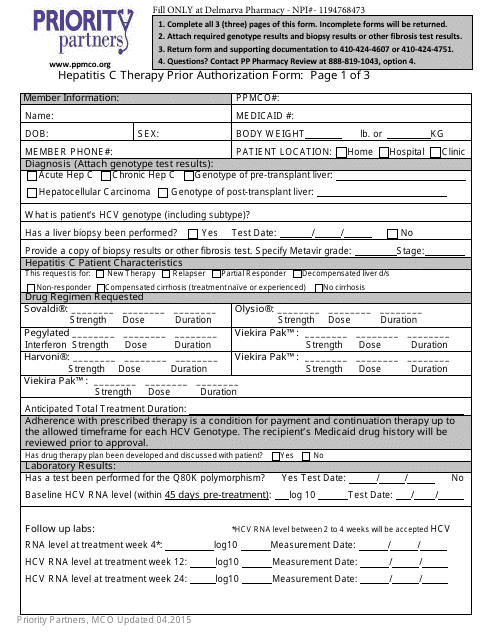
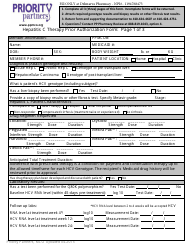
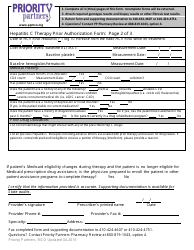
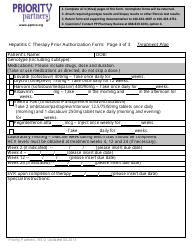
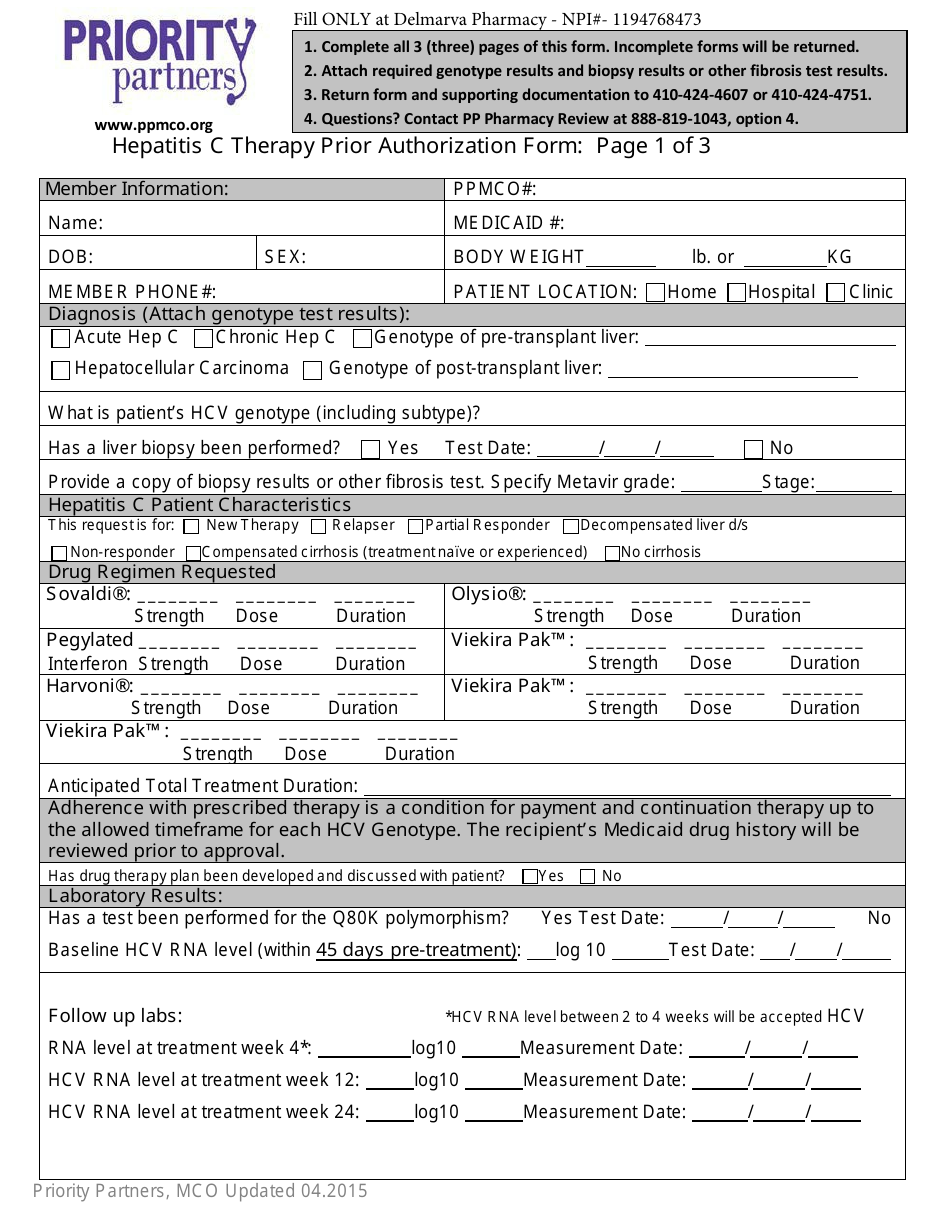
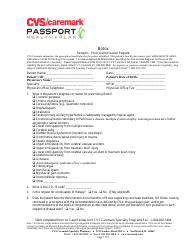
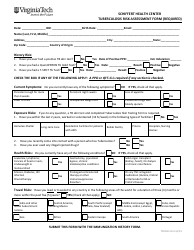
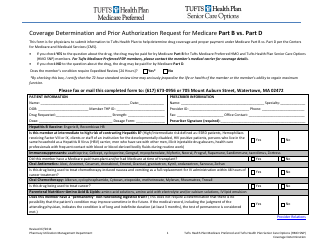
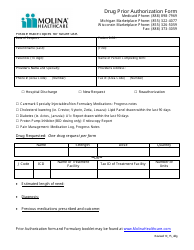
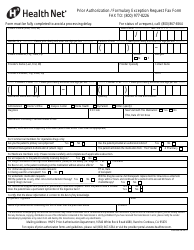
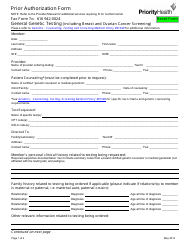
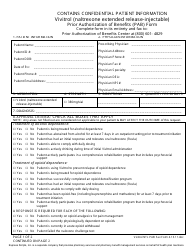
Hepatitis C Therapy Prior Authorization Form - Priority Partners
The Hepatitis C Therapy Prior Authorization Form is used by Priority Partners to determine coverage and authorization for Hepatitis C treatment. It is necessary to fill out this form in order to receive approval for the therapy.
FAQ
Q: What is the Hepatitis C Therapy Prior Authorization Form?
A: The Hepatitis C Therapy Prior Authorization Form is a document used by Priority Partners to request authorization for Hepatitis C therapy.
Q: Who needs to fill out the Hepatitis C Therapy Prior Authorization Form?
A: Healthcare providers who want to prescribe Hepatitis C therapy to their patients through Priority Partners need to fill out this form.
Q: What is the purpose of the form?
A: The purpose of the form is to request prior authorization for Hepatitis C therapy to ensure coverage and payment by Priority Partners.
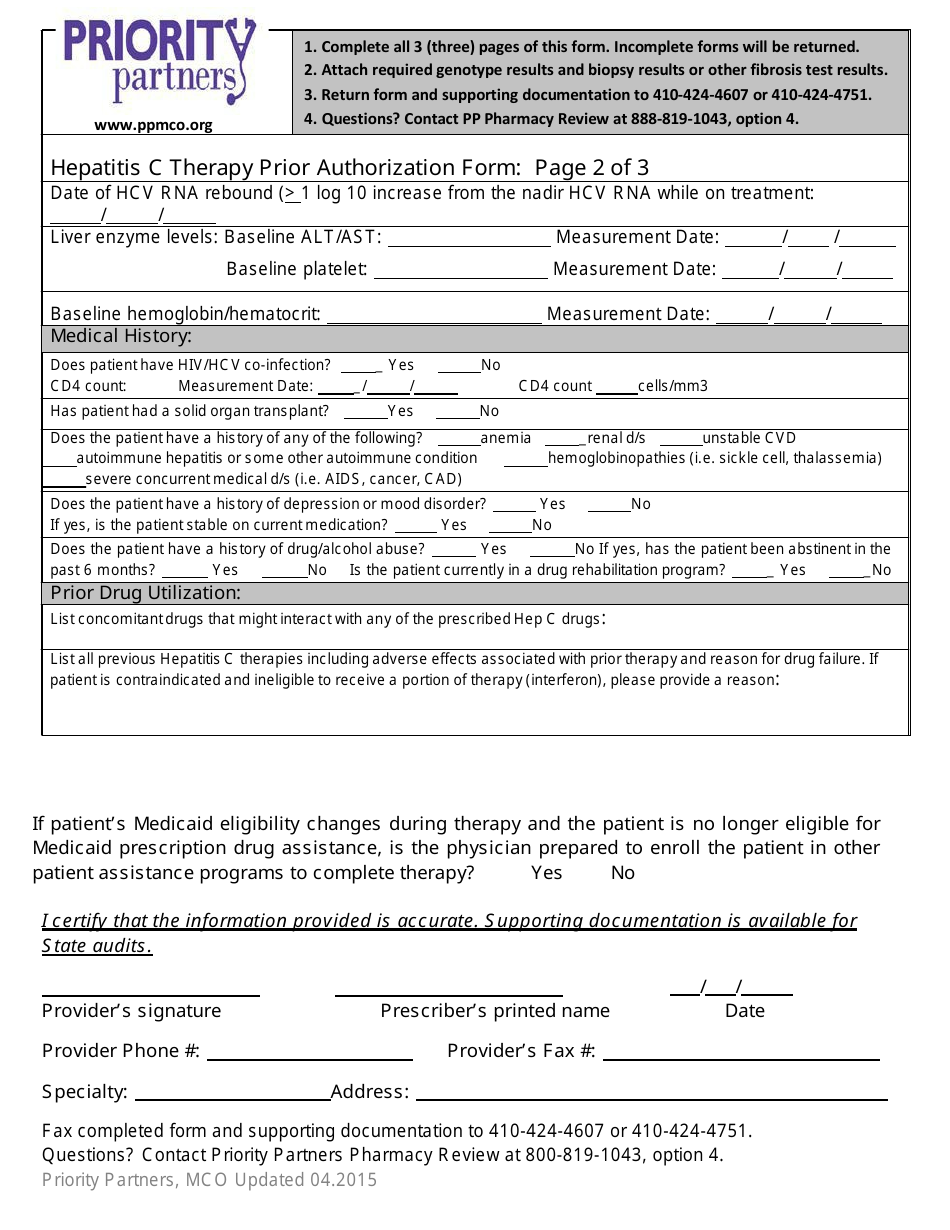
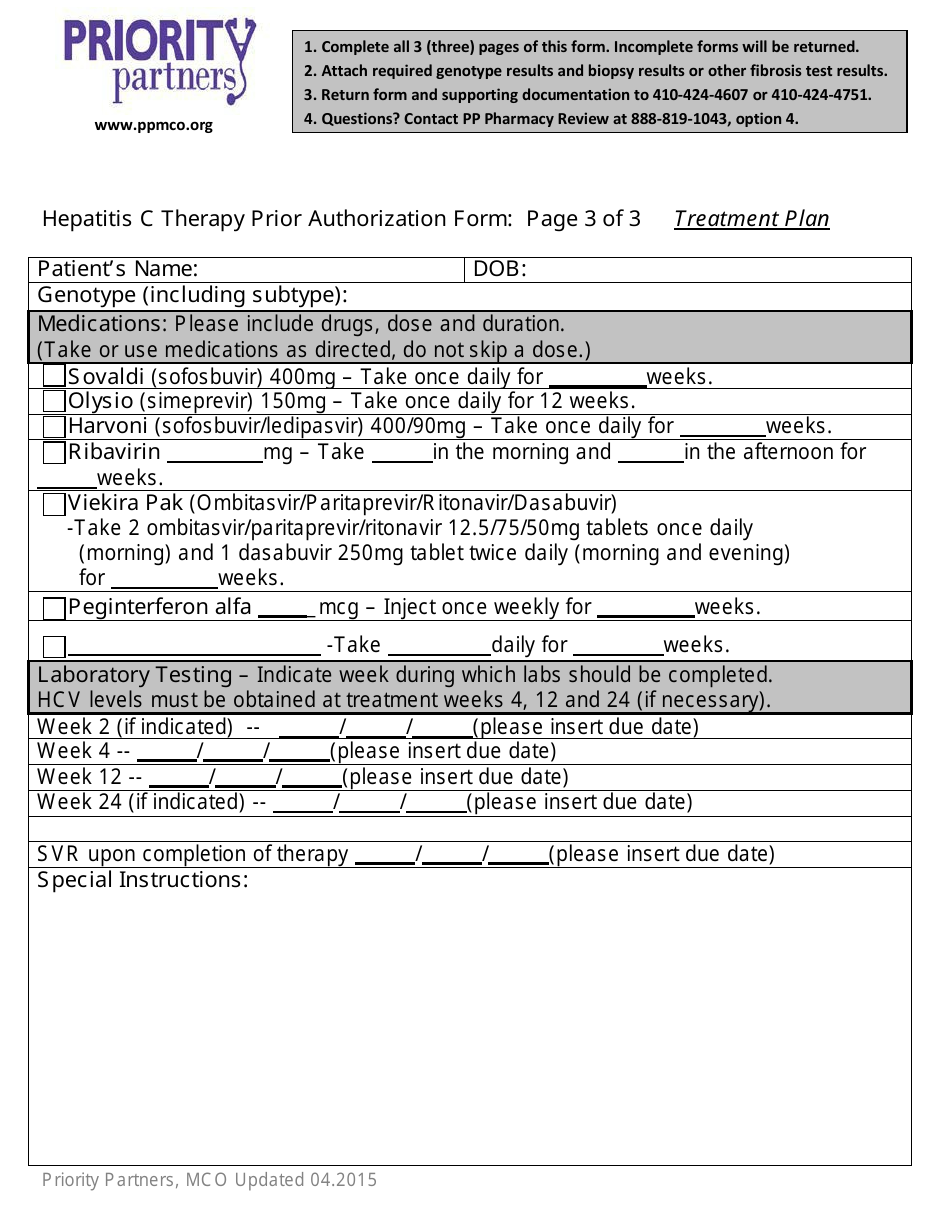
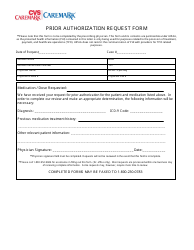
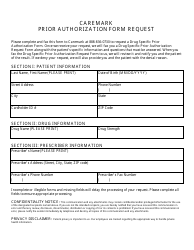
Q: What information is required on the form?
A: The form requires the healthcare provider to provide patient and prescriber information, diagnosis, treatment plan, and supporting documentation.
Q: How long does it take to process the form?
A: The processing time for the form may vary, but typically it takes a few business days to receive a decision from Priority Partners.
Q: What happens after the form is submitted?
A: After the form is submitted, Priority Partners will review the request and notify the healthcare provider of their decision regarding authorization.
Q: Is prior authorization guaranteed with the form?
A: No, prior authorization is not guaranteed with the form. The decision will depend on the clinical criteria and guidelines set by Priority Partners.
Q: What if the prior authorization request is denied?
A: If the request is denied, the healthcare provider can appeal the decision or explore alternative treatment options with Priority Partners.
Q: Are there any fees associated with the prior authorization process?
A: No, there are no fees associated with submitting the Hepatitis C Therapy Prior Authorization Form.