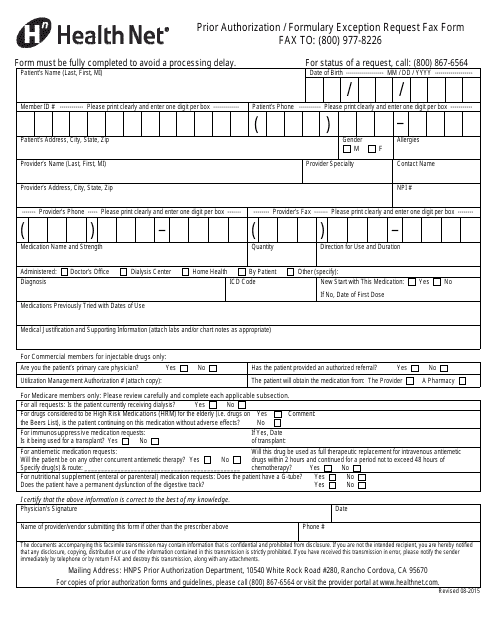
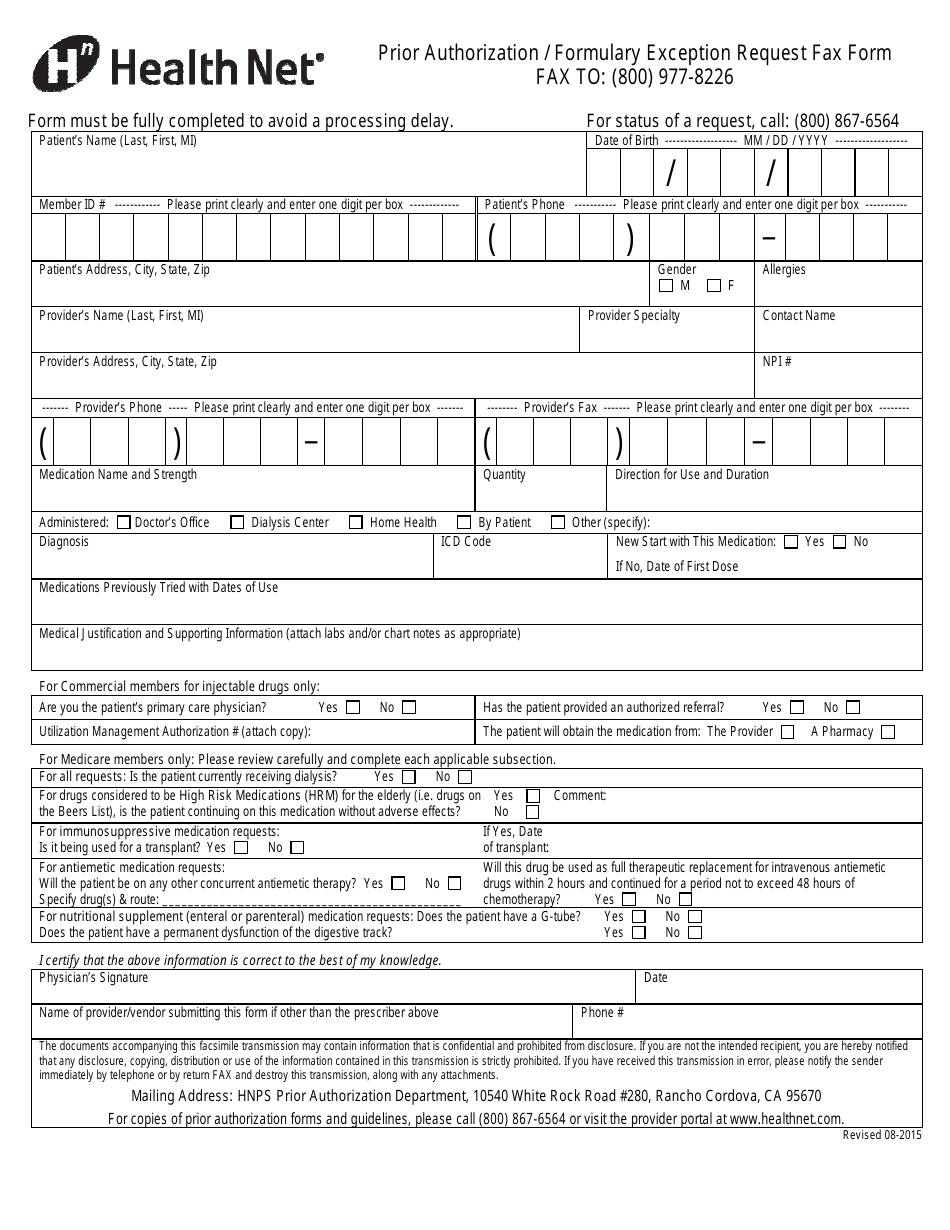
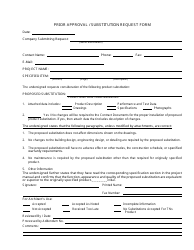
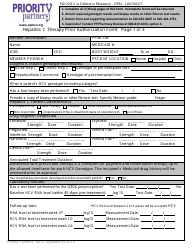
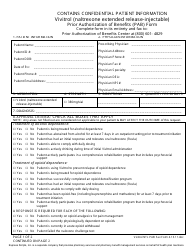
Prior Authorization / Formulary Exception Request Fax Form - Health Net
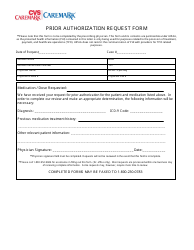
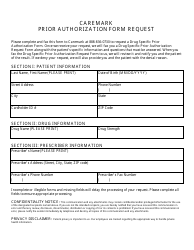
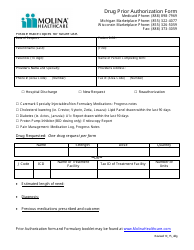
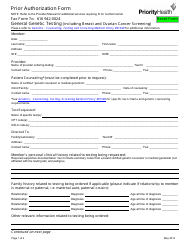
The Prior Authorization/Formulary Exception Request Fax Form is used by Health Net to request pre-approval for medications or treatments that may require prior authorization or are not covered by the drug formulary. This form allows healthcare providers to communicate with Health Net and provide necessary information to determine if the requested medication or treatment is medically necessary and should be covered by the insurance plan.
The Prior Authorization/Formulary Exception Request Fax Form for Health Net is typically filed by the healthcare provider or the pharmacist on behalf of the patient.
FAQ
Q: What is a prior authorization?
A: A prior authorization is a process where a health insurance company reviews a prescribed medication or medical treatment to determine if it is medically necessary and covered under the plan.
Q: What is a formulary exception request?
A: A formulary exception request is a process where an individual asks their health insurance company to cover a medication that is not included on the formulary (list of covered medications).
Q: What is a fax form?
A: A fax form is a document that can be filled out and sent via fax to request a prior authorization or formulary exception from a health insurance company, like Health Net.
Q: Why do I need to fill out a prior authorization or formulary exception request?
A: You may need to fill out a prior authorization or formulary exception request to ensure that your prescribed medication or medical treatment is covered by your health insurance and to avoid unexpected costs.