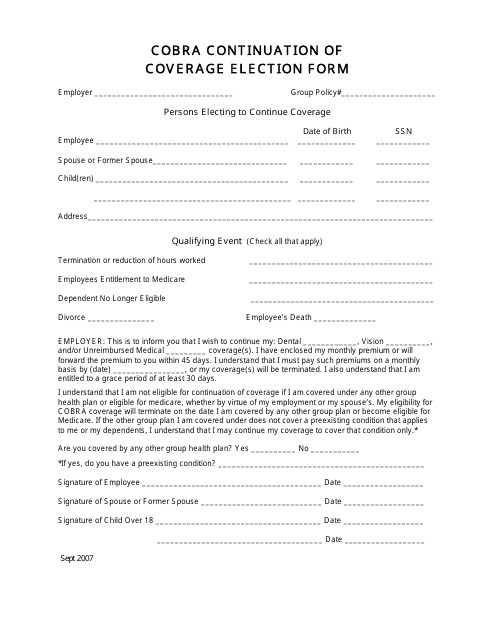
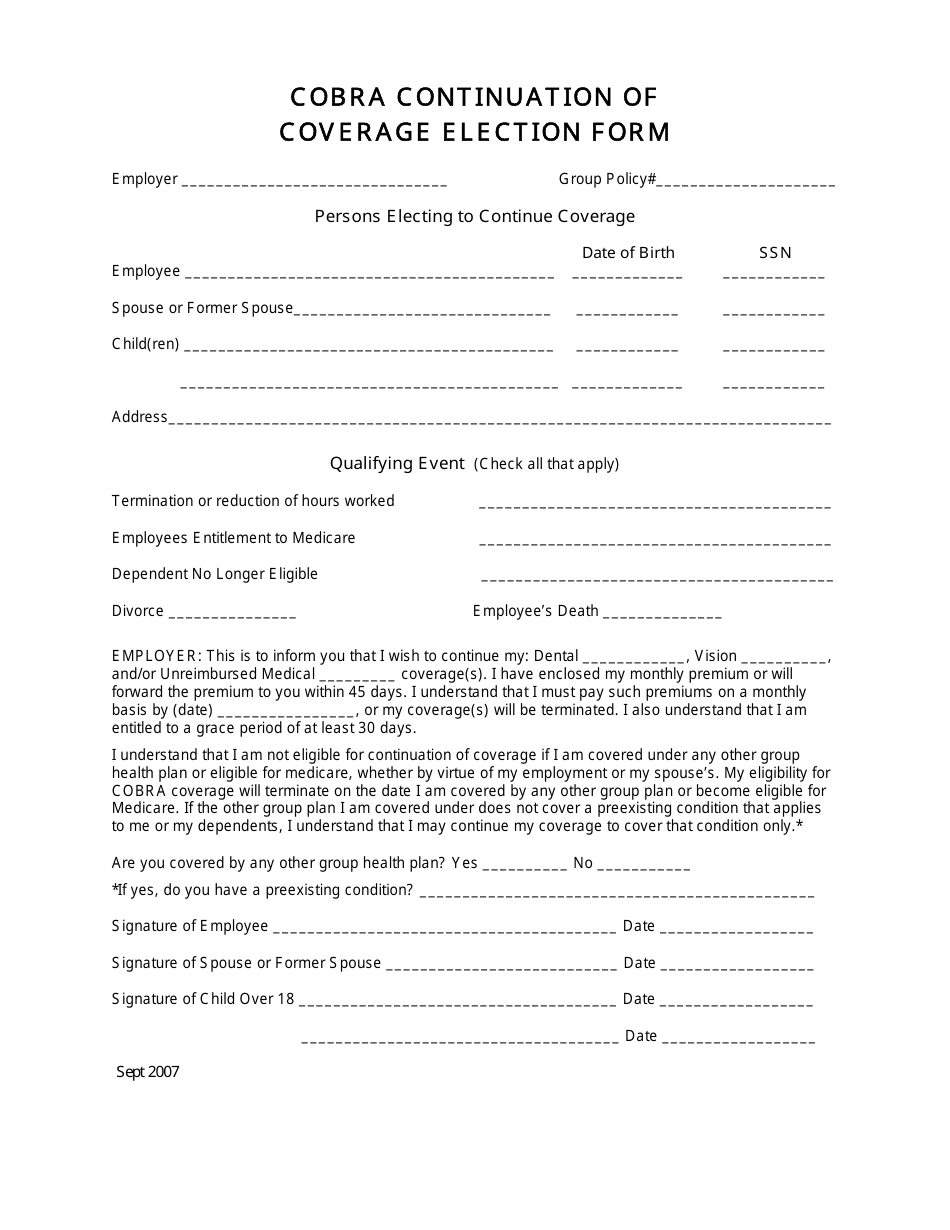
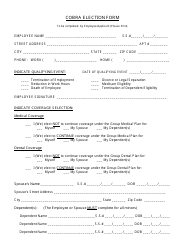
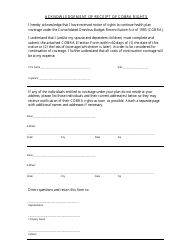
Cobra Continuation of Coverage Election Form
The Cobra Continuation of Coverage Election Form is used to enroll in continued health insurance coverage after experiencing a qualifying event that results in the loss of eligibility for a group health plan.
The Cobra Continuation of Coverage Election Form is typically filed by the former employee or the covered employee's qualified beneficiaries.
FAQ
Q: What is a Cobra Continuation of Coverage Election Form?
A: The Cobra Continuation of Coverage Election Form is a document that allows eligible individuals to elect to continue their employer-sponsored health insurance coverage after experiencing a qualifying event.
Q: Who is eligible to use a Cobra Continuation of Coverage Election Form?
A: Employees, their spouses, and dependent children are typically eligible to use a Cobra Continuation of Coverage Election Form if they experience a qualifying event that causes them to lose their employer-sponsored health insurance.
Q: What is a qualifying event?
A: A qualifying event is an event that causes an individual to lose their employer-sponsored health insurance coverage, such as termination of employment, divorce, or death of the covered employee.
Q: How long do I have to submit a Cobra Continuation of Coverage Election Form?
A: The timeframe to submit a Cobra Continuation of Coverage Election Form is typically within 60 days of the qualifying event.
Q: What are the benefits of using a Cobra Continuation of Coverage Election Form?
A: By using a Cobra Continuation of Coverage Election Form, eligible individuals can continue their employer-sponsored health insurance coverage, although they may have to pay the full premium themselves.