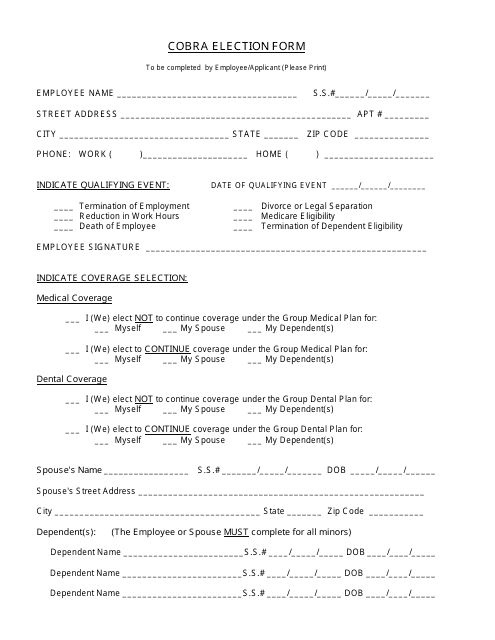
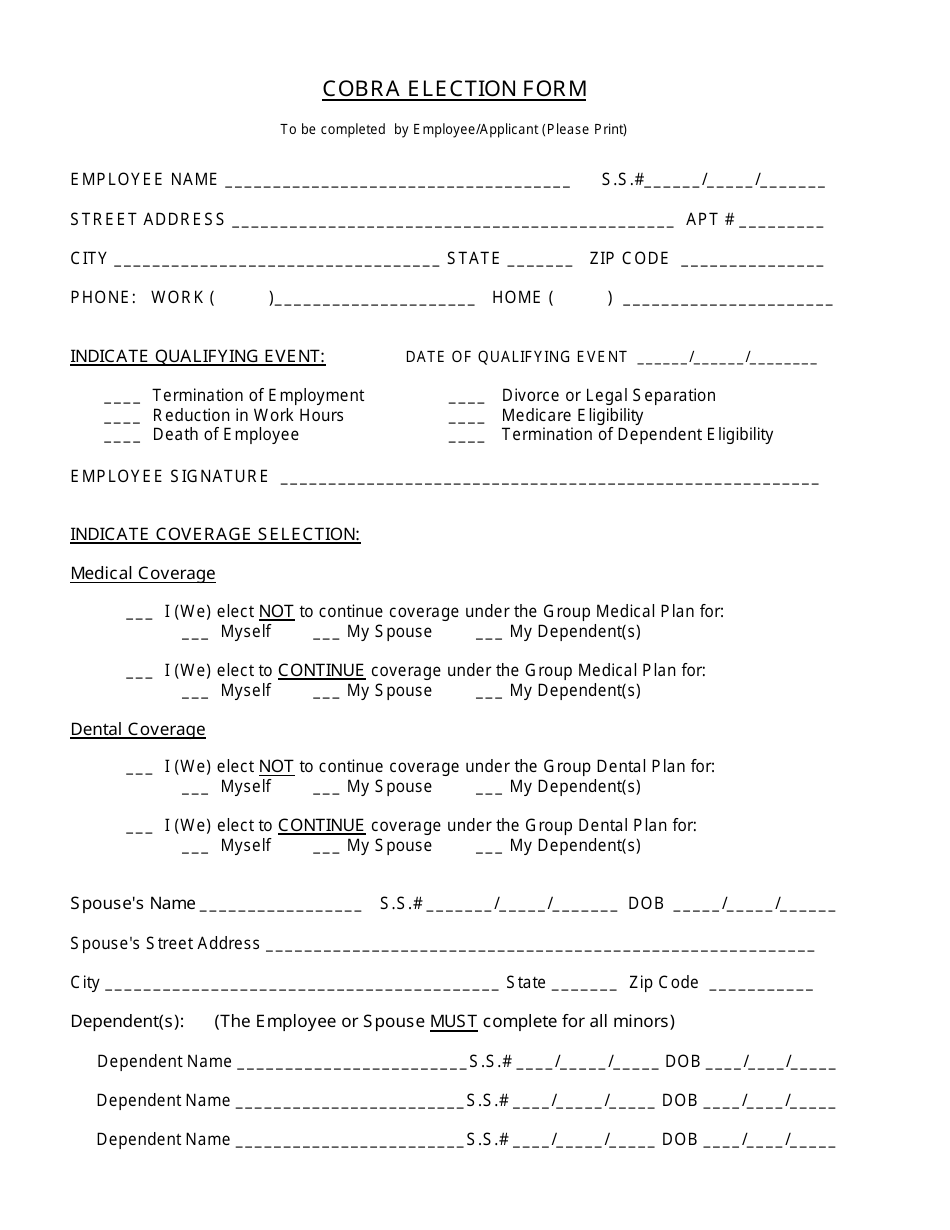
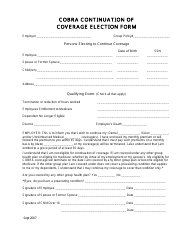
Cobra Election Form
The Cobra Election Form is used to apply for continued health insurance coverage through the Consolidated Omnibus Budget Reconciliation Act (COBRA) after a qualifying event, such as job loss or divorce, that would otherwise result in losing health insurance coverage.
The Cobra election form is typically filed by the employee who is eligible for the benefits.
FAQ
Q: What is the Cobra Election Form?
A: The Cobra Election Form is a document used to elect or decline continued health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA).
Q: Who needs to fill out the Cobra Election Form?
A: Employees who experience a qualifying event that makes them eligible for COBRA coverage, as well as their dependents, may need to fill out the Cobra Election Form.
Q: When should I submit the Cobra Election Form?
A: You should submit the Cobra Election Form within the specified deadline, usually within 60 days after the qualifying event.
Q: What information do I need to provide on the Cobra Election Form?
A: The Cobra Election Form typically requires you to provide personal information, details about your qualifying event, and your election to continue or decline COBRA coverage.
Q: What happens if I don't submit the Cobra Election Form?
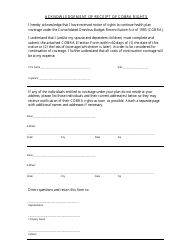
A: If you fail to submit the Cobra Election Form within the specified deadline, you may lose the opportunity to continue your health insurance coverage through COBRA.
Q: Can I change my election after submitting the Cobra Election Form?
A: If you initially elect COBRA coverage, you generally cannot change your election later unless you experience another qualifying event.