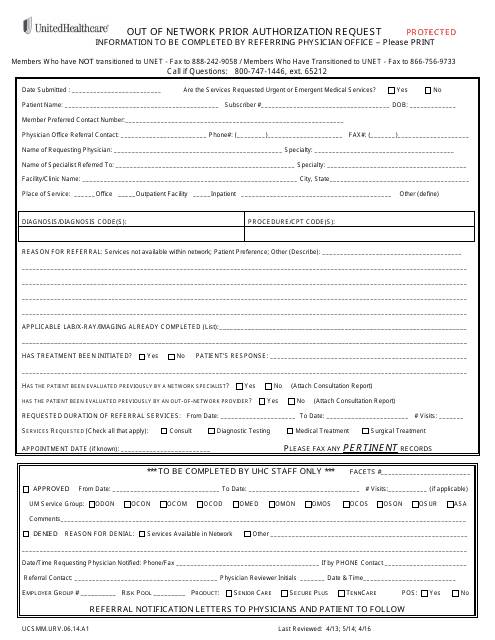
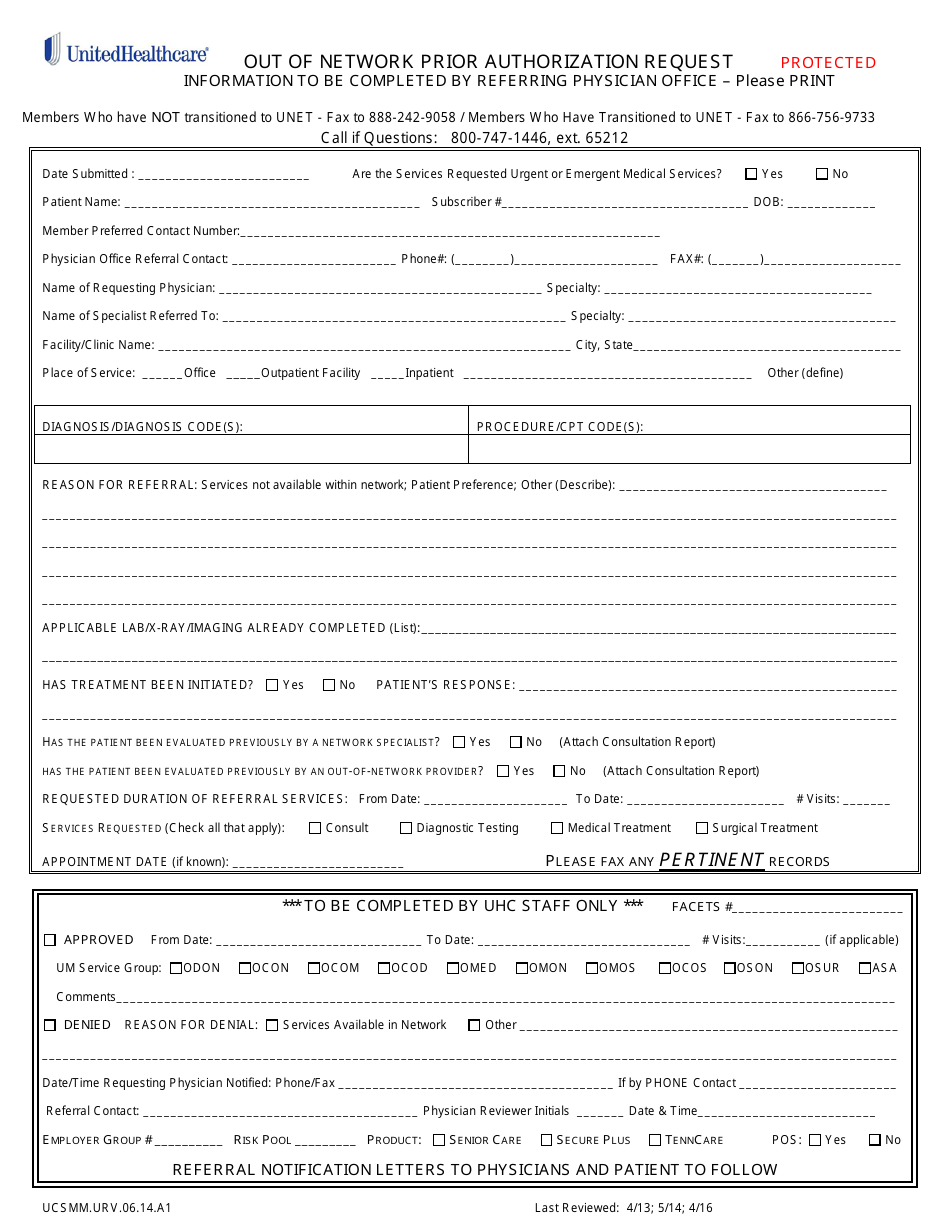
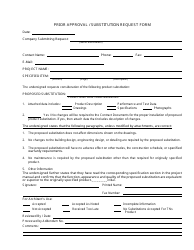
Form UCSMM.URV.06.14.A1 Out of Network Prior Authorization Request - Unitedhealthcare
Form UCSMM.URV.06.14.A1 Out of Network Prior Authorization Request - Unitedhealthcare is a document used by UnitedHealthcare members to request prior authorization for medical services that are out of network. This form is used to seek approval from the insurance provider for coverage of the medical services received from providers who are not in the UnitedHealthcare network.
The United Healthcare member or their authorized representative files the Form UCSMM.URV.06.14.A1 Out of Network Prior Authorization Request.
FAQ
Q: What is an Out of Network Prior Authorization Request?
A: An Out of Network Prior Authorization Request is a request to get approval from Unitedhealthcare for receiving out-of-network medical services.
Q: Why do I need to submit an Out of Network Prior Authorization Request?
A: You need to submit this request to ensure that you will receive coverage and reimbursement for out-of-network medical services.
Q: What information do I need to provide in the Out of Network Prior Authorization Request?
A: You will need to provide details about the medical service, the provider, and the reason for seeking out-of-network services.
Q: How long does it take to process an Out of Network Prior Authorization Request?
A: The processing time may vary, but it typically takes around 7-10 business days.