Prior Authorization Templates
Documents:
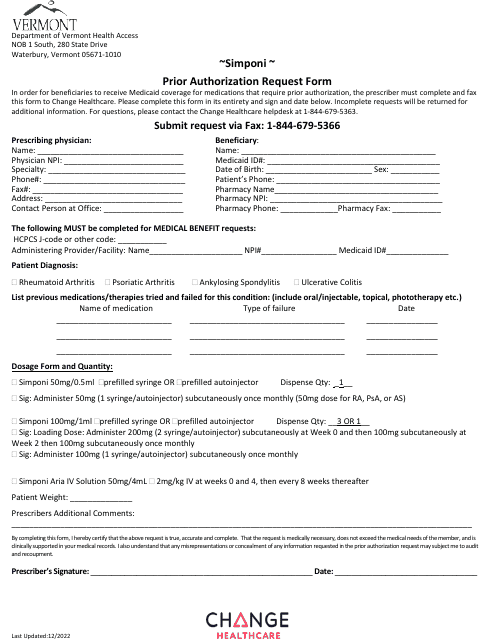
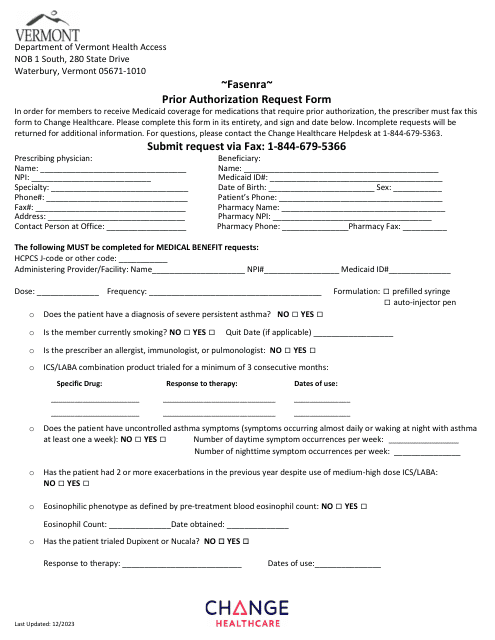
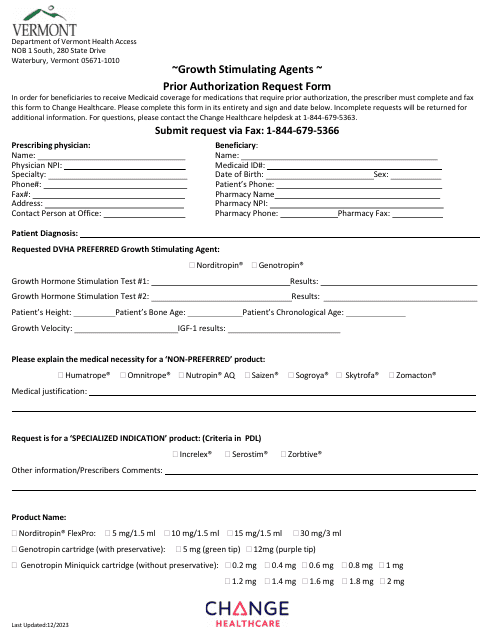
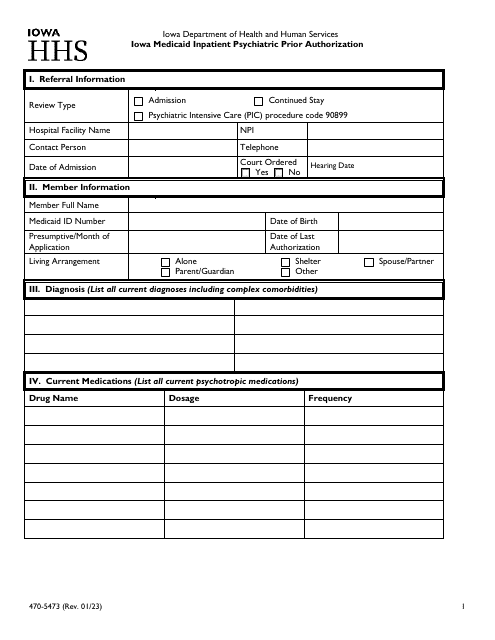
390
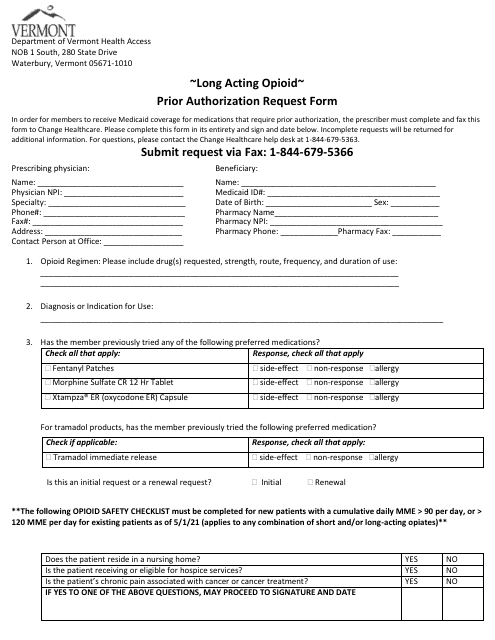
This Form is used for requesting prior authorization for long-acting opioids in the state of Vermont.
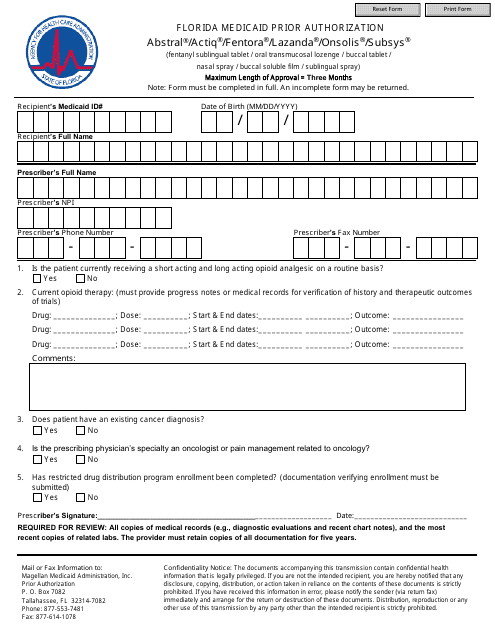
This Form is used for obtaining prior authorization for certain medications (Abstral, Actiq, Fentora, Lazanda, Onsolis, Subsys) under Florida Medicaid. Prior authorization is required to ensure that these medications meet the coverage criteria and are medically necessary for the patient.
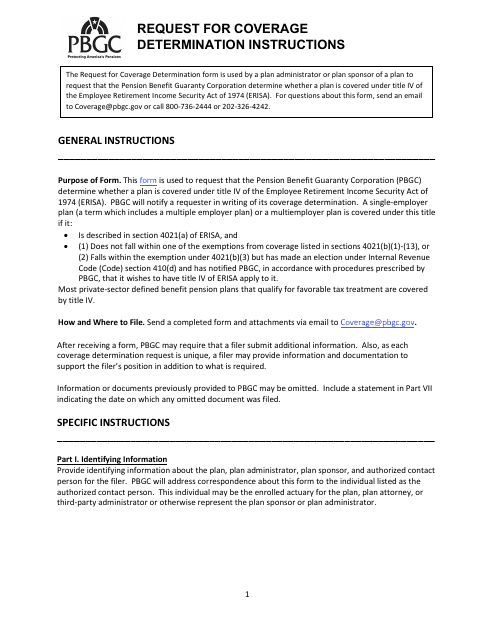
This document provides instructions on how to request a coverage determination.
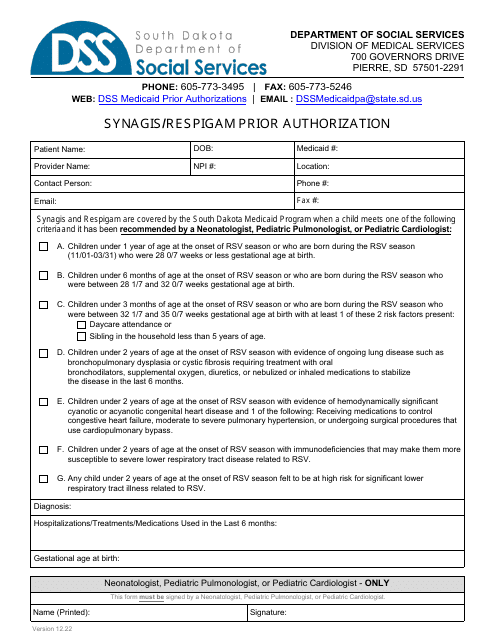
This form is used for obtaining prior authorization for the medications Synagis and Respigam in South Dakota.
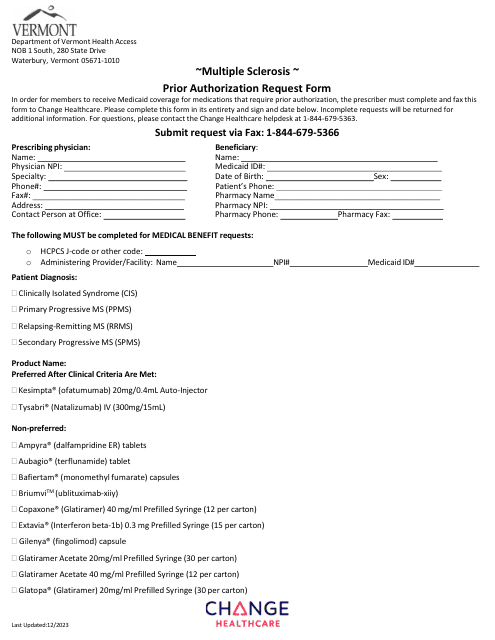
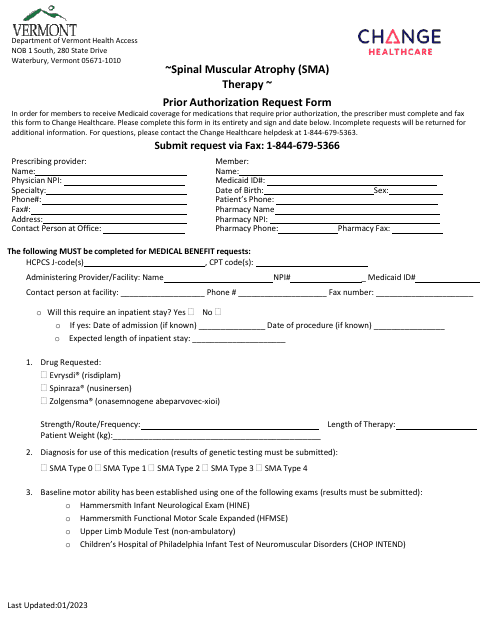
This Form is used for requesting prior authorization for Spinal Muscular Atrophy (SMA) therapy in Vermont.
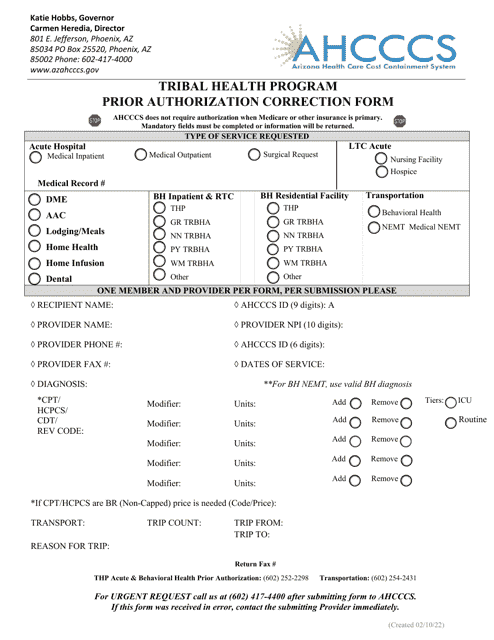
This form is used for making corrections to prior authorizations in the Tribal Health Program in Arizona.
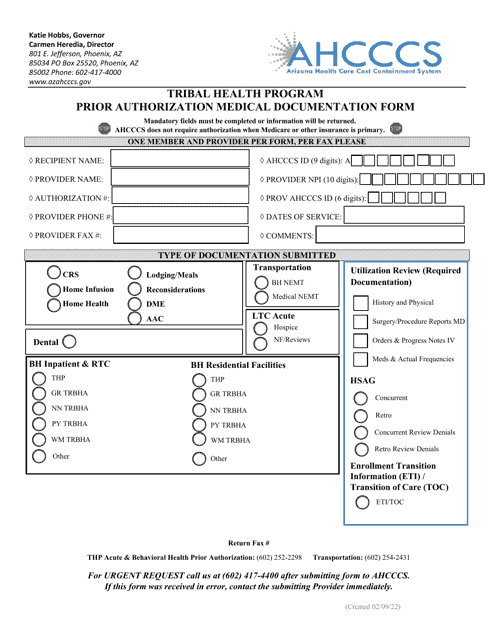
This Form is used for submitting medical documentation for prior authorization through the Tribal Health Program in Arizona.
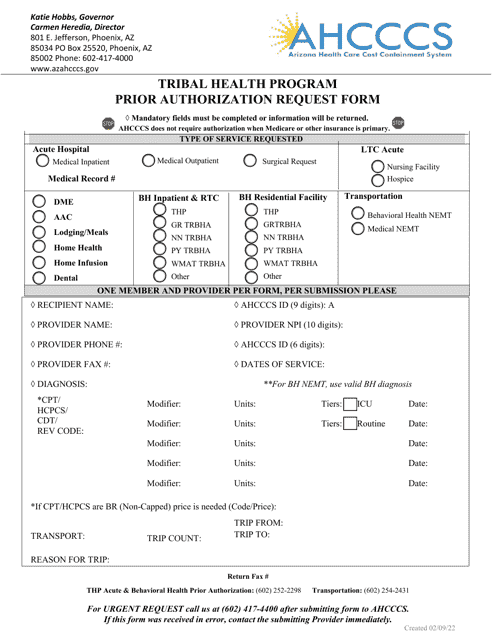
This form is used to request prior authorization for medical services under the Tribal Health Program in Arizona.
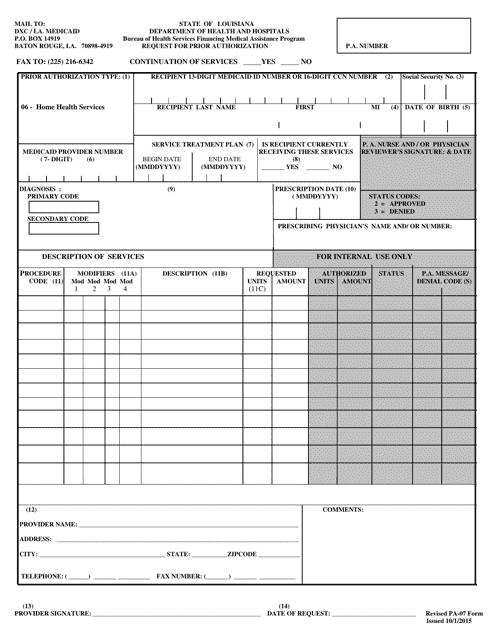
This form is used for requesting prior authorization for medical services in the state of Louisiana.
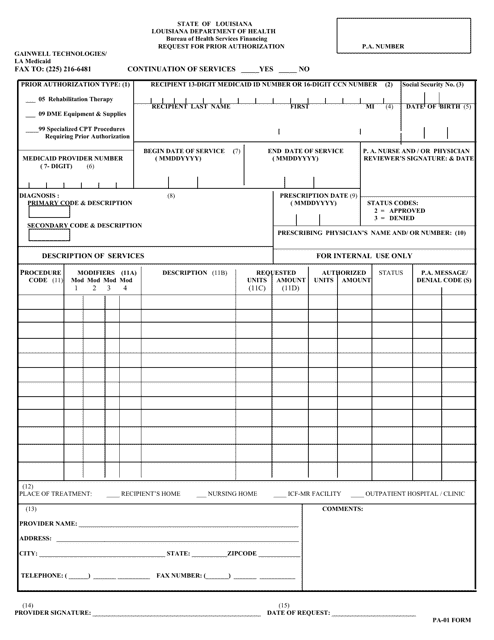
This form is used for requesting prior authorization for medical services in the state of Louisiana. It is important to complete this form in order to receive coverage for certain procedures or treatments.
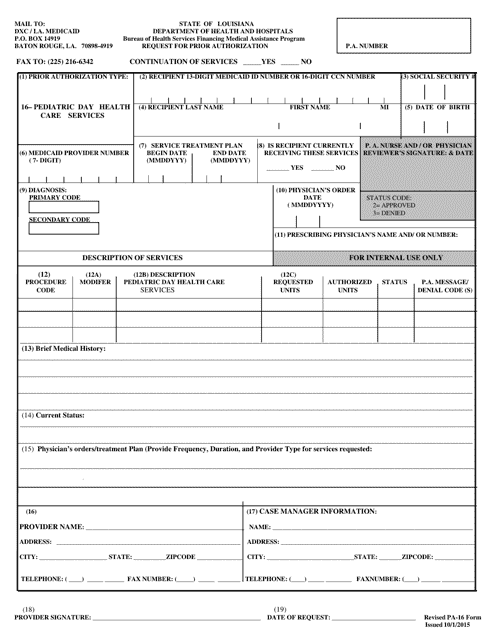
This Form is used for requesting authorization for pediatric day health care services in Louisiana.
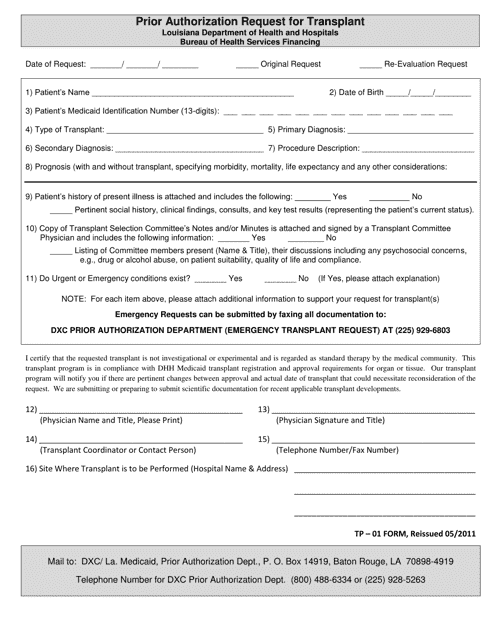
This form is used for submitting a prior authorization request for a transplant procedure in the state of Louisiana. It is necessary to obtain approval from the insurance provider before undergoing a transplant surgery.
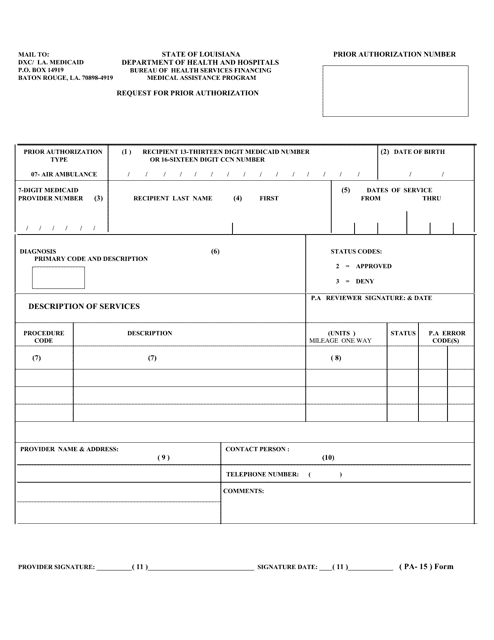
This form is used for residents of Louisiana to request prior authorization for air ambulance services. It is required to ensure coverage and payment for the services rendered.
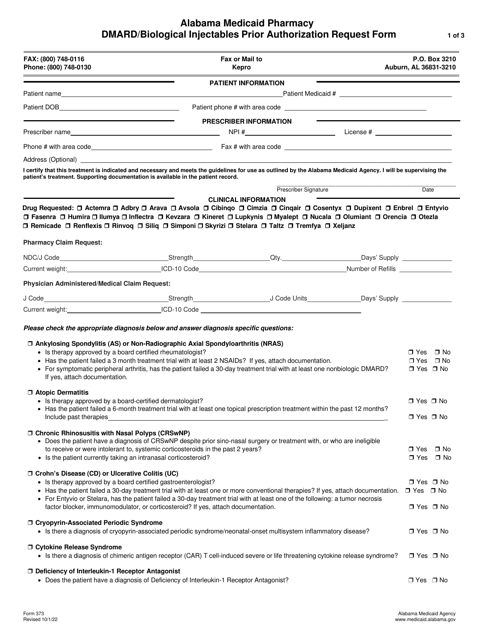
This form is used for requesting prior authorization for DMARD/biological injectables in the state of Alabama.