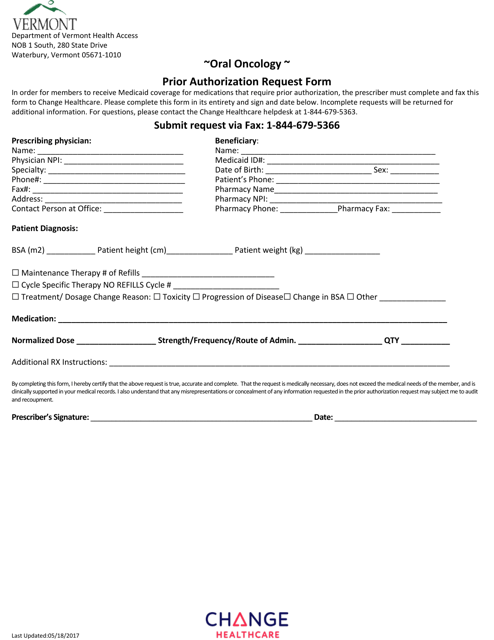
This form is used for submitting a prior authorization request for oral oncology treatment in the state of Vermont.
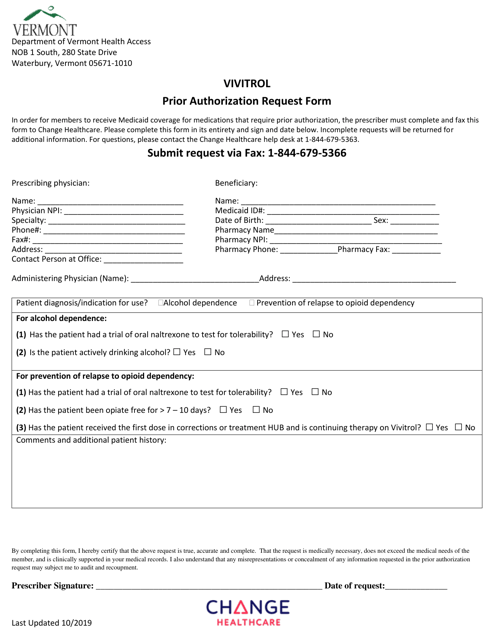
This form is used for requesting prior authorization for Vivitrol medication in the state of Vermont.
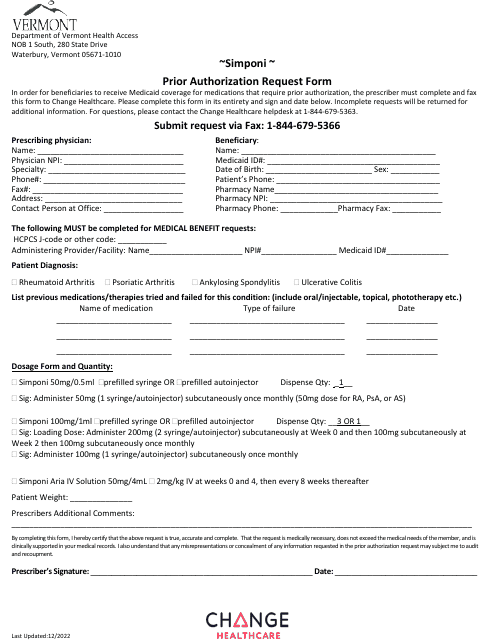
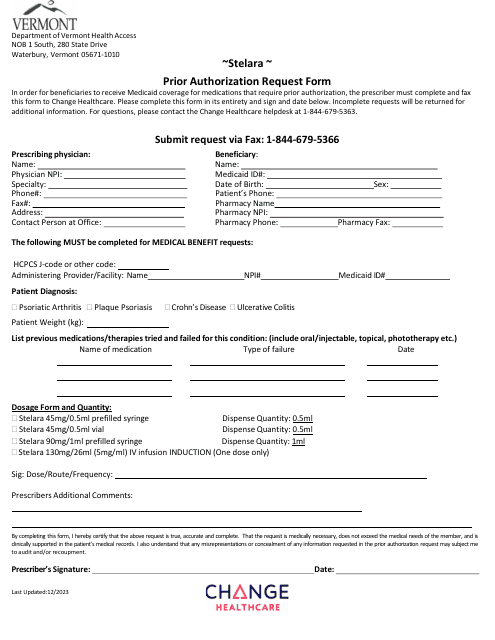
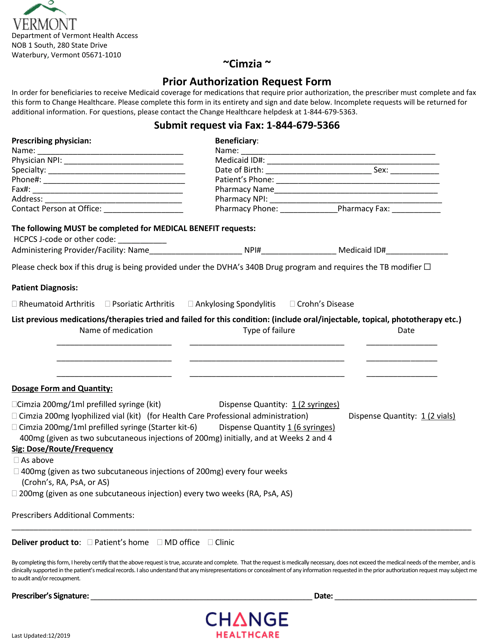
This document is a Cimzia Prior Authorization Form specific to the state of Vermont. It is a required form to obtain prior authorization for Cimzia medication.
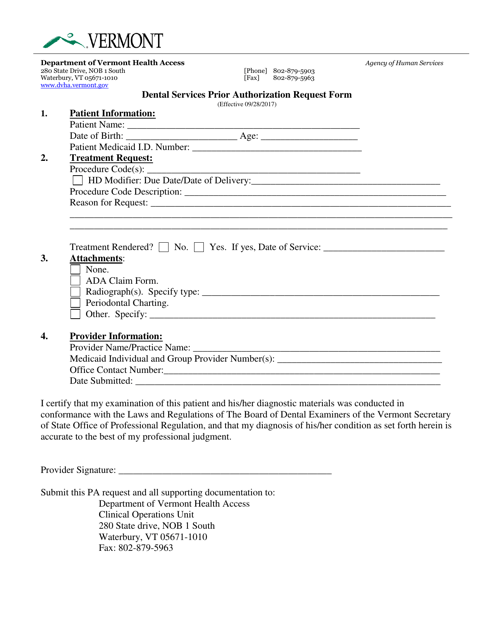
This document is used for requesting prior authorization for dental services in the state of Vermont.
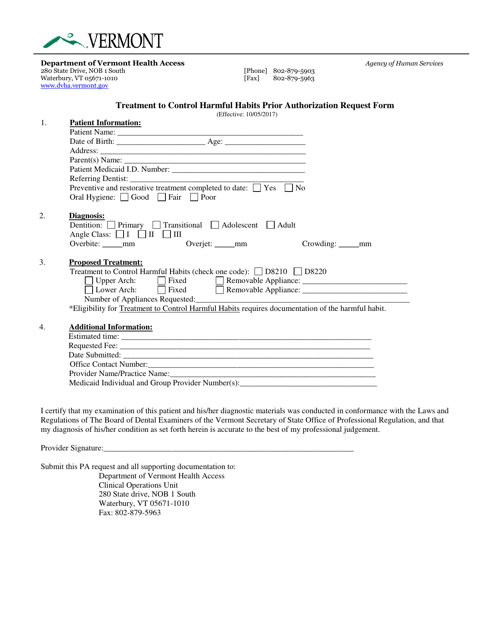
This Form is used for requesting prior authorization for treatment to control harmful habits in the state of Vermont.
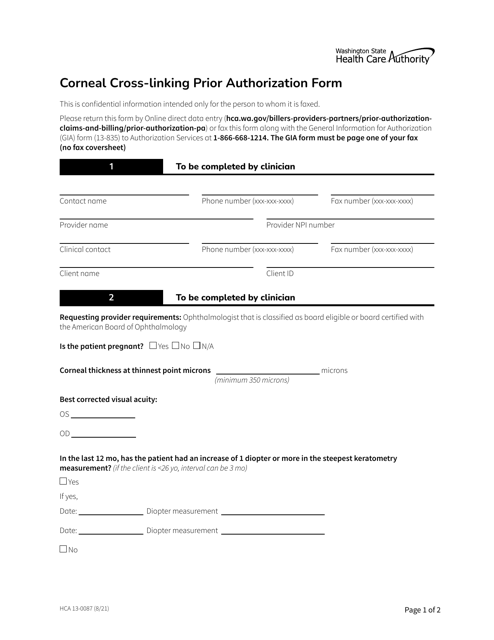
This Form is used for obtaining prior authorization for corneal cross-linking in the state of Washington.
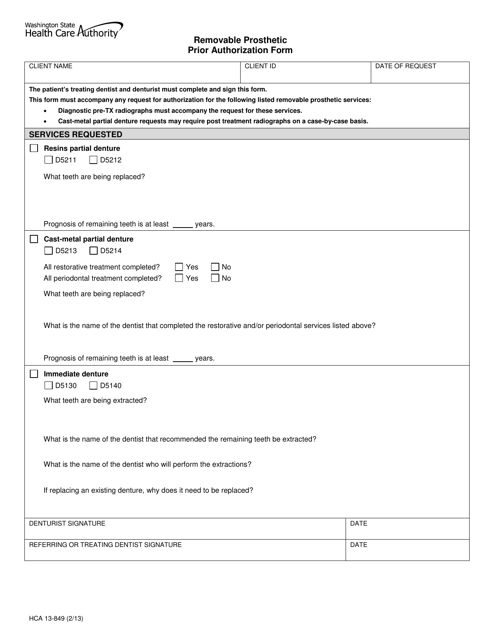
This Form is used for requesting prior authorization for removable prosthetic devices in the state of Washington.
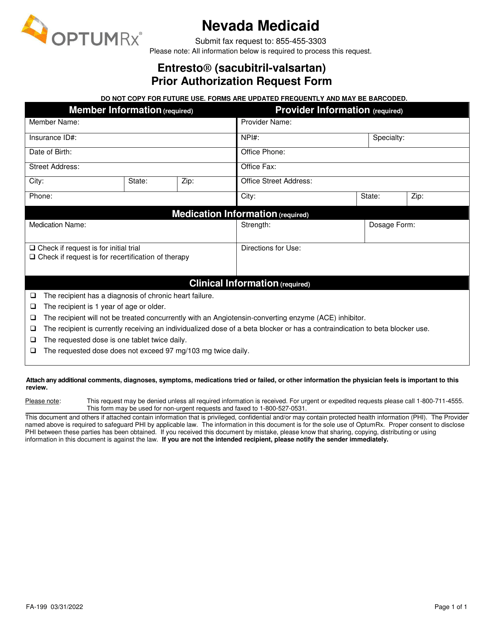
This Form is used for requesting prior authorization for the medication Entresto (Sacubitril-Valsartan) in Nevada. Prior authorization is required for this medication in order to ensure proper coverage and payment.
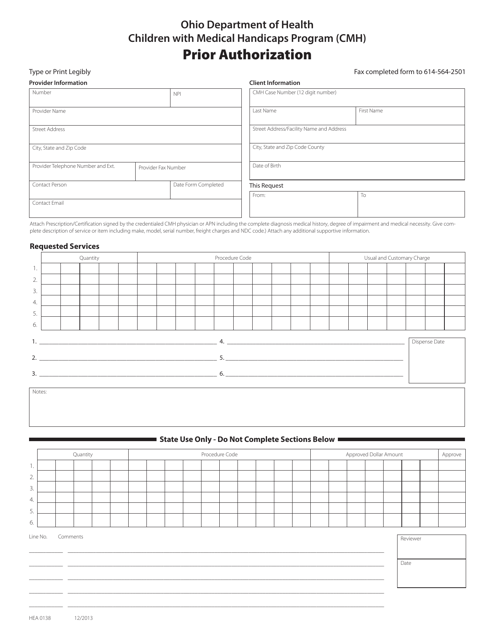
This Form is used for Medicaid recipients in Ohio to request prior authorization for services under the Children With Medical Handicaps Program (CMH).
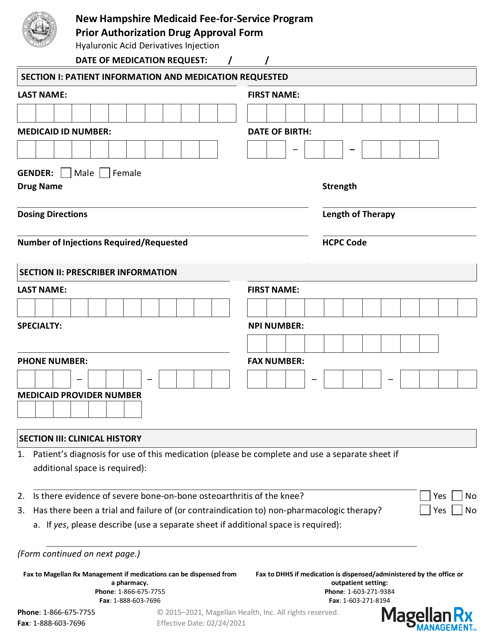
This Form is used for obtaining prior authorization for Hyaluronic Acid Derivatives Injection in the Medicaid Fee-For-Service Program in New Hampshire.
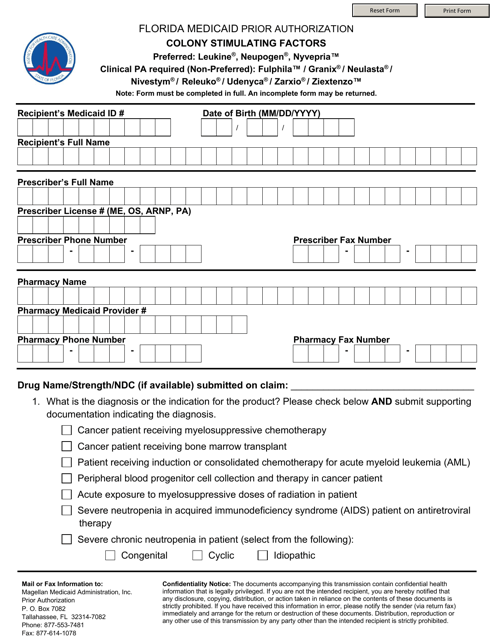
This form is used for Medicaid patients in Florida who need prior authorization for colony stimulating factors.
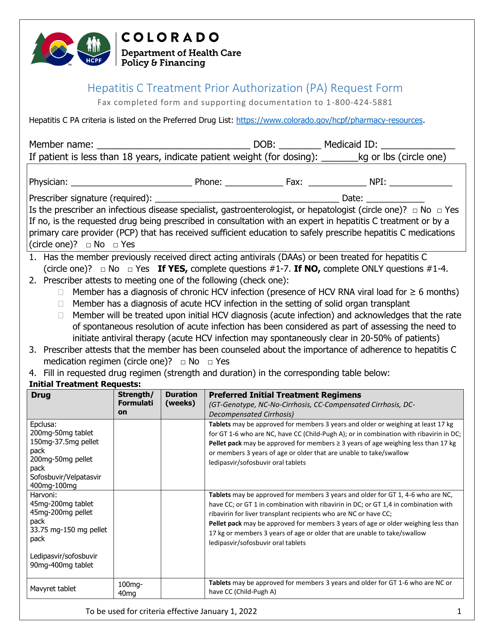
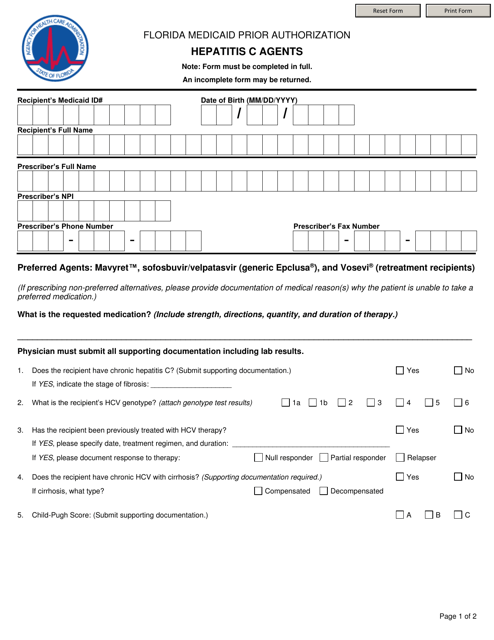
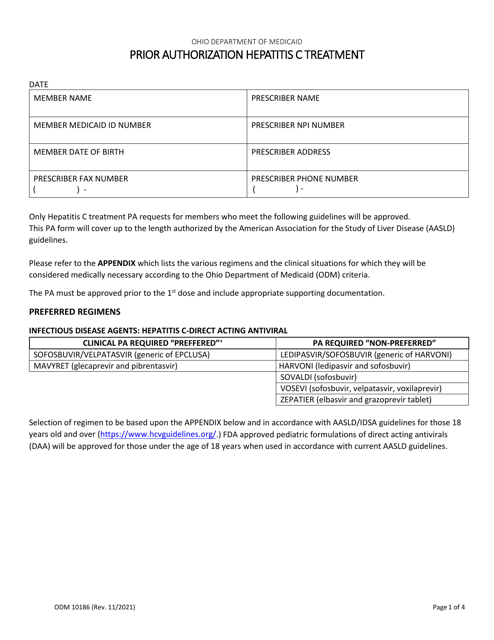
This form is used for requesting prior authorization for Medicaid coverage of Hepatitis C agents in Florida. It is required to access necessary medications for treating Hepatitis C under the Medicaid program.
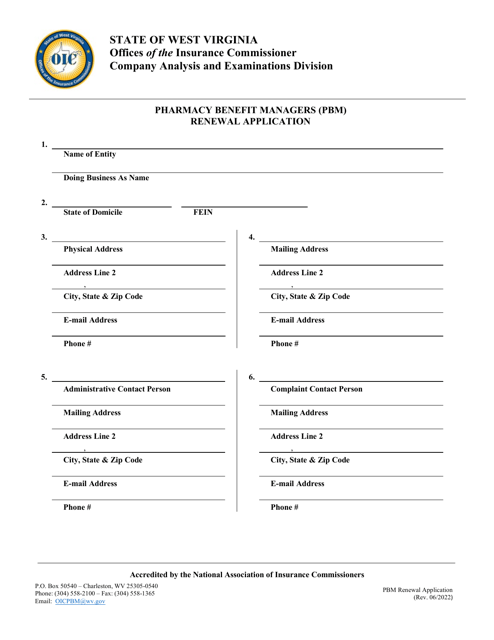
This Form is used for renewing the application for Pharmacy Benefit Managers (PBM) in West Virginia.
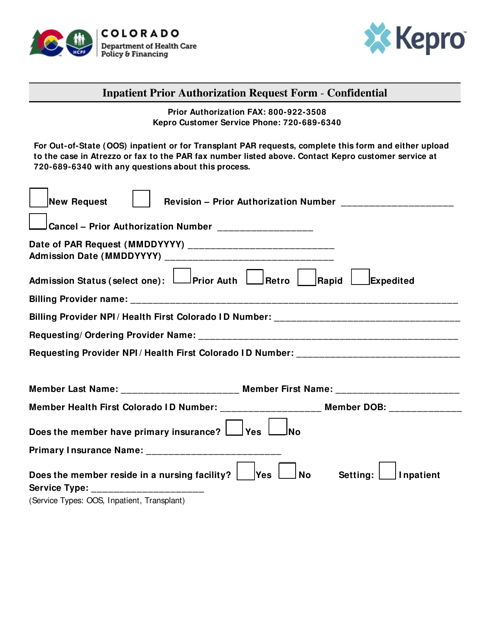
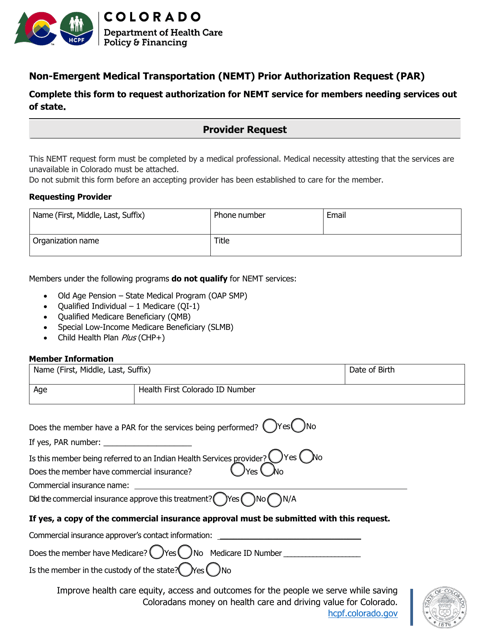
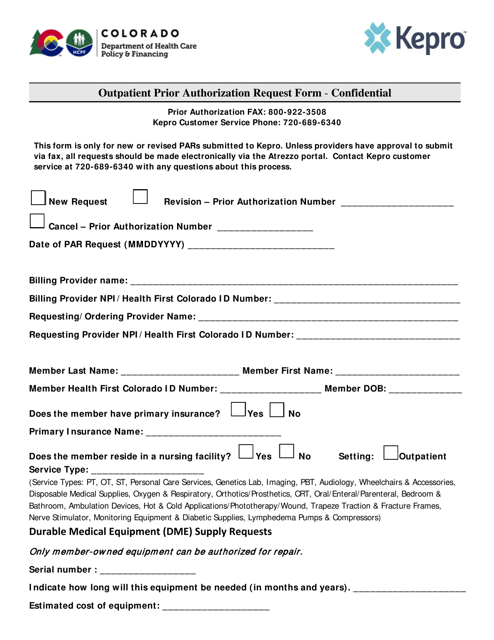
This document is used for requesting prior authorization for non-emergent medical transportation (NEMT) in the state of Colorado.
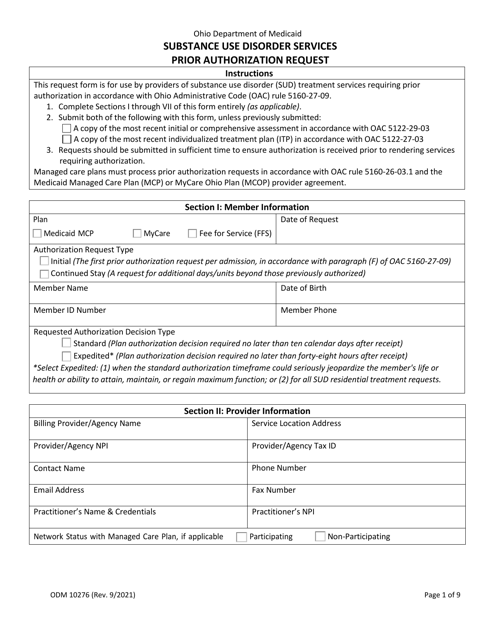
This form is used for requesting prior authorization for substance use disorder services in Ohio.
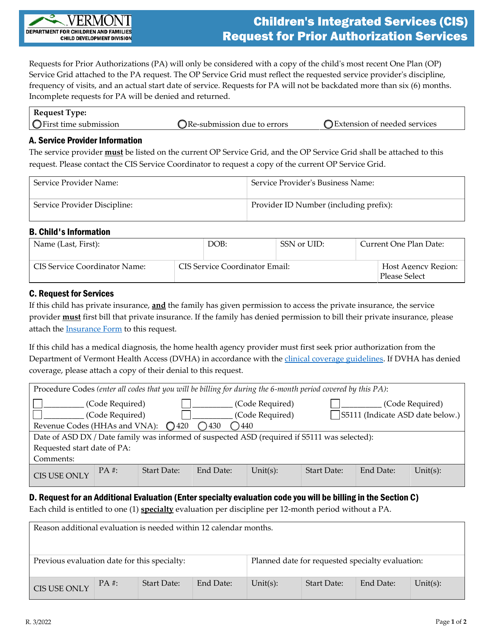
This document is a request for prior authorization services for the Children's Integrated Services (CIS) program in Vermont. It is used to seek approval for specific services and support for children.
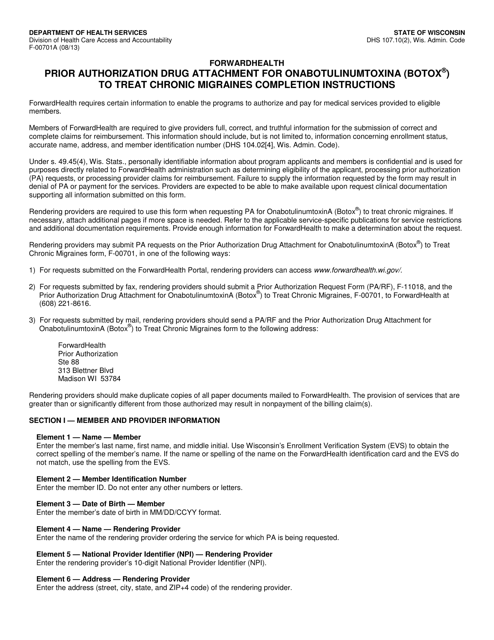
This Form is used for providing instructions for completing Form F-00701 for obtaining prior authorization for onabotulinumtoxina (Botox) treatment of chronic migraines in Wisconsin.
This document provides instructions for completing Form F-11308, which is used for requesting prior authorization or preferred drug list (Pa/Pdl) for cytokine and cell adhesion molecule (Cam) antagonist drugs for patients with rheumatoid arthritis (Ra) and polyarticular juvenile Ra in Wisconsin.
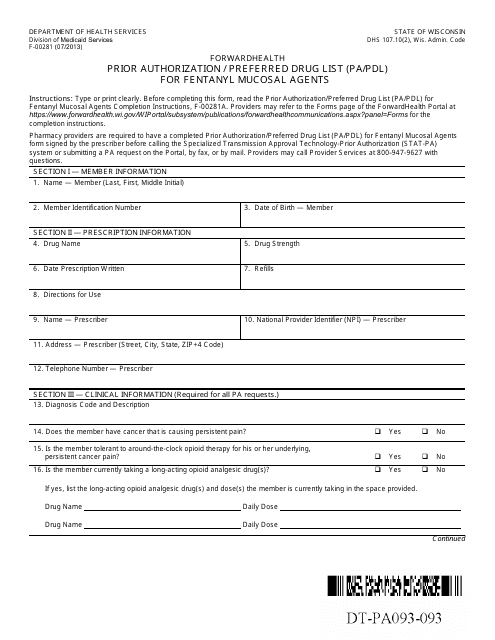
This document provides instructions for completing and submitting Form F-00281, which is used for prior authorization and preferred drug list for fentanyl mucosal agents in the state of Wisconsin.
This Form is used for obtaining prior authorization or preferred drug list (Pa/Pdl) for Proton Pump Inhibitor (Ppi) orally disintegrating tablets in Wisconsin. It provides instructions on how to complete the form and submit it for approval.
This Form is used for submitting a request for prior authorization for hearing instrument and audiological services in Wisconsin. It provides instructions on how to fill out the form and what documentation is required.
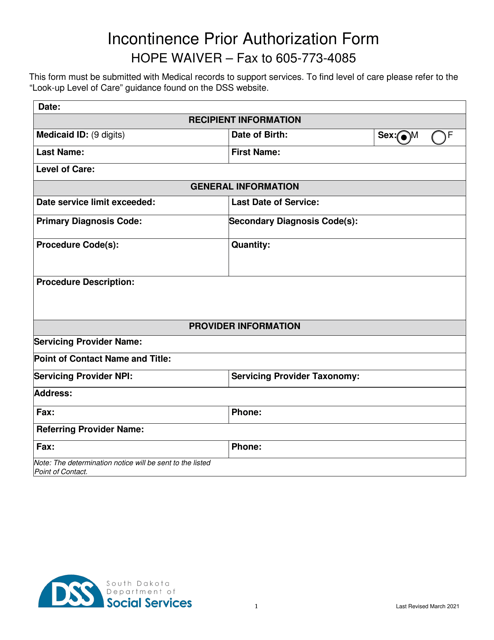
This form is used for obtaining prior authorization for the Incontinence Supply Hope Waiver in South Dakota. It is required for individuals who need assistance with incontinence supplies.
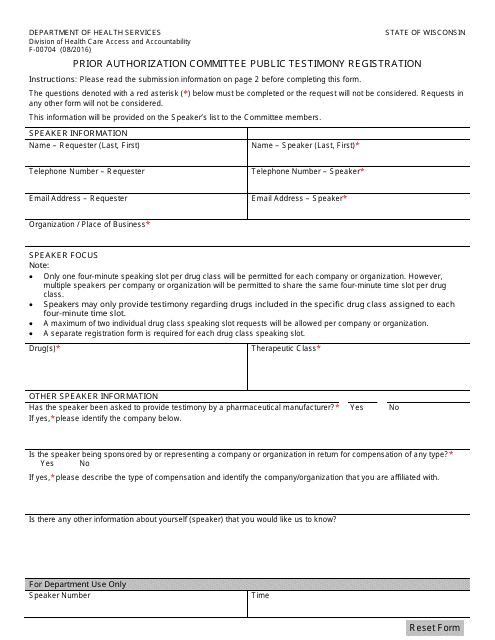
This form is used for registering to provide public testimony at a committee meeting in Wisconsin.
This form is used for prior authorization and preferred drug list for fentanyl mucosal agents in the state of Wisconsin.