Prior Authorization Templates
Documents:
390
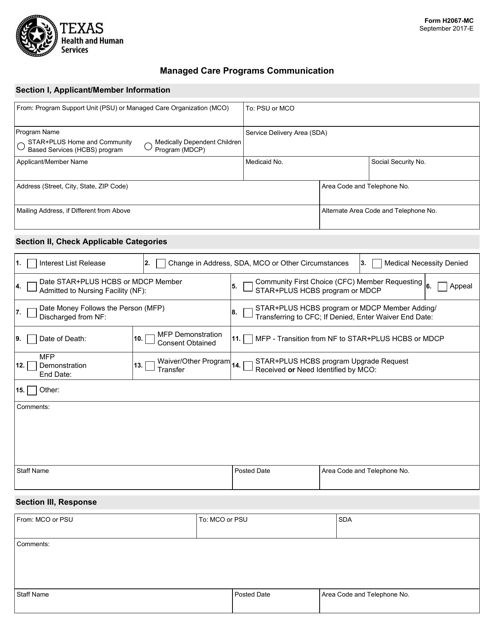
This form is used for communicating with managed care programs in Texas. It is used to provide information or request assistance related to healthcare services.
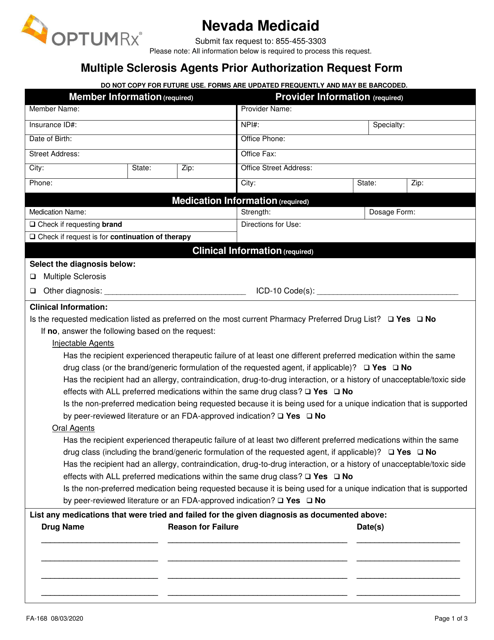
This form is used for requesting prior authorization for multiple sclerosis agents in Nevada.
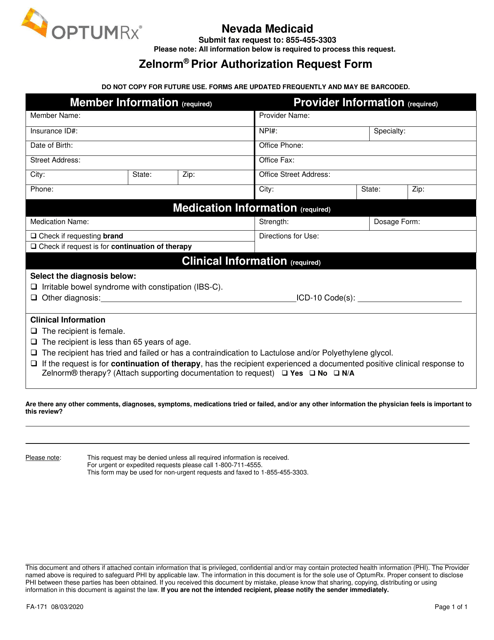
This Form is used for requesting prior authorization for the medication Zelnorm in the state of Nevada.
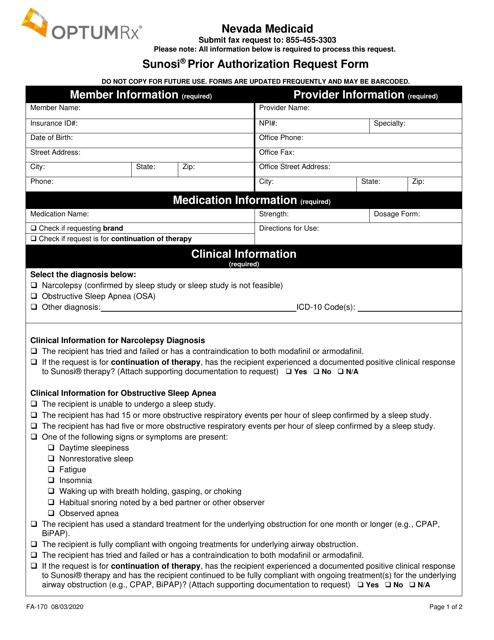
This Form is used for requesting prior authorization for the medication Sunosi in the state of Nevada.
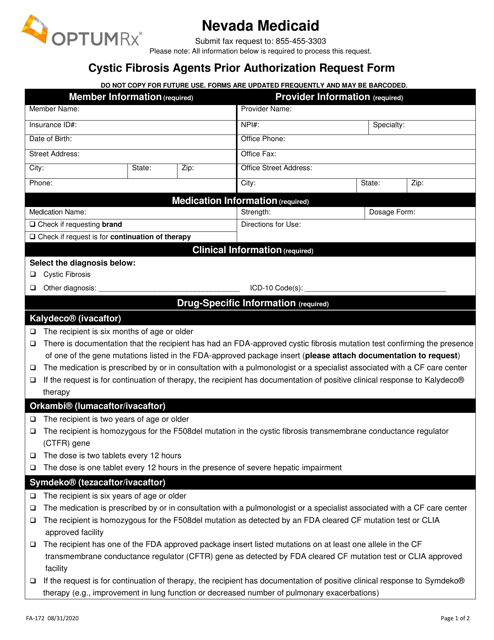
This Form is used for requesting prior authorization for Cystic Fibrosis agents in Nevada.
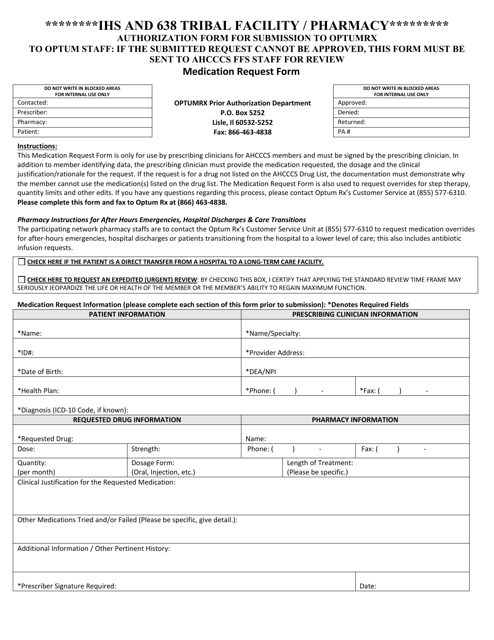
This Form is used for obtaining prior authorization for medications at IHS and 638 Tribal Facilities/Pharmacies in Arizona.
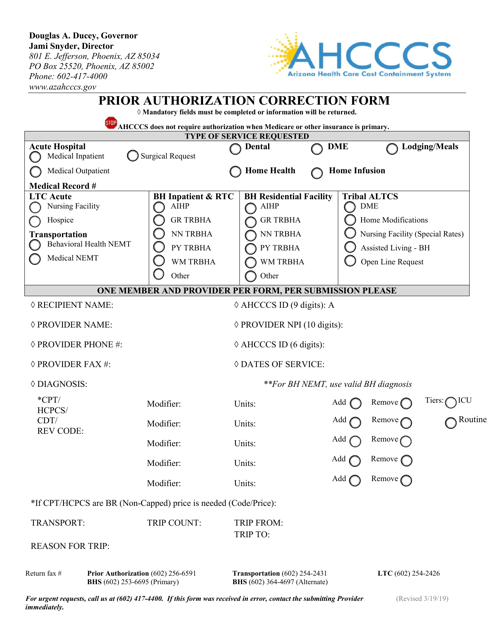
This Form is used for correcting prior authorization information in Arizona.
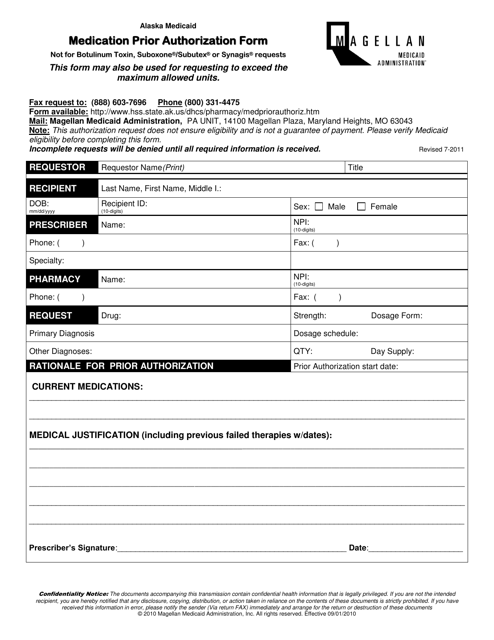
This Form is used for requesting prior authorization for medications in the state of Alaska.
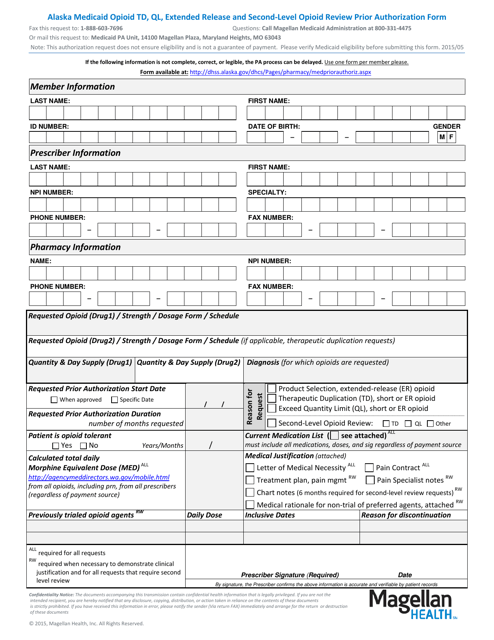
This form is used for Medicaid in Alaska to request prior authorization for certain opioid medications, including extended-release formulations. It is used for second-level review of opioid prescriptions to ensure appropriate use and minimize potential abuse.
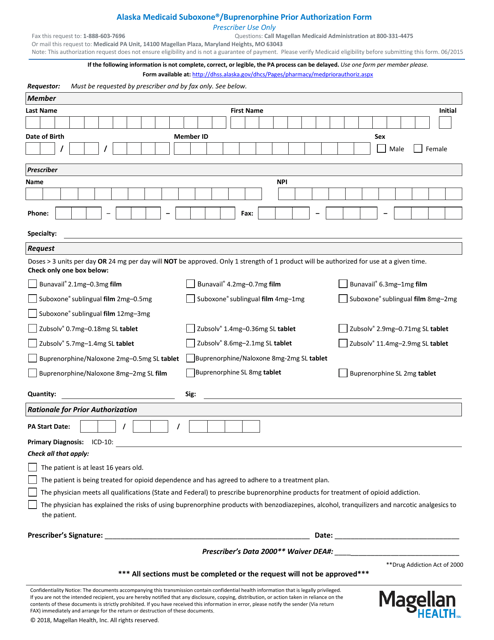
This form is used for obtaining prior authorization for Suboxone/Buprenorphine through Alaska Medicaid.
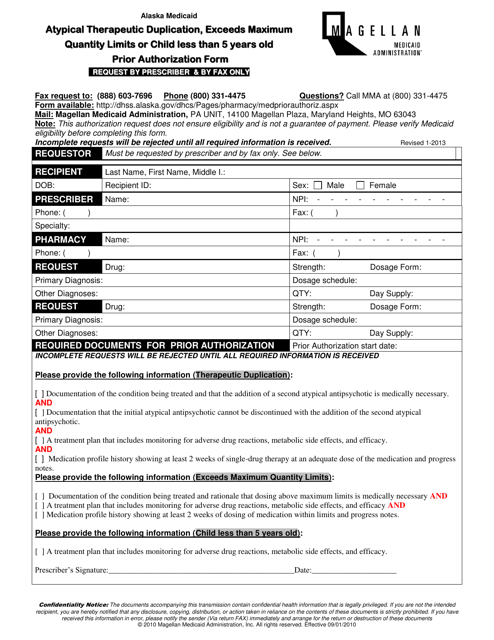
This document is a Prior Authorization Form for Atypical Therapeutic Duplication, Exceeds Maximum Quantity Limits, or Child Less Than 5 Years Old in Alaska. It is used to request permission for medication that may be duplicated or exceeds quantity limits, or for children under 5 years old.
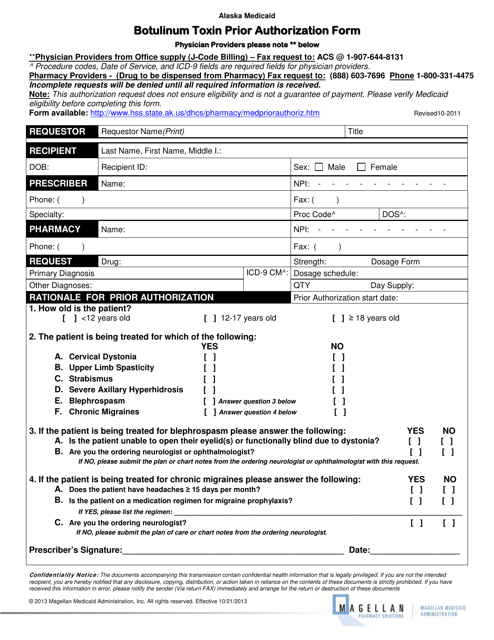
This form is used for obtaining prior authorization for the use of Botulinum Toxin in Alaska.
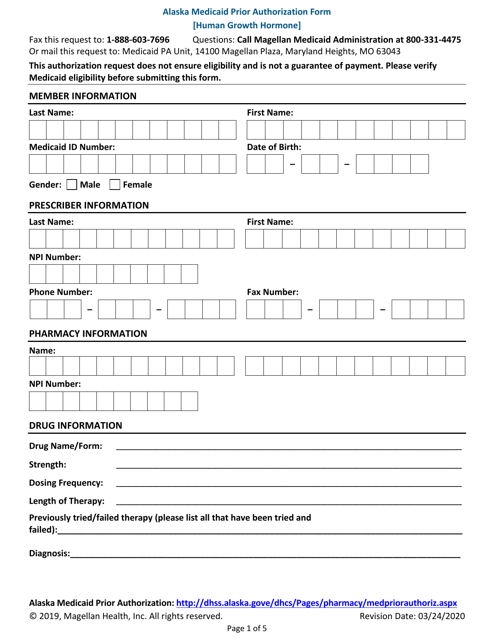
This form is used for prior authorization of human growth hormone under the Alaska Medicaid program.
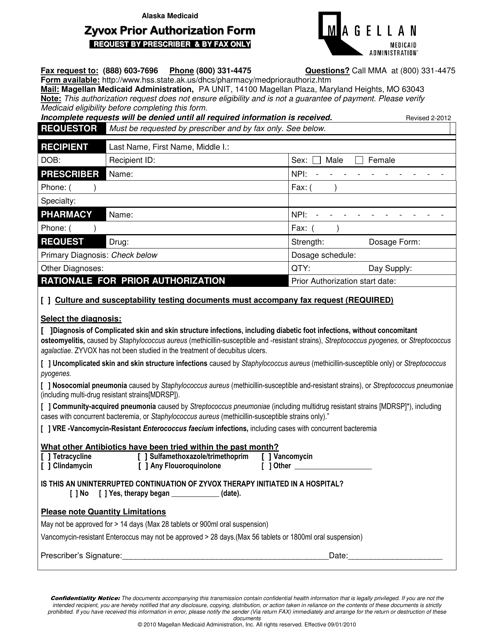
This Form is used for obtaining prior authorization for the medication Zyvox in Alaska.
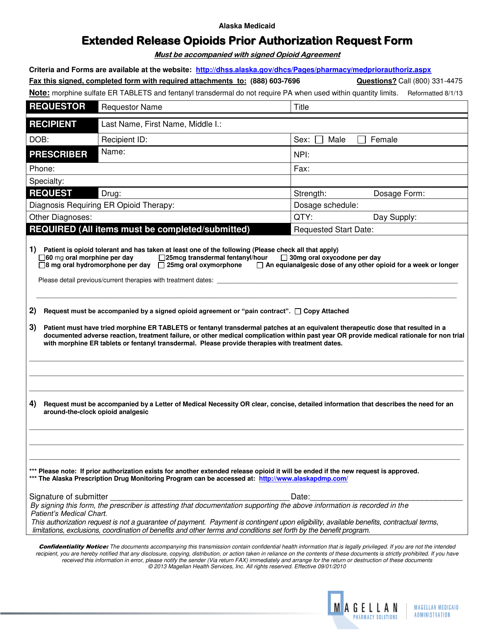
This form is used for requesting prior authorization for extended release opioids in the state of Alaska.
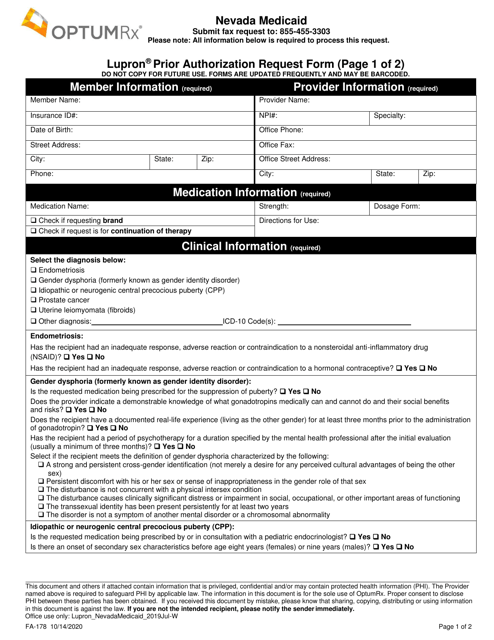
This form is used for requesting prior authorization for Lupron medication in Nevada.
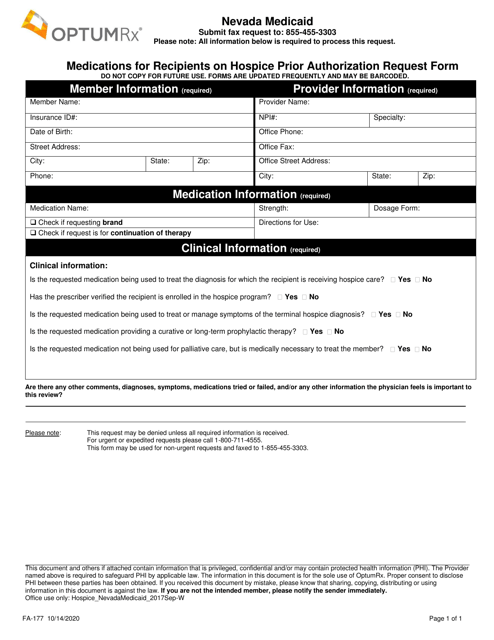
This Form is used for requesting prior authorization for medications for recipients on hospice in Nevada.
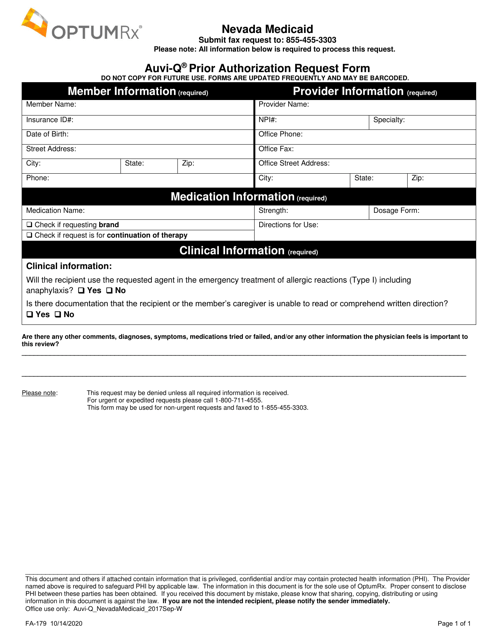
This Form is used for requesting prior authorization for Auvi-Q medication in the state of Nevada.
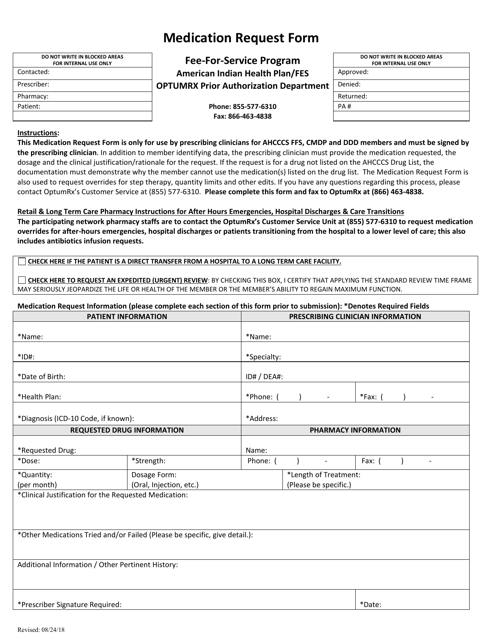
This form is used for requesting prior authorization for medications in the Arizona Fee-for-Service Drug program.
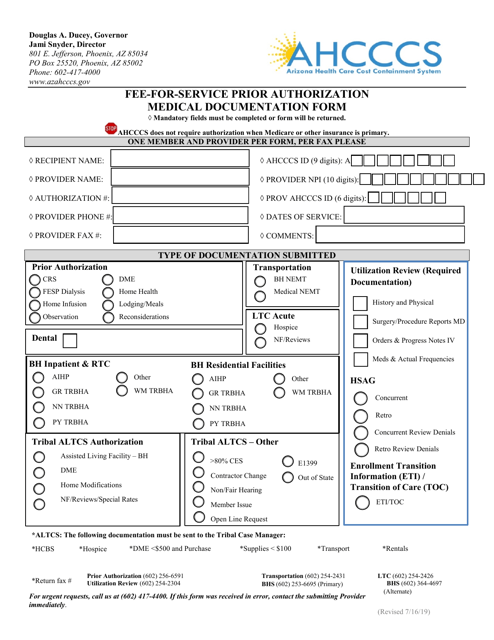
This Form is used for requesting prior authorization for fee-for-service medical services in Arizona. It requires medical documentation to support the need for the requested service.
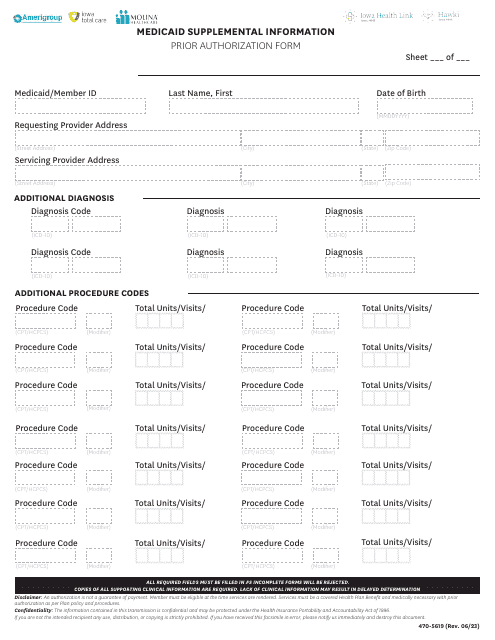
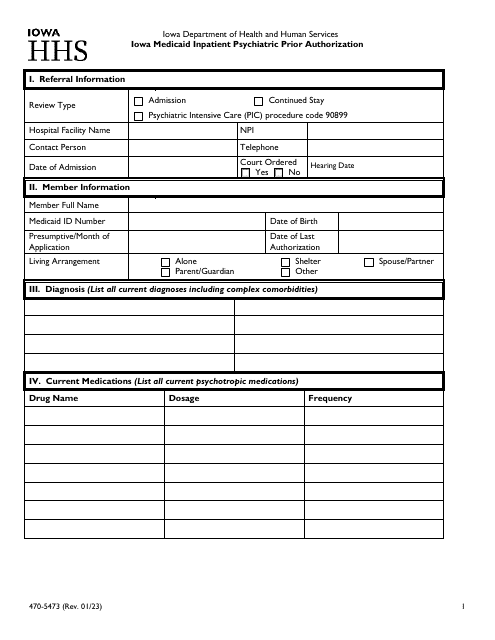
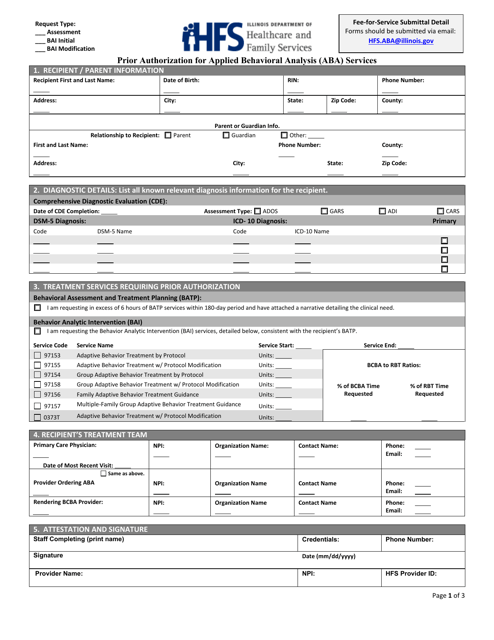
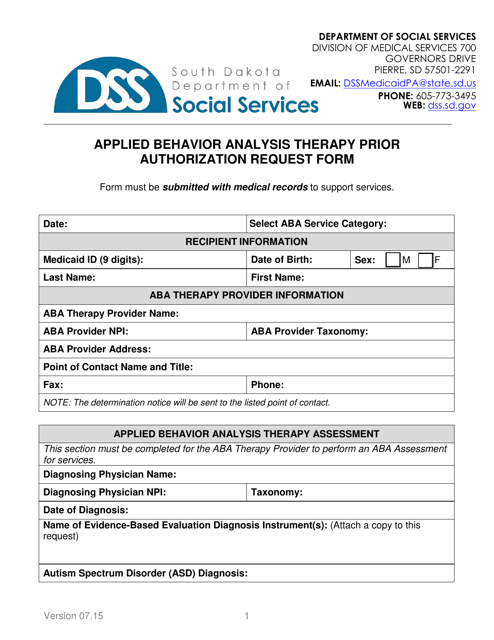
This form is used for obtaining prior authorization for Applied Behavioral Analysis (ABA) services in the state of Illinois. ABA is a type of therapy that helps individuals with autism spectrum disorder improve their social, communication, and behavioral skills. Prior authorization is required to ensure coverage and reimbursement for ABA services.
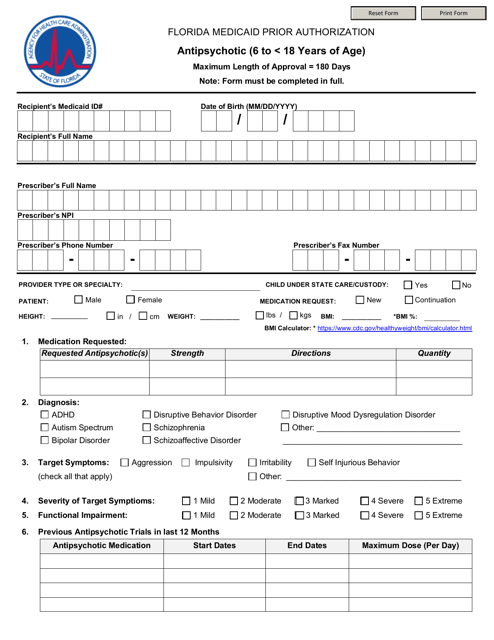
This form is used for requesting prior authorization for antipsychotic medications for children between the ages of 6 and 18 in Florida.
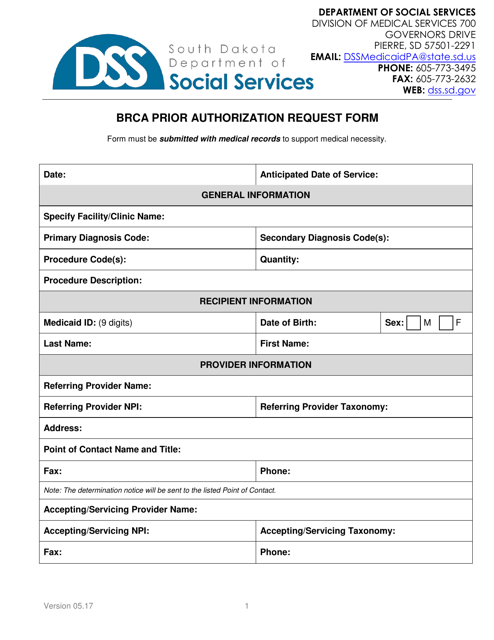
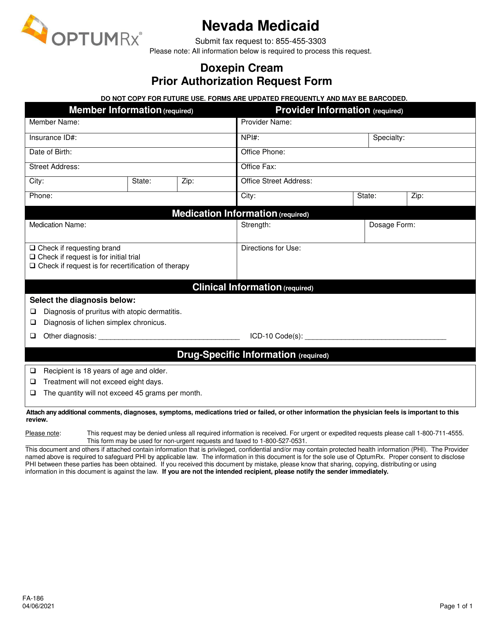
This form is used for requesting prior authorization for Doxepin Cream in the state of Nevada. It is necessary to complete this form in order to obtain coverage for this medication.
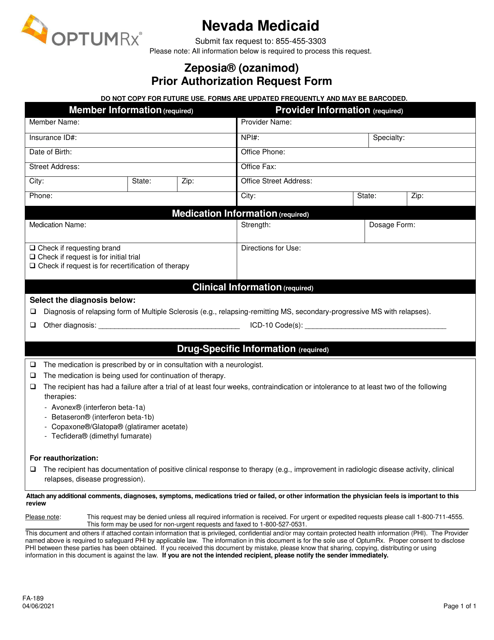
This form is used for requesting prior authorization for the medication Zeposia (Ozanimod) in Nevada.
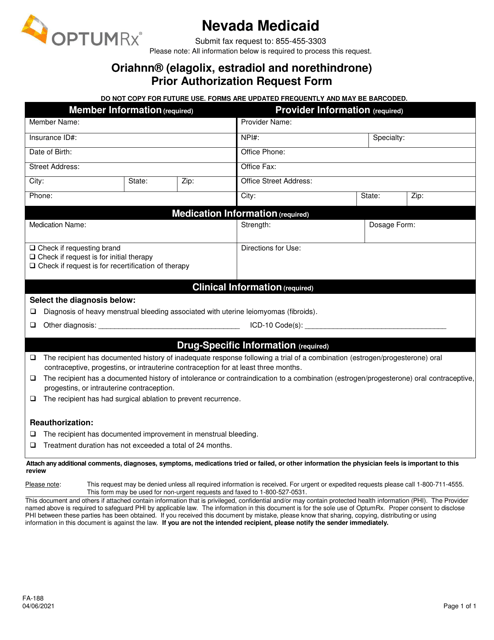
This form is used for requesting prior authorization for Oriahnn (Elagolix, Estradiol, and Norethindrone) medication in Nevada.
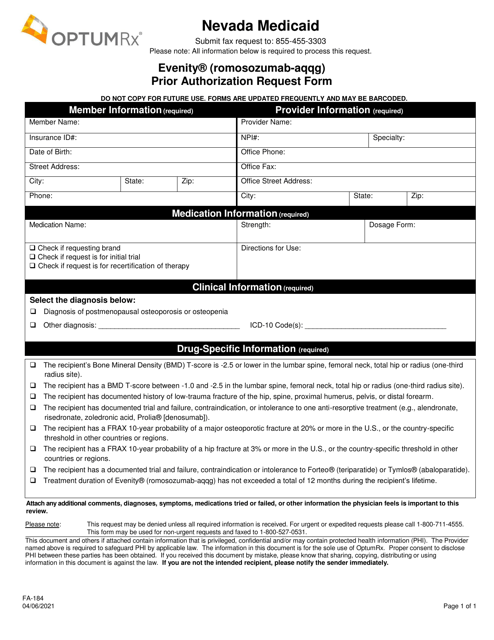
This form is used for submitting a prior authorization request for Evenity (Romosozumab-Aqqg) in the state of Nevada.
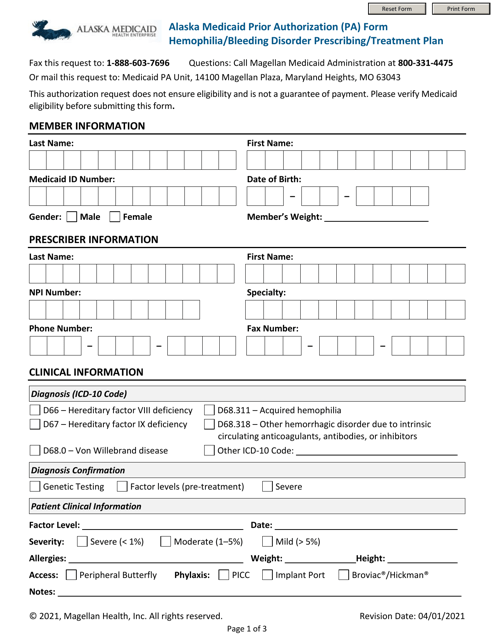
This Form is used for requesting prior authorization for hemophilia or bleeding disorder treatment plans under Alaska Medicaid.
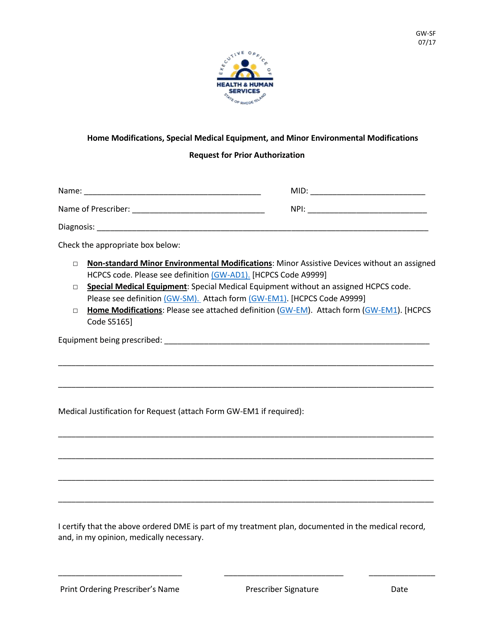
This Form is used for residents of Rhode Island to request prior authorization for home modifications, special medical equipment, and minor environmental modifications.
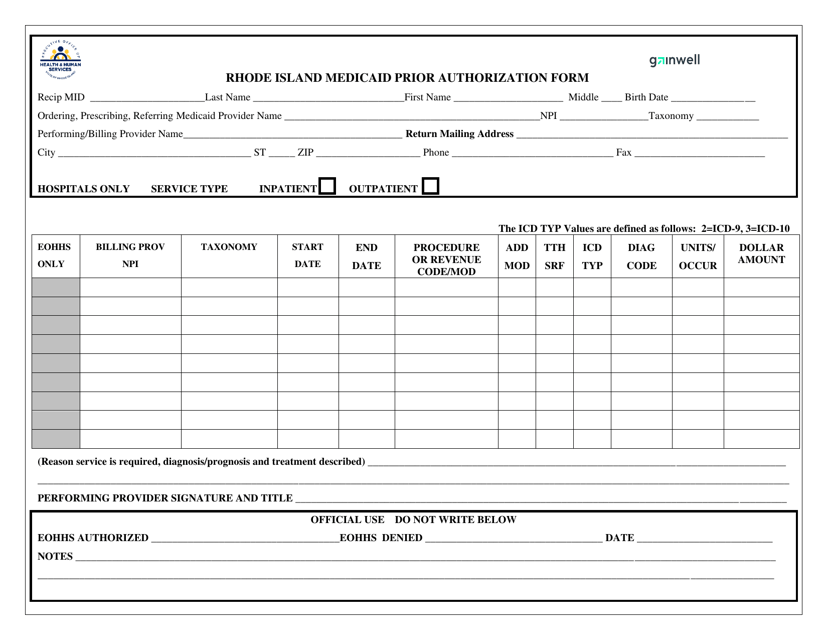
This form is used for obtaining prior authorization for Medicaid services in Rhode Island. It helps ensure that necessary medical treatments are approved and covered by Medicaid.
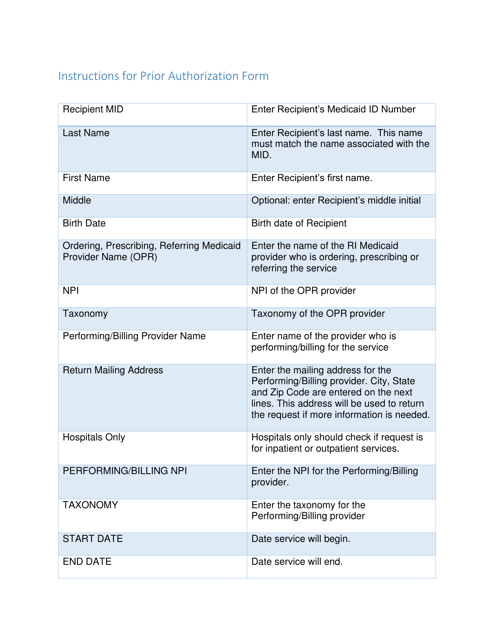
This document provides instructions for completing the Rhode Island Medicaid Prior Authorization Form. It is used to request approval for specific medical services or treatments before they can be covered by Medicaid in Rhode Island.