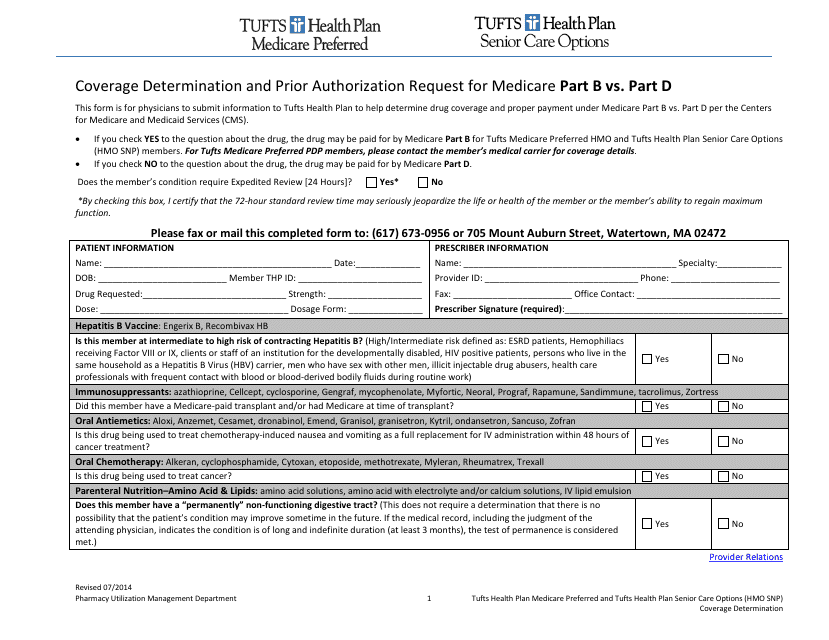
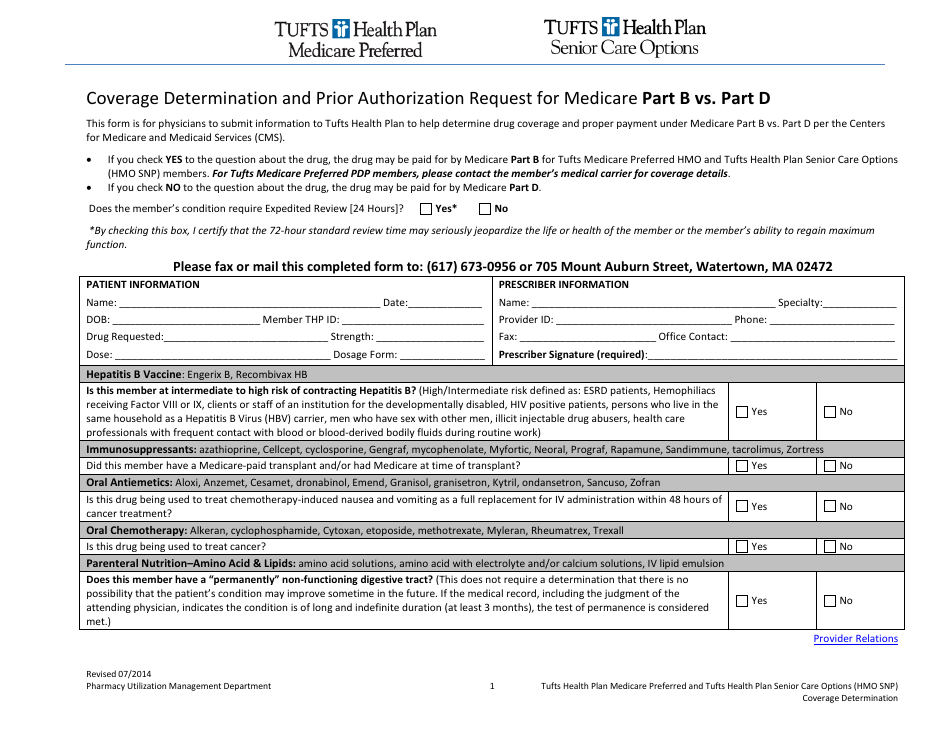
Coverage Determination Form and Prior Authorization Request for Medicare Part B VS. Part D - Tufts
The Coverage Determination Form for Medicare Part B and Part D is used by Tufts to determine if a specific medication or treatment is covered under the respective plans. The Prior Authorization Request is also used by Tufts to obtain approval in advance for certain medications or treatments before they can be covered by Medicare Part B or Part D.
In the case of Medicare Part B, the Coverage Determination Form and Prior Authorization Request are filed by the healthcare provider or the beneficiary themselves. For Medicare Part D, the process is typically handled by the beneficiary or their designated representative. However, it's important to note that specific procedures may vary depending on the insurance provider, Tufts Health Plan in this case. It is recommended to directly contact Tufts Health Plan for the most accurate information regarding their specific requirements for filing these forms.
FAQ
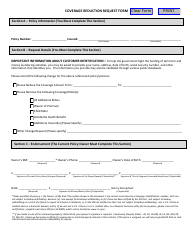
Q: What is a Coverage Determination Form?
A: A Coverage Determination Form is a document used to request coverage for a specific medication or medical service under Medicare Part B or Part D.
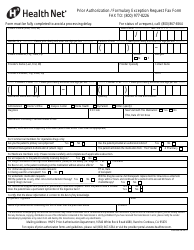
Q: What is a Prior Authorization Request?
A: A Prior Authorization Request is a document used to ask for approval from Medicare Part B or Part D to cover a specific medication or medical service.
Q: What is the difference between Medicare Part B and Part D?
A: Medicare Part B covers medical services like doctor's visits and outpatient care, while Medicare Part D covers prescription medications.
Q: When do I need to fill out a Coverage Determination Form?
A: You should fill out a Coverage Determination Form when you need to request coverage for a medication or medical service that is not automatically covered by Medicare.
Q: When do I need to submit a Prior Authorization Request?
A: You should submit a Prior Authorization Request when you need approval from Medicare Part B or Part D to cover a medication or medical service that requires prior authorization.