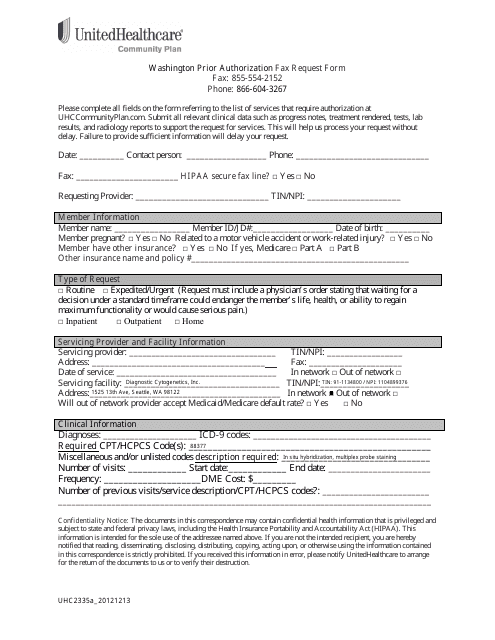
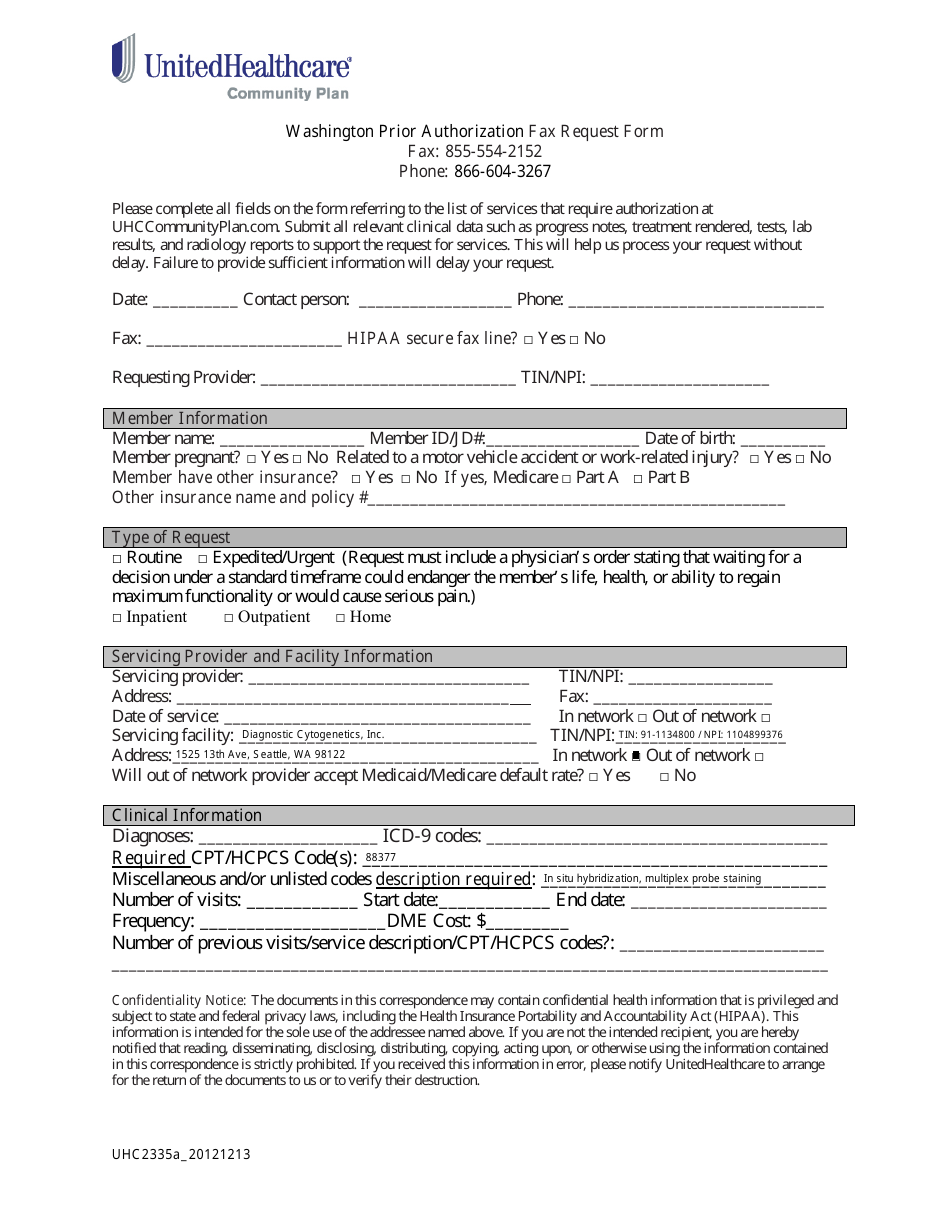
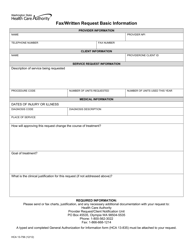
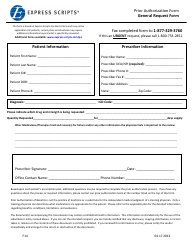
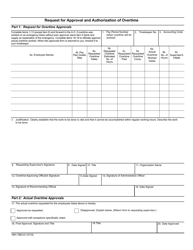
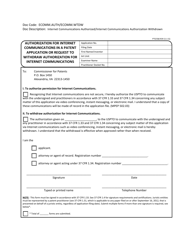
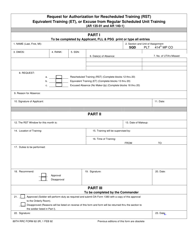
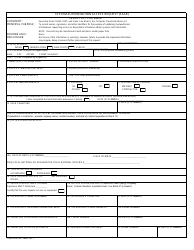
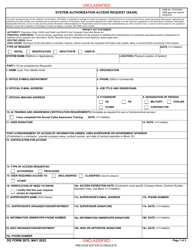
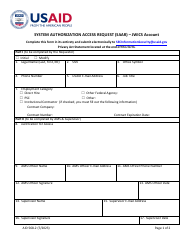
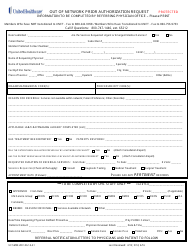
Form 2335a_20121213 Prior Authorization Fax Request Form - Unitedhealthcare - Washington
Form 2335a_20121213 Prior Authorization Fax Request Form is a document used by UnitedHealthcare in the state of Washington. This form is used to request prior authorization for certain medical treatments or services. Prior authorization is a process where the insurance company reviews and approves specific healthcare services before they are provided to ensure they are medically necessary and covered by the insurance plan. The form is typically faxed to UnitedHealthcare for review and processing.
The Form 2335a_20121213 Prior Authorization Fax Request Form for UnitedHealthcare in Washington is typically filed by the healthcare provider or their authorized representative.
FAQ
Q: What is Form 2335a_20121213?
A: Form 2335a_20121213 is the Prior Authorization Fax Request Form used for Unitedhealthcare in Washington.
Q: What is Prior Authorization?
A: Prior Authorization is a process used by health insurance companies to determine if they will cover a particular medication, procedure, or medical service.
Q: Why is Prior Authorization required?
A: Prior Authorization is typically required to ensure that the requested treatment, medication or procedure is medically necessary and meets the criteria set by the insurance company.
Q: What is the purpose of Form 2335a_20121213?
A: Form 2335a_20121213 is used to submit a request for Prior Authorization to Unitedhealthcare in Washington.
Q: When should I use Form 2335a_20121213?
A: You should use Form 2335a_20121213 when you need to request Prior Authorization for a specific medication, procedure, or medical service.
Q: How do I fill out Form 2335a_20121213?
A: You will need to provide your personal information, insurance details, information about the requested treatment or medication, and any supporting documentation.
Q: How long does it take to get a response after submitting Form 2335a_20121213?
A: The response time can vary, but insurance companies typically aim to provide a decision within a certain number of business days.
Q: What if my request for Prior Authorization is denied?
A: If your request for Prior Authorization is denied, you may have options to appeal the decision or explore alternative treatment options with your healthcare provider.