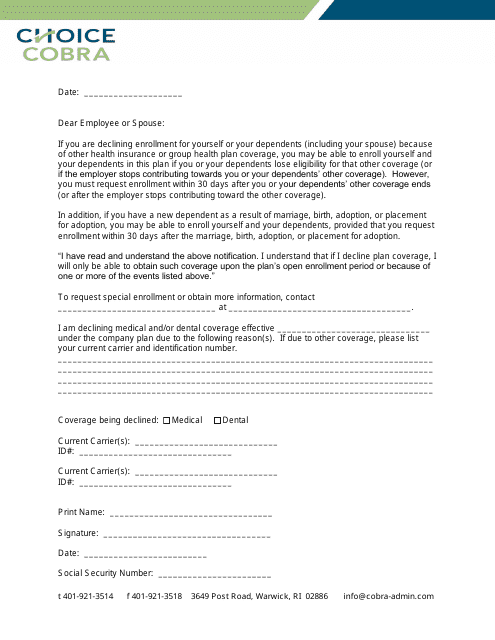
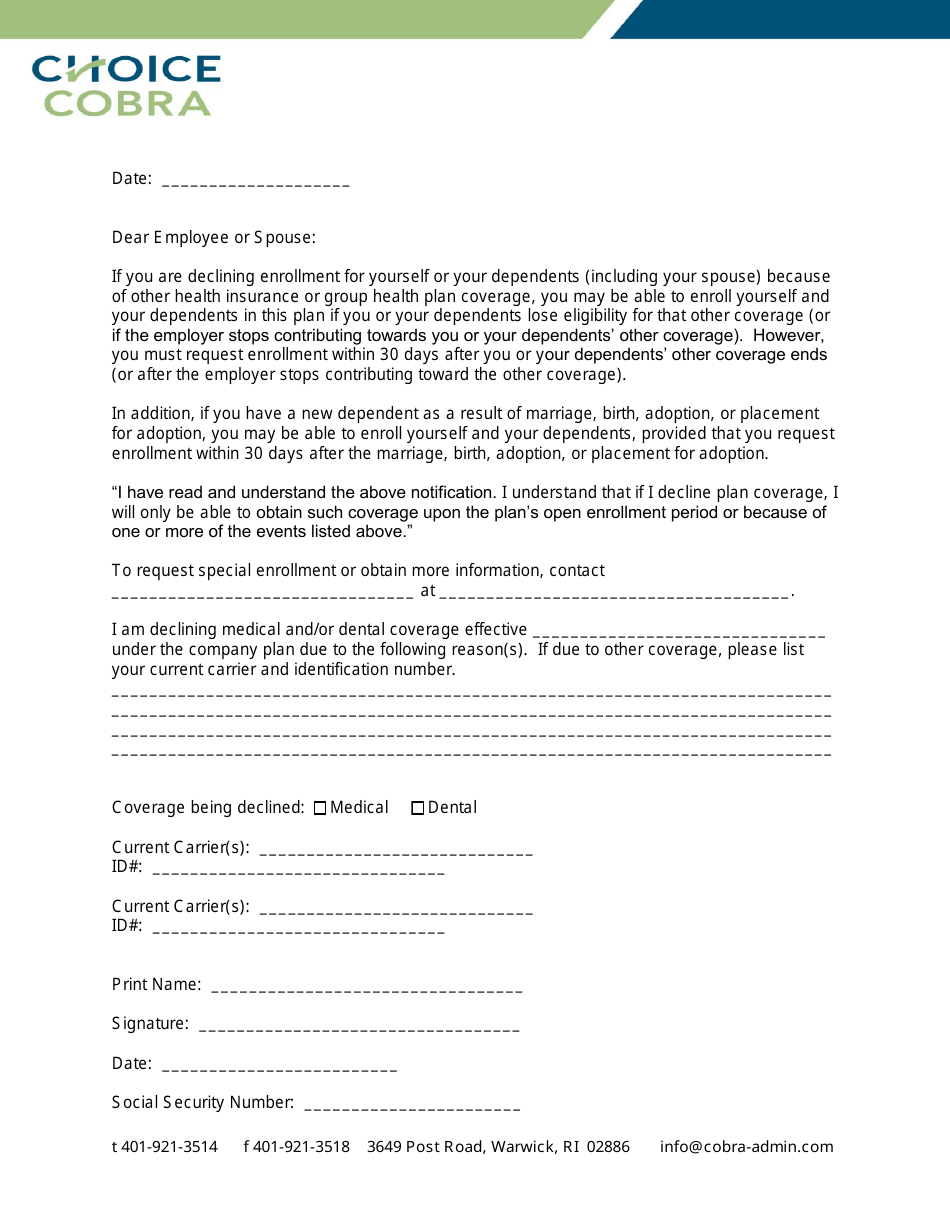
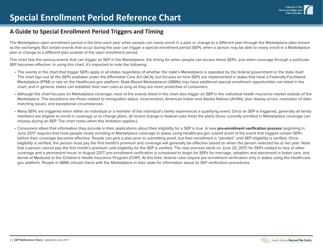
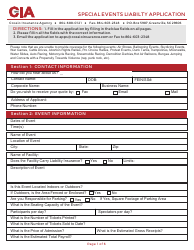
Special Enrollment Rights Notice and Waiver Form - Choice Cobra
The Special Enrollment Rights Notice and Waiver Form - Choice COBRA is typically used for providing information and obtaining consent for continuing health coverage under COBRA (Consolidated Omnibus Budget Reconciliation Act) after a qualifying event such as job loss or reduction in work hours. It ensures that individuals are aware of their rights to enroll in COBRA and gives them the option to decline coverage if they wish.
The Special Enrollment Rights Notice and Waiver Form - Choice COBRA is typically filed by the employer or the group health plan administrator.
FAQ
Q: What is a Special Enrollment Rights Notice and Waiver Form?
A: It is a form that provides information about special enrollment rights and allows individuals to waive those rights.
Q: What are special enrollment rights?
A: Special enrollment rights allow individuals to enroll in a health plan outside of the regular enrollment period under certain circumstances.
Q: When can special enrollment rights be used?
A: Special enrollment rights can be used when an individual experiences certain life events, such as getting married, having a baby, or losing other health coverage.
Q: Why would someone want to waive their special enrollment rights?
A: Someone might want to waive their special enrollment rights if they do not want or need to enroll in a health plan outside of the regular enrollment period.
Q: Is waiving special enrollment rights permanent?
A: Yes, once an individual waives their special enrollment rights, they cannot change their decision.
Q: Can an employer or health plan require a special enrollment rights waiver?
A: No, an employer or health plan cannot require someone to waive their special enrollment rights.