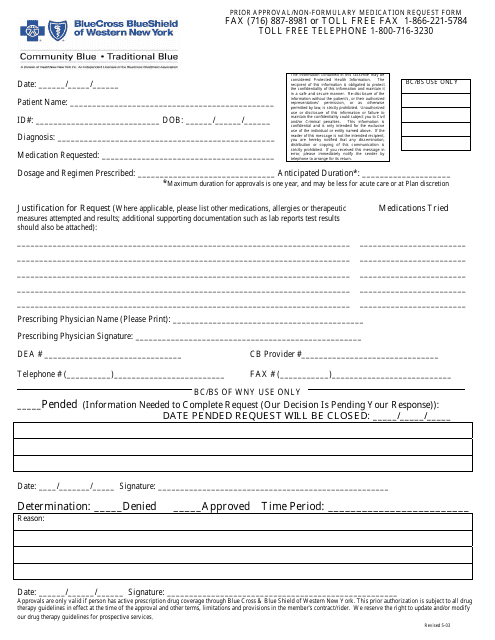
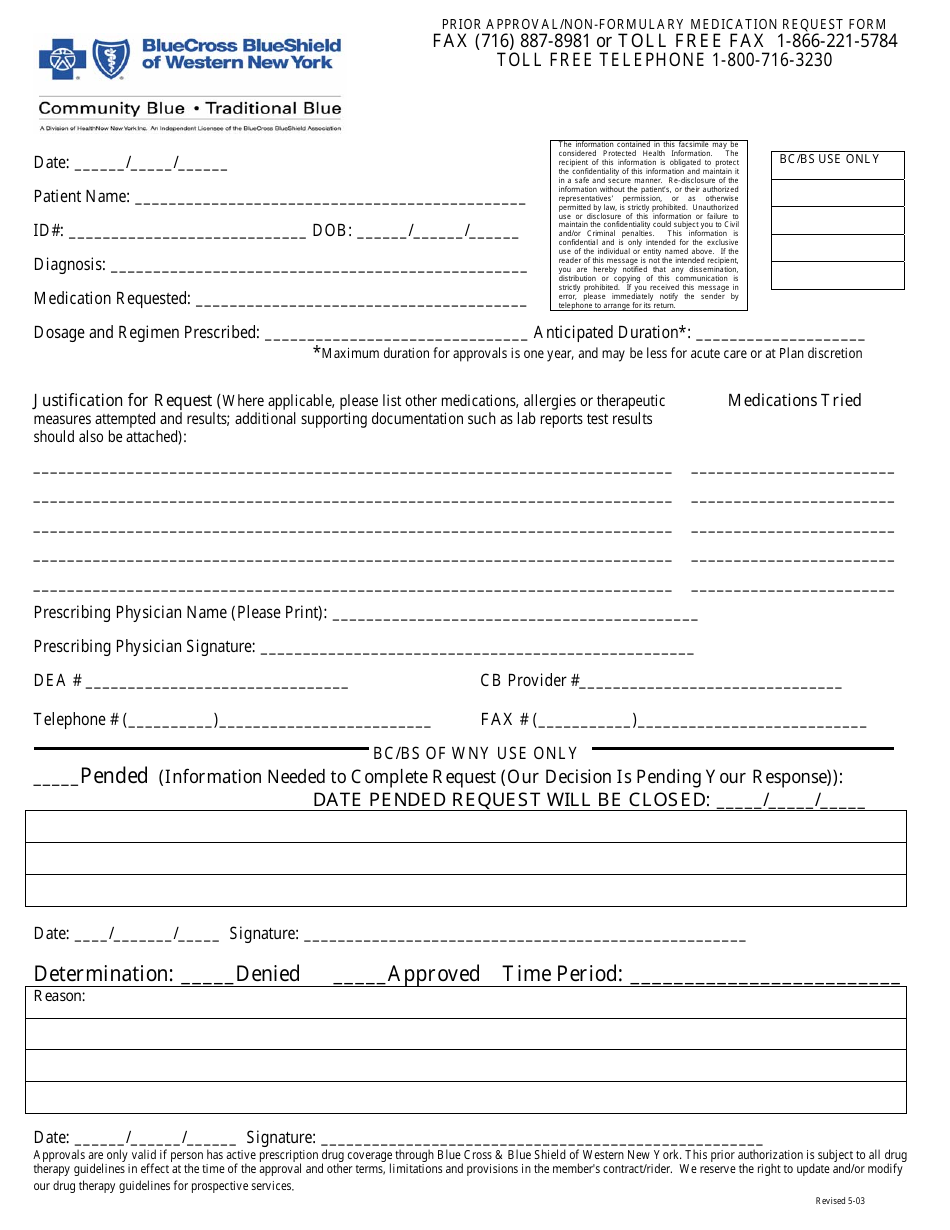
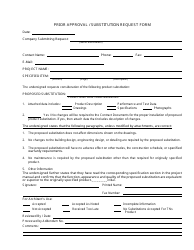
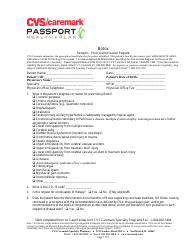
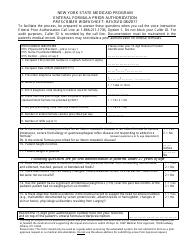
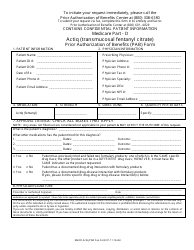
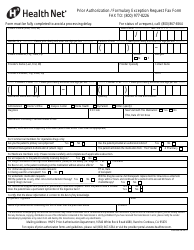
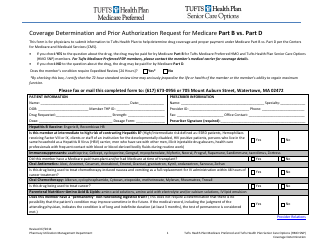
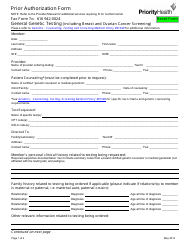
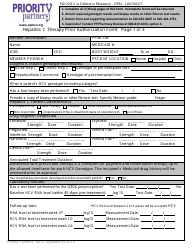
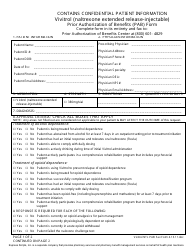
Prior Approval / Non-formulary Medication Request Form - Blue Cross Blue Shield of Western New York - New York
The Prior Approval/Non-formulary Medication Request Form is used by Blue Cross Blue Shield of Western New York in New York to request coverage for medications that are not on their standard formulary list. It allows members to seek approval for medications that may not be typically covered by their insurance plan.
The form is typically filed by the prescribing healthcare provider or pharmacist on behalf of the patient.
FAQ
Q: What is the Prior Approval/Non-formulary Medication Request Form?
A: The Prior Approval/Non-formulary Medication Request Form is a document used by Blue Cross Blue Shield of Western New York in New York.
Q: What is the purpose of the form?
A: The form is used to request approval for medications that are not included in the insurance company's formulary.
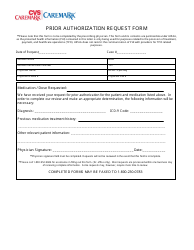
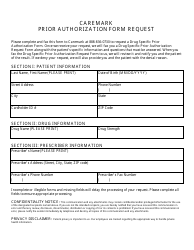
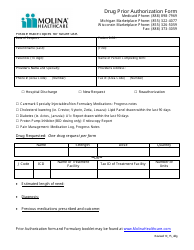
Q: What information is required on the form?
A: The form typically requires personal information, details about the medication, and supporting documentation from the prescribing physician.
Q: What happens after I submit the form?
A: After you submit the form, Blue Cross Blue Shield of Western New York will review your request and notify you of their decision.
Q: What if my request is denied?
A: If your request is denied, you may have other options such as requesting an appeal or exploring alternative medication options with your doctor.
Q: Is there a deadline for submitting the form?
A: There may be a deadline depending on your specific insurance plan. It is best to check with Blue Cross Blue Shield of Western New York for any deadline information.
Q: Can I fax or mail the form?
A: Yes, you can also fax or mail the Prior Approval/Non-formulary Medication Request Form if preferred.
Q: Are there any fees associated with the form?
A: It is best to review your insurance plan's details or contact Blue Cross Blue Shield of Western New York directly for information on any fees or copayments associated with the form.