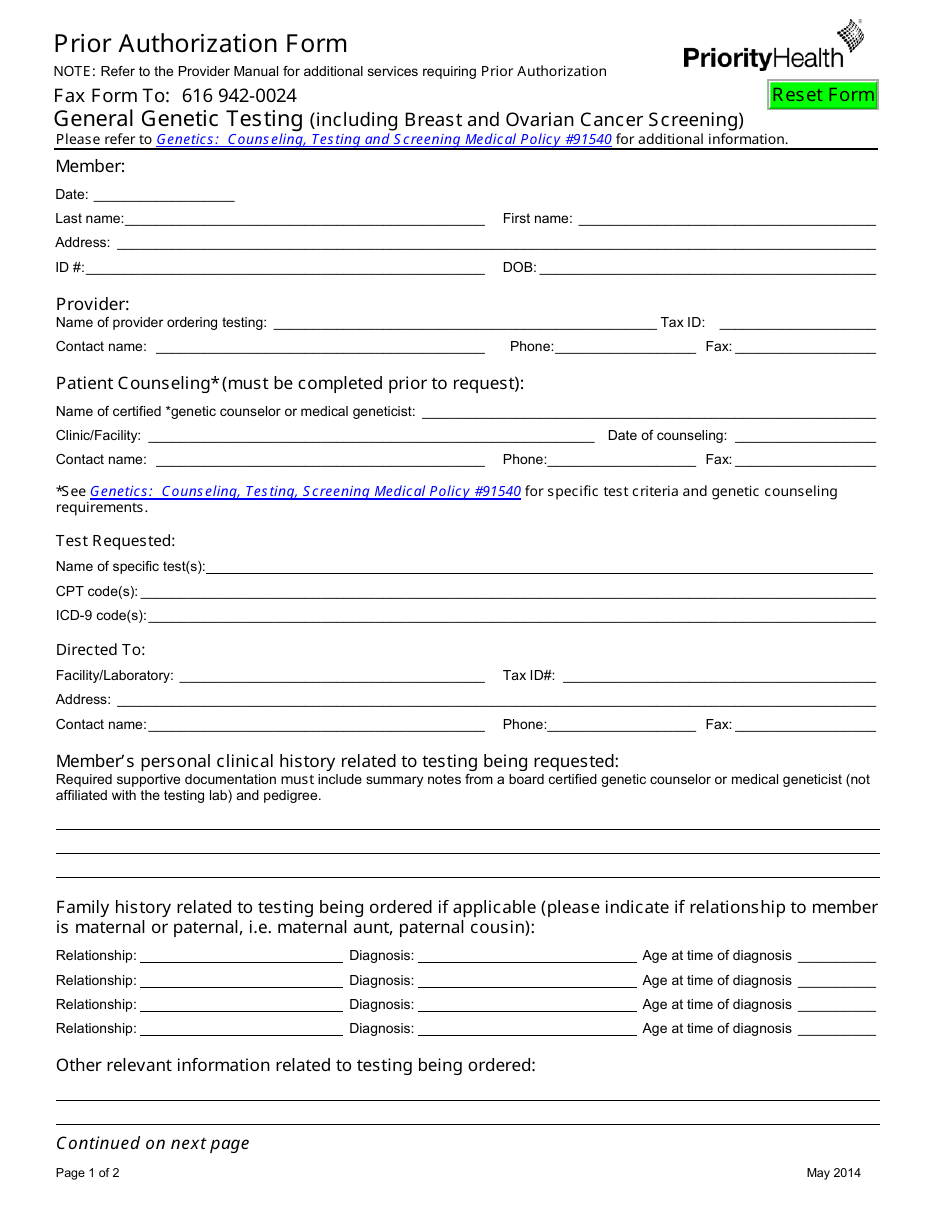
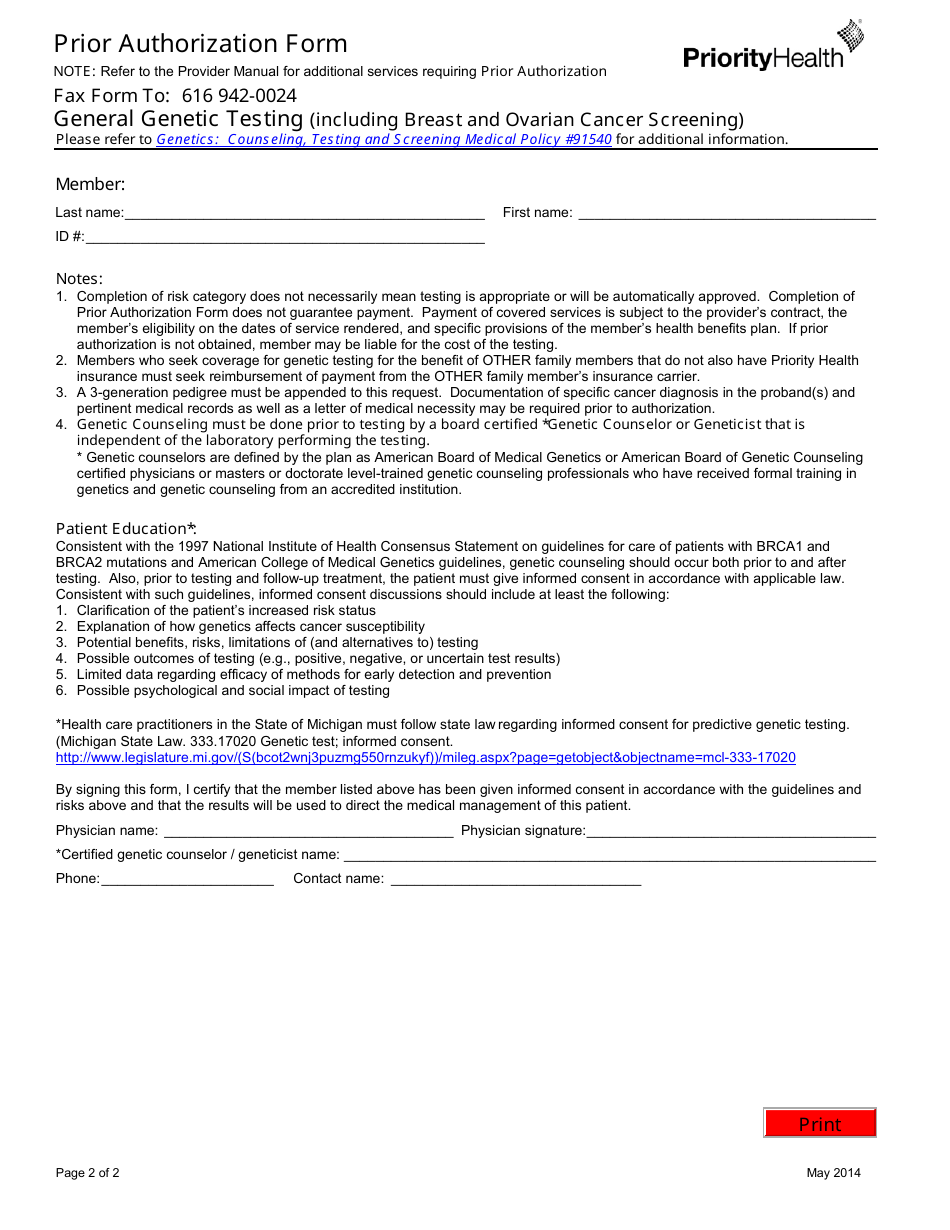
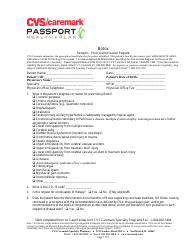
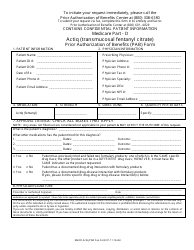
Prior Authorization Form - Priorityhealth
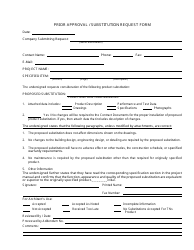
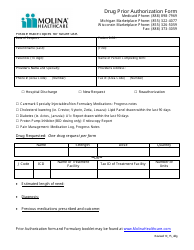
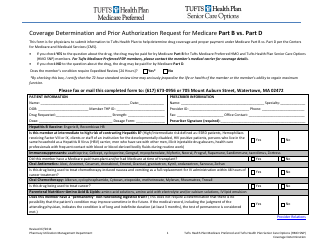
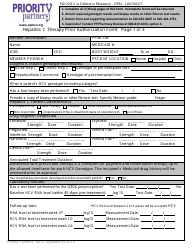
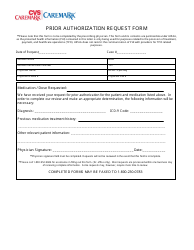
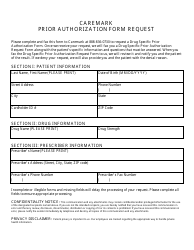
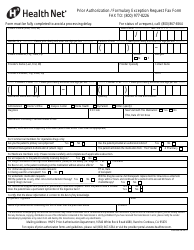
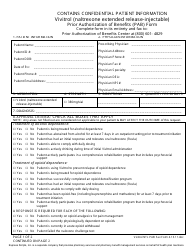
The Prior Authorization Form for Priority Health is used to request approval for certain medical services, treatments, or medications. It is typically required to ensure that the requested service is medically necessary and will be covered by the insurance plan.
The Prior Authorization Form for Priority Health is filed by the healthcare provider.
FAQ
Q: What is a prior authorization form?
A: A prior authorization form is a request from your doctor to your insurance company for approval of a specific medication, treatment, or procedure.
Q: Why is a prior authorization necessary?
A: Insurance companies require prior authorization to ensure that the prescribed treatment or medication is medically necessary and to determine coverage.
Q: What information is needed on a prior authorization form?
A: The form typically requires information such as your personal details, the treating physician's information, the medication or treatment being requested, and supporting documentation from the doctor.
Q: How long does it take for a prior authorization to be approved?
A: The time required for approval varies depending on the complexity of the request, but it can take a few days to a few weeks in some cases.
Q: What if my prior authorization is denied?
A: If your prior authorization is denied, you can discuss alternative treatment options with your doctor or file an appeal with your insurance company.
Q: Will I have to pay for a prior authorization?
A: Most insurance plans cover the cost of prior authorizations, but it's always best to check with your insurance company to confirm.