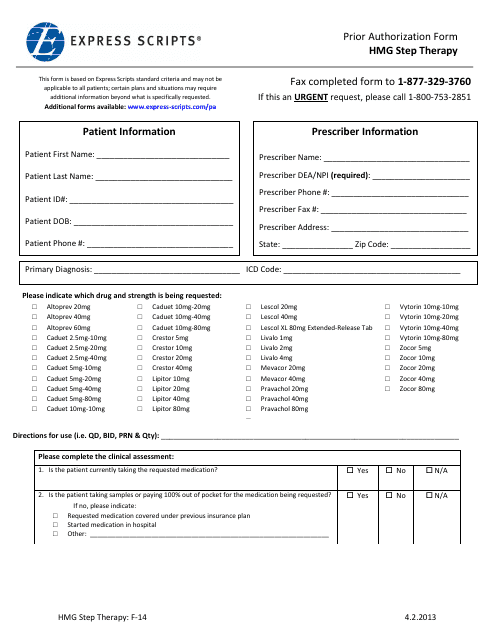
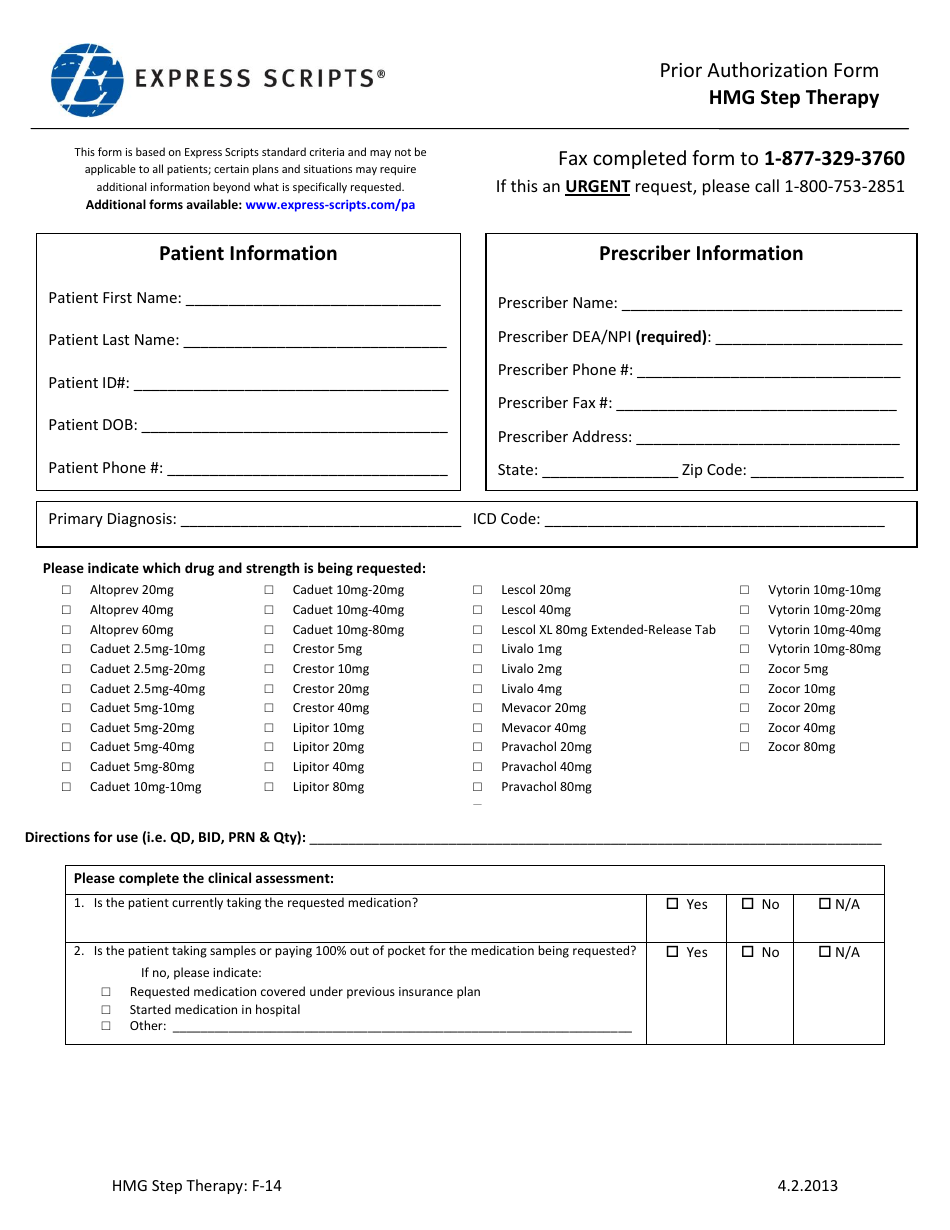
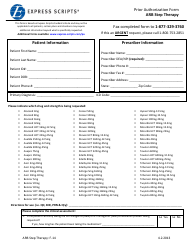
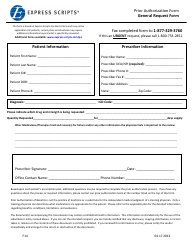
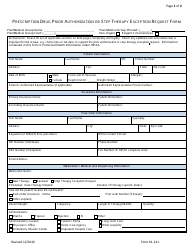
Form F14 Prior Authorization Form - Hmg Step Therapy - Express Scripts
The Form F14 Prior Authorization Form - Hmg Step Therapy - Express Scripts is used to request prior authorization for a specific medication called HMG, which is used to treat fertility issues. This form is used by Express Scripts, a pharmacy benefit manager, to determine if the medication is medically necessary and if step therapy requirements have been met.
FAQ
Q: What is the Form F14 Prior Authorization Form?
A: The Form F14 Prior Authorization Form is a document used to request prior authorization for a specific medication or treatment.
Q: What is Hmg Step Therapy?
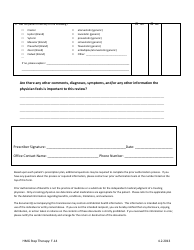
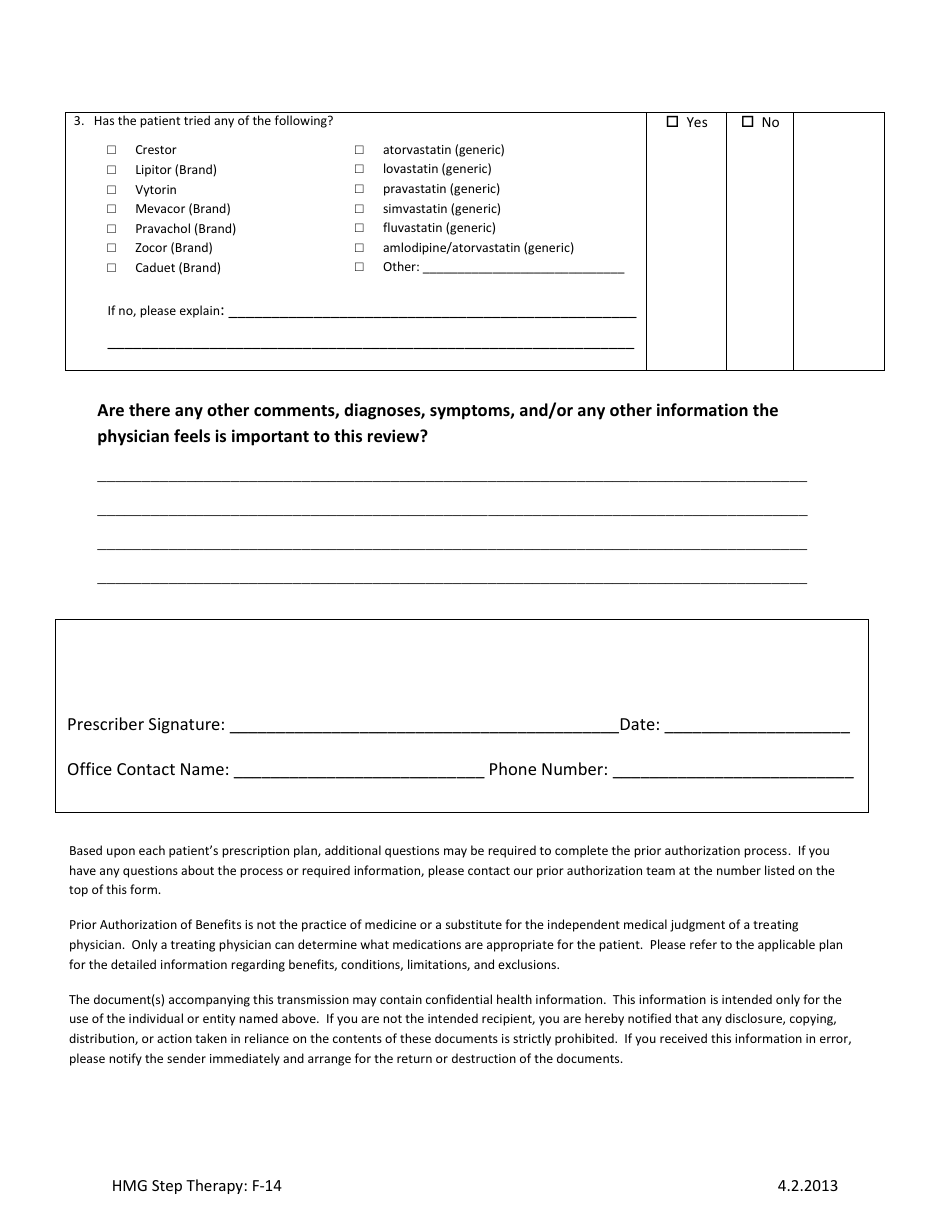
A: Hmg Step Therapy is a process used by Express Scripts to manage the use of certain medications. It requires patients to try lower-cost or preferred alternatives before using higher-cost medications.
Q: What is Express Scripts?
A: Express Scripts is a pharmacy benefits management company that helps manage prescription drug benefits for health plans, employers, and government programs.
Q: Why do I need to fill out the Form F14 Prior Authorization Form?
A: You need to fill out the Form F14 Prior Authorization Form to request approval for a medication or treatment that may require prior authorization from your health plan.
Q: How can I obtain the Form F14 Prior Authorization Form?
A: You can obtain the Form F14 Prior Authorization Form from your healthcare provider or by contacting Express Scripts directly.
Q: What information do I need to provide on the Form F14 Prior Authorization Form?
A: You will need to provide information such as your personal details, healthcare provider information, medication details, and the reason for the request.
Q: How long does it take to process a prior authorization request?
A: The processing time for prior authorization requests can vary, but it is typically within a few business days.
Q: What happens if my prior authorization request is approved?
A: If your prior authorization request is approved, you will be able to obtain the prescribed medication or treatment with coverage from your health plan.
Q: What if my prior authorization request is denied?
A: If your prior authorization request is denied, you may have options such as appealing the decision or exploring alternative treatment options with your healthcare provider.