Prior Authorization Templates
Documents:
390
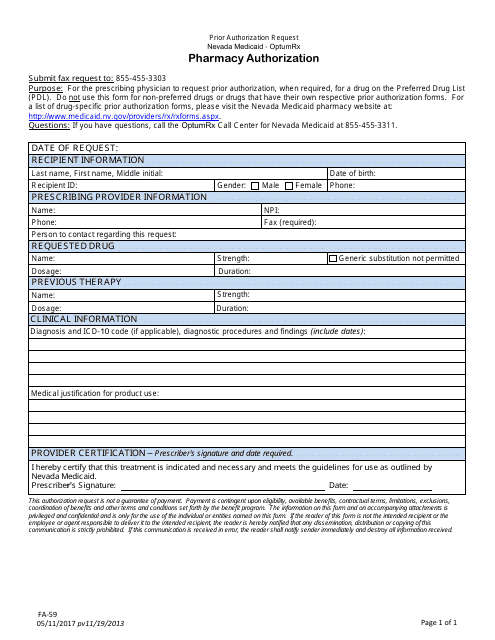
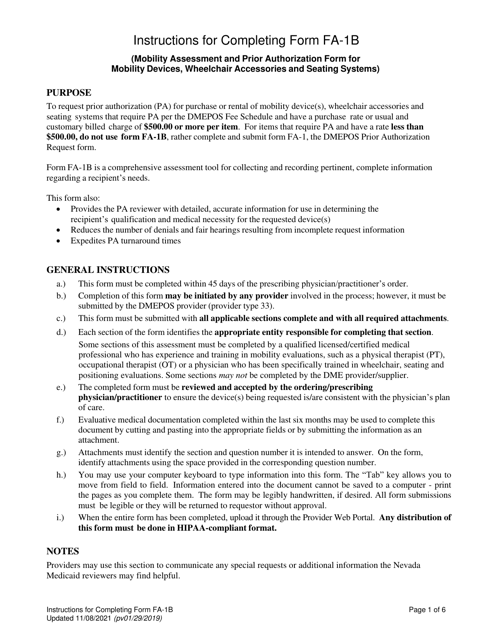
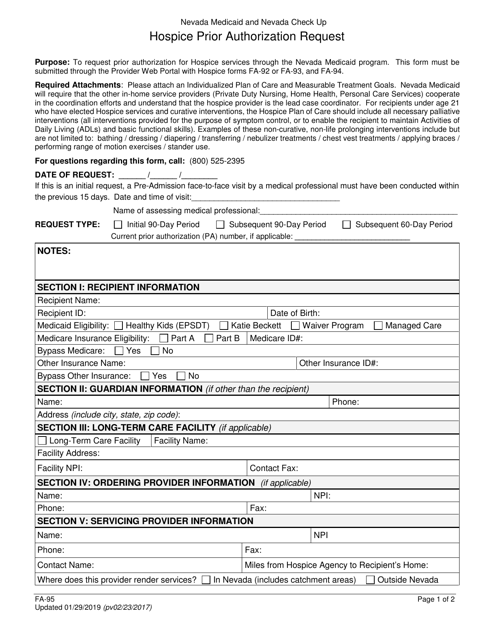
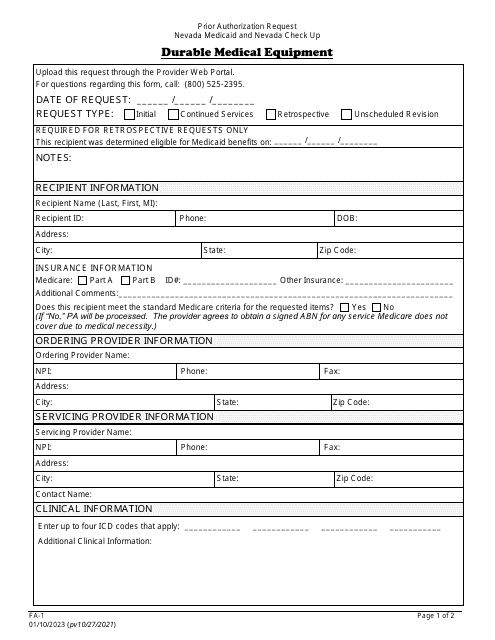
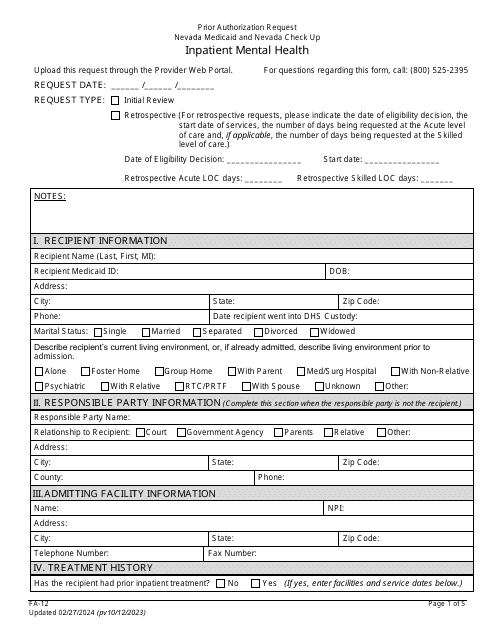
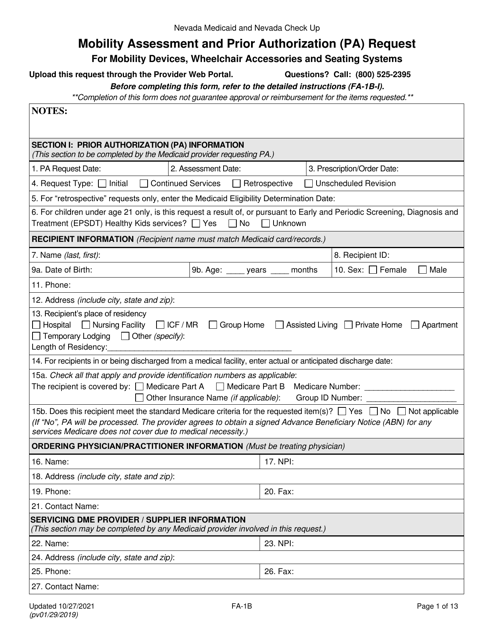
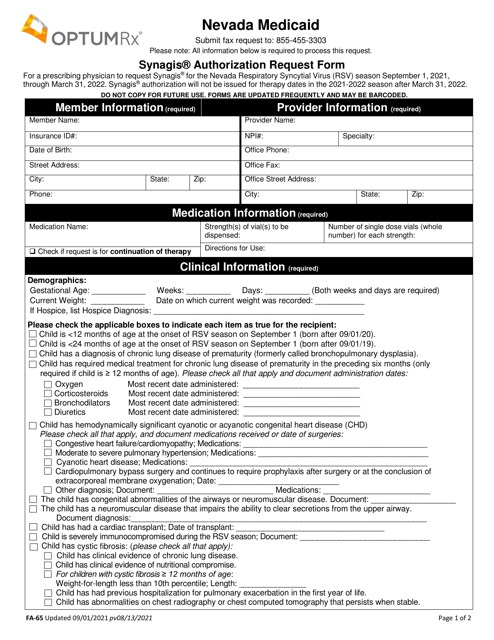
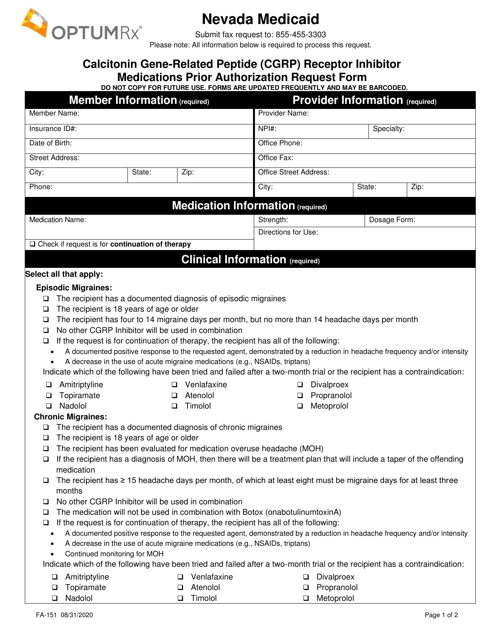
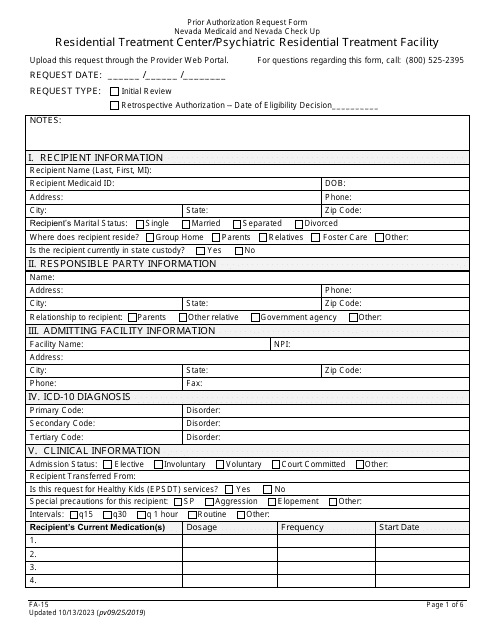
This Form is used for prior authorization of medical services in Nevada. It allows patients to request coverage for certain treatments or procedures.
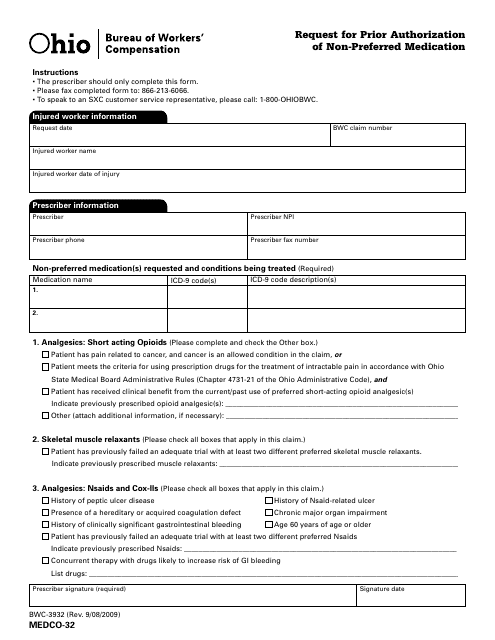
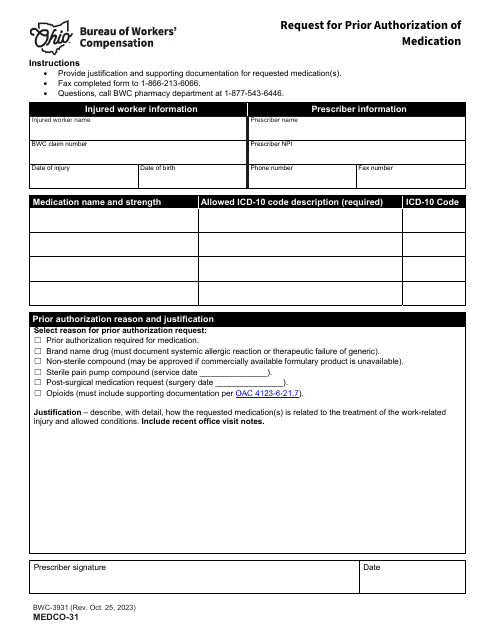
This form is used for requesting prior authorization of non-preferred medication in the state of Ohio. It allows individuals to submit a request to their health insurance provider for coverage of a medication that is not on their preferred drug list.
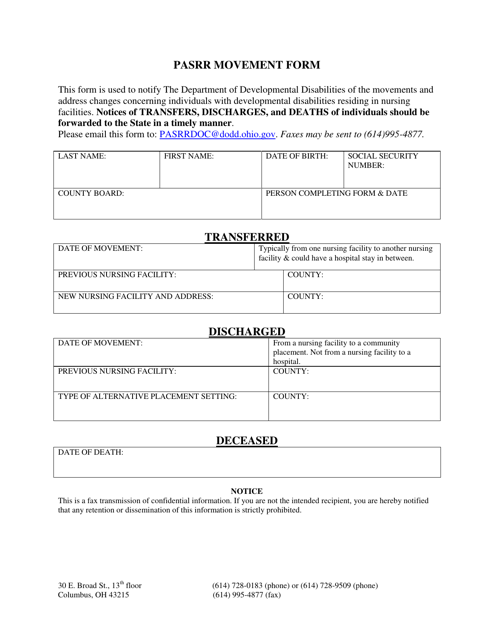
This Form is used for the Pasrr Movement Program in the state of Ohio. The Pasrr Movement Program aims to assess the need for specialized services for individuals with mental health illnesses and developmental disabilities. This form helps in the identification and coordination of appropriate services for individuals in Ohio.
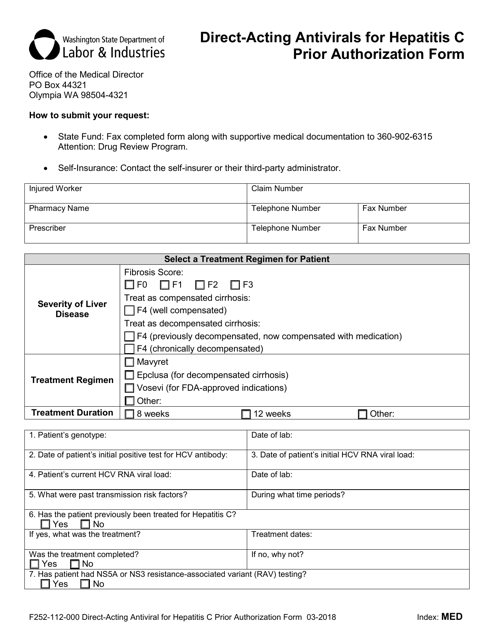
This form is used for obtaining prior authorization for direct-acting antiviral medication for the treatment of Hepatitis C in the state of Washington.
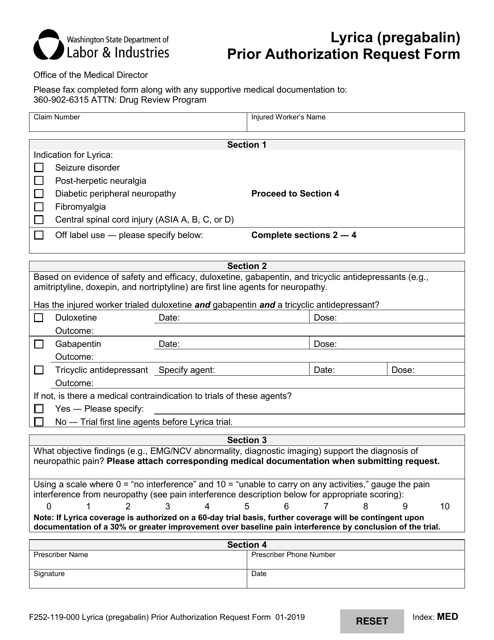
This form is used for requesting prior authorization for the medication Lyrica (Pregabalin) in the state of Washington.
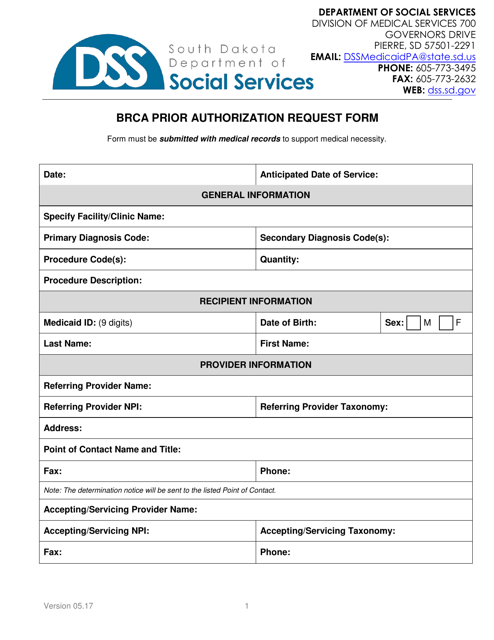
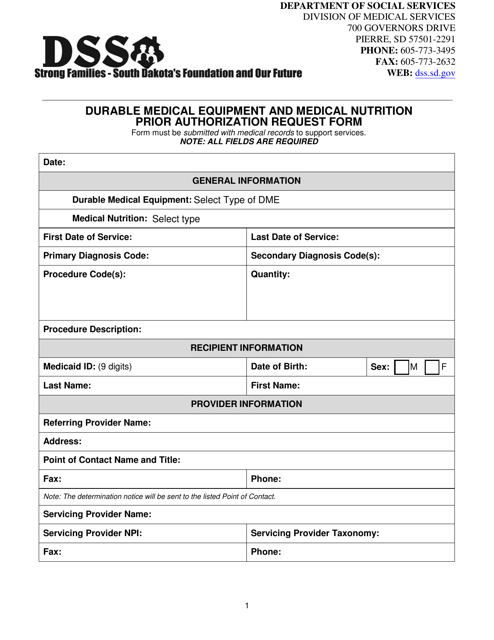
This Form is used for requesting prior authorization for durable medical equipment and medical nutrition in South Dakota.
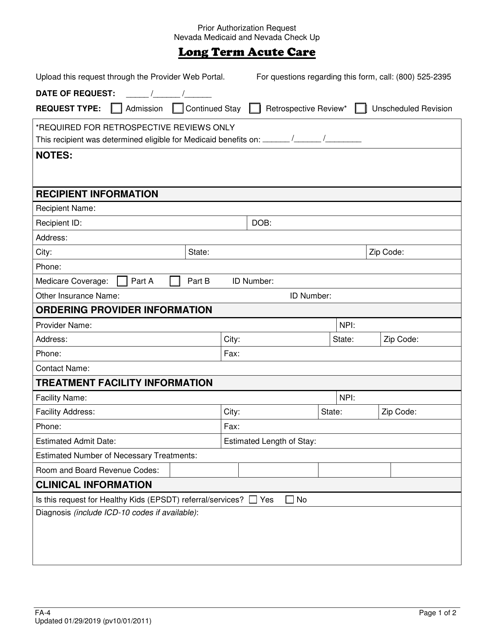
This Form is used for requesting prior authorization for long-term acute care in Nevada.
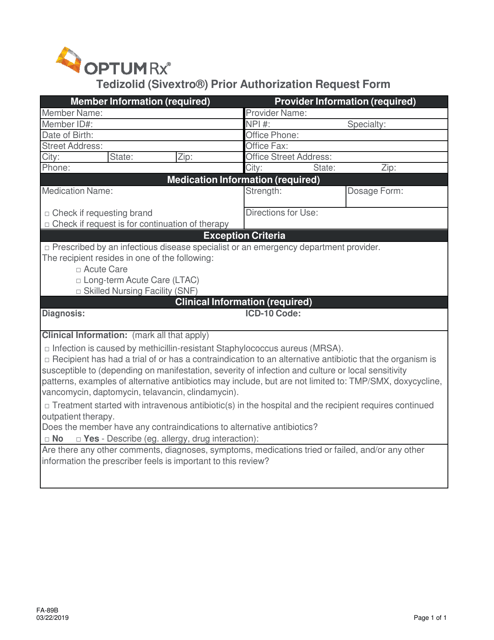
This form is used for requesting prior authorization for the medication Tedizolid (Sivextro) in the state of Nevada.
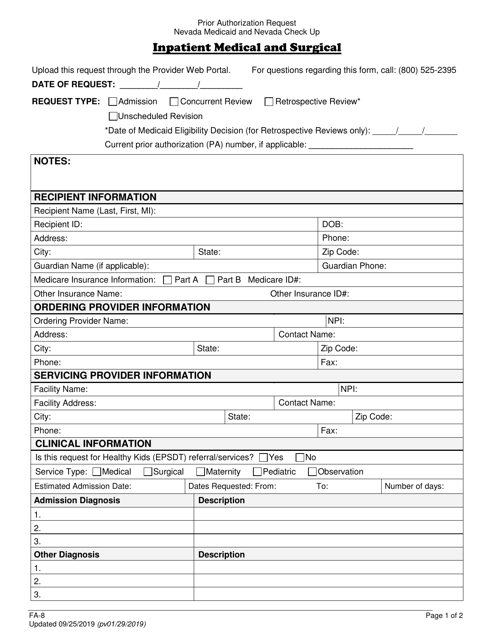
This form is used for requesting prior authorization for inpatient medical/surgical services in Nevada.
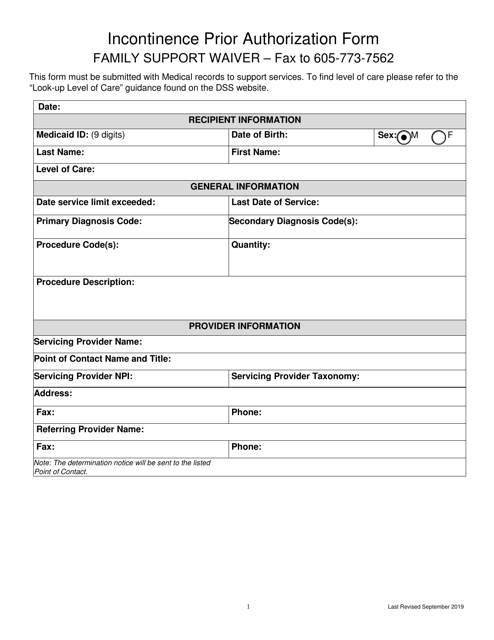
This form is used for requesting prior authorization for the Incontinence Supply Family Support 360 Waiver program in South Dakota.
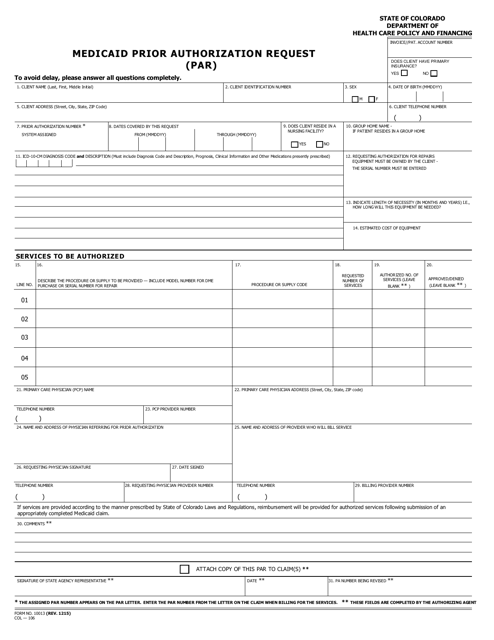
This form is used for submitting a prior authorization request for Medicaid services in Colorado.
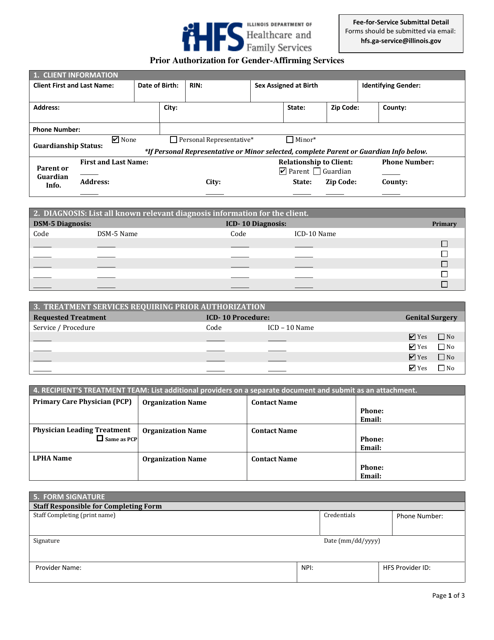
This Form is used for obtaining prior authorization in Illinois for gender-affirming services. It is necessary for individuals seeking these services to complete this form in order to receive coverage from their insurance provider.
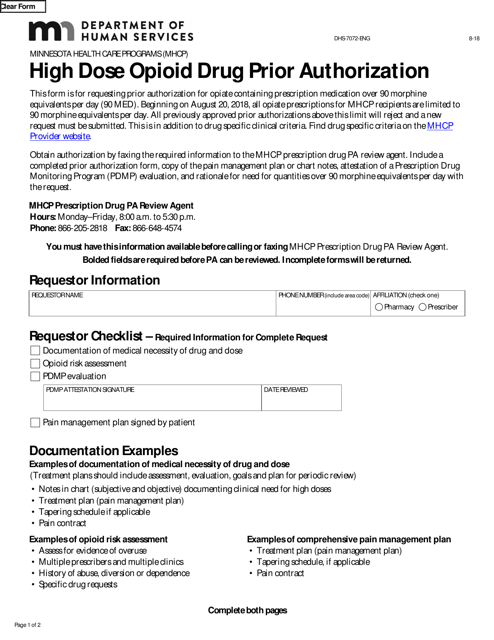
This form is used for requesting prior authorization for high dose opioid drugs in the state of Minnesota.
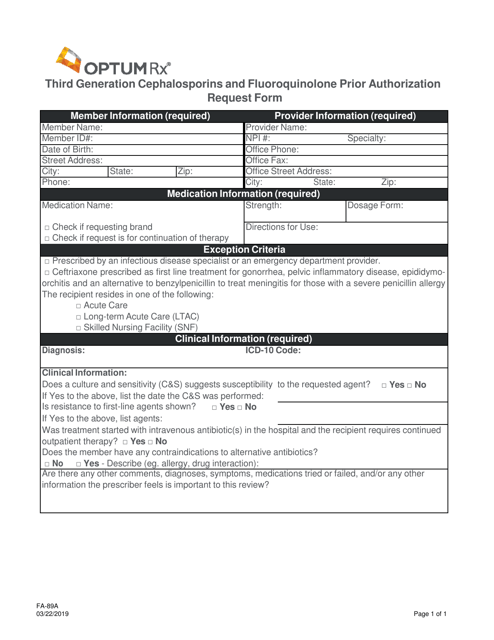
This form is used for requesting prior authorization for the use of third generation cephalosporins and fluoroquinolone medications in Nevada.
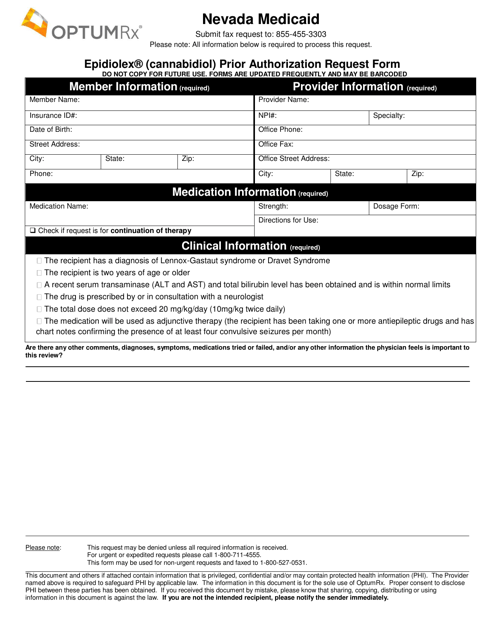
This form is used for requesting prior authorization for Epidiolex (Cannabidiol) medication in Nevada.
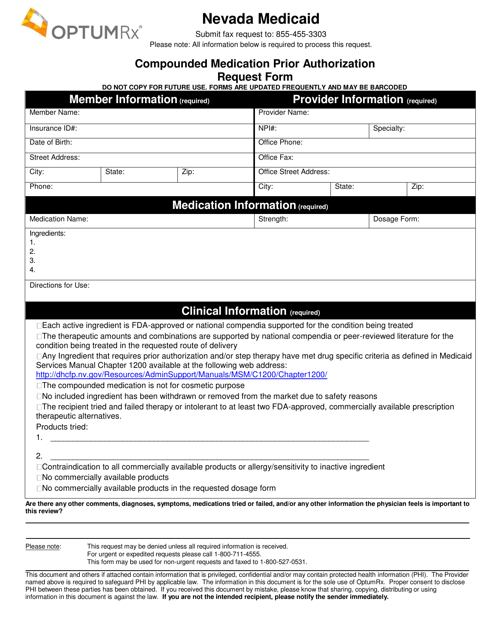
This form is used for requesting prior authorization for compounded medication in Nevada.
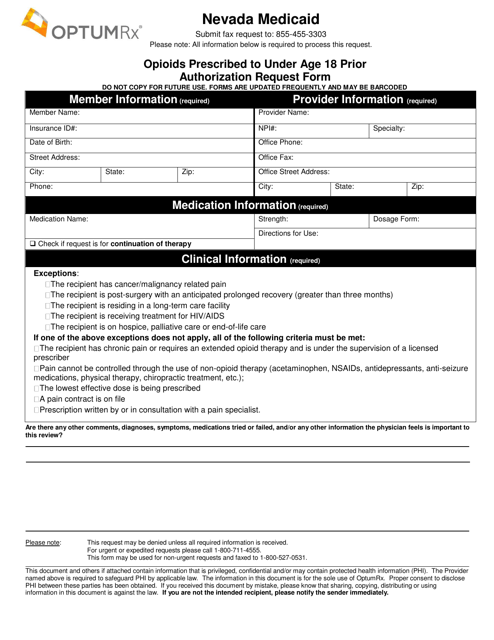
This Form is used for requesting prior authorization for prescribing opioids to individuals under the age of 18 in Nevada.
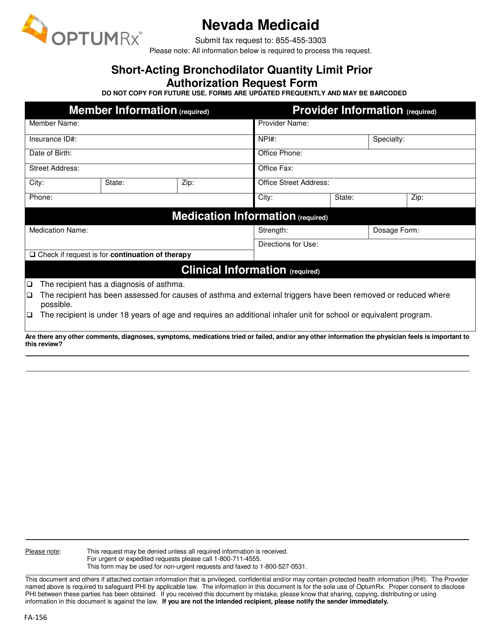
This form is used for requesting prior authorization for a specific quantity limit of a short-acting bronchodilator medication in Nevada.
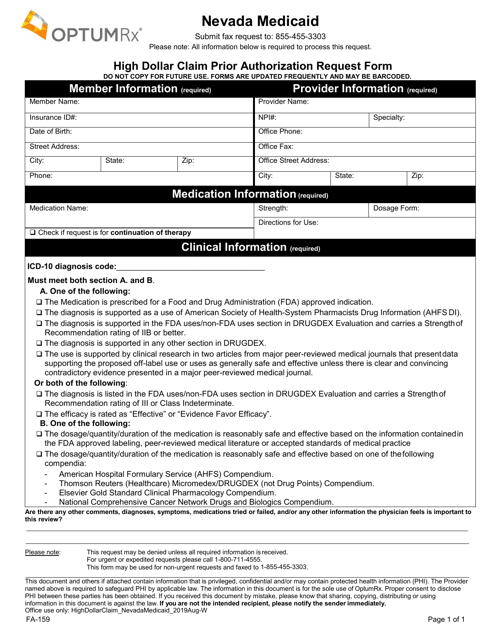
This form is used for requesting prior authorization for high dollar claims in Nevada. It is designed to ensure that the claim meets specific criteria before it is approved for payment.
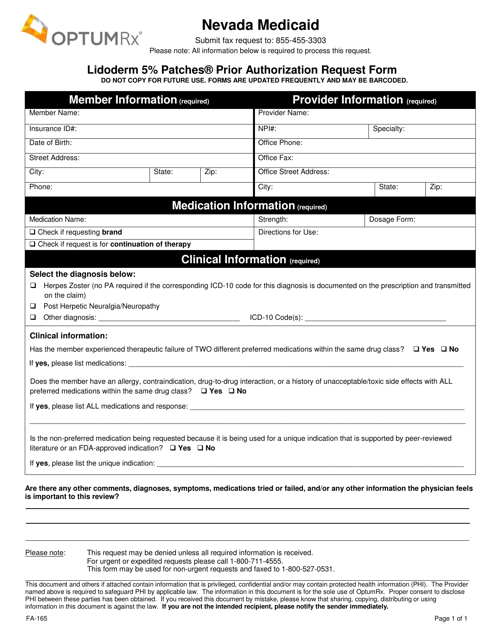
This form is used for requesting prior authorization for Lidoderm 5% Patches in Nevada.
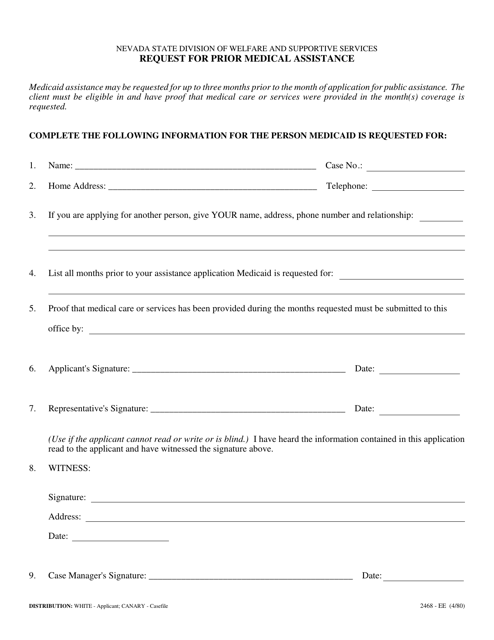
This form is used for requesting prior medical assistance in the state of Nevada.
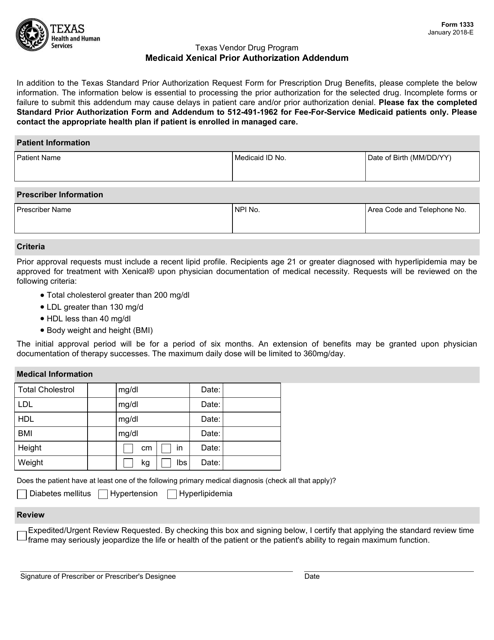
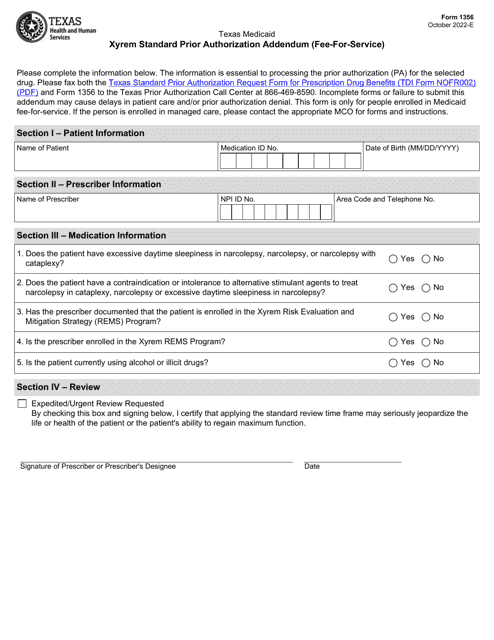
This form is used for adding a prior authorization addendum for the Medicaid program in Texas specifically for Xenical medication.
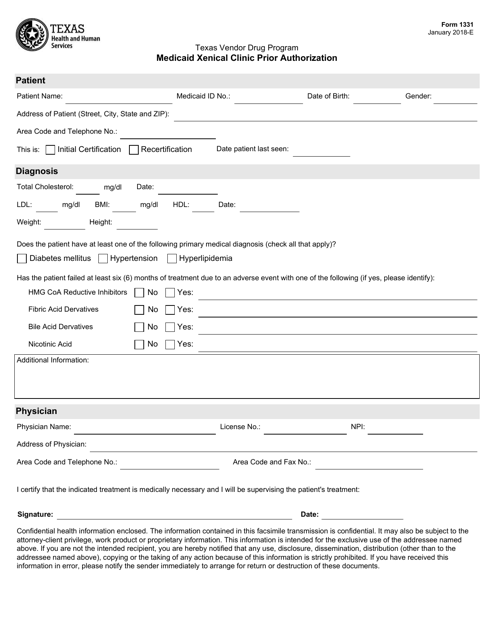
This form is used for Medicaid beneficiaries in Texas who need prior authorization for the prescription medication Xenical at a clinic.
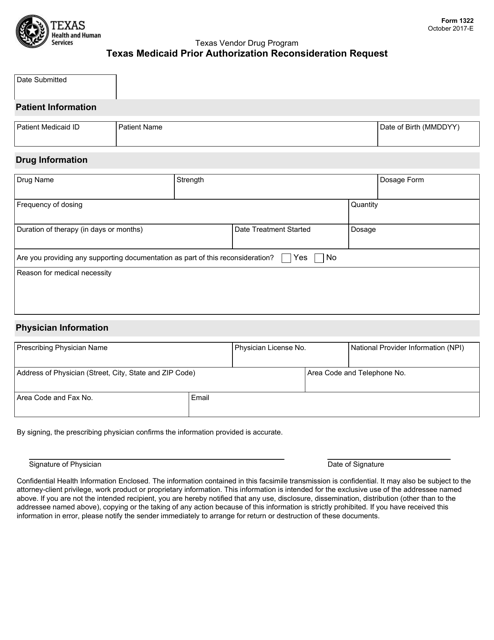
This form is used for requesting a reconsideration of a prior authorization decision under the Texas Medicaid program.
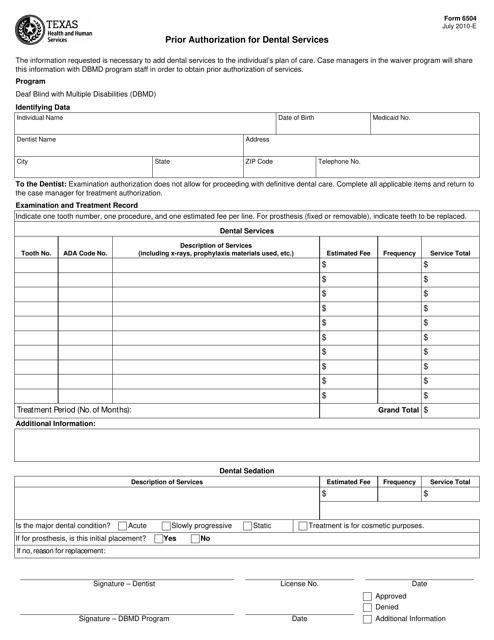
This form is used for obtaining prior authorization for dental services in the state of Texas. It is required to receive approval for certain dental procedures before they can be covered by insurance.