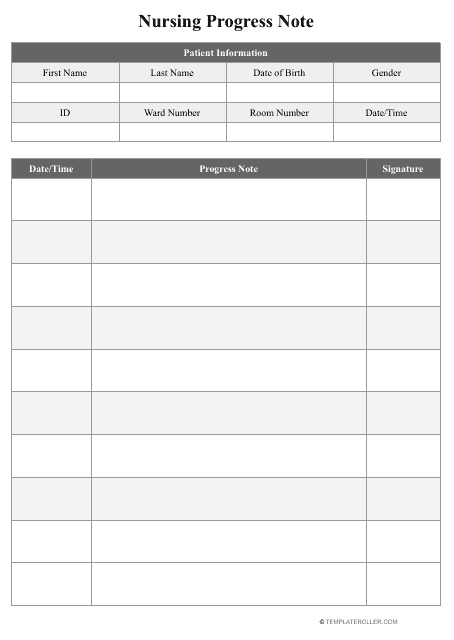
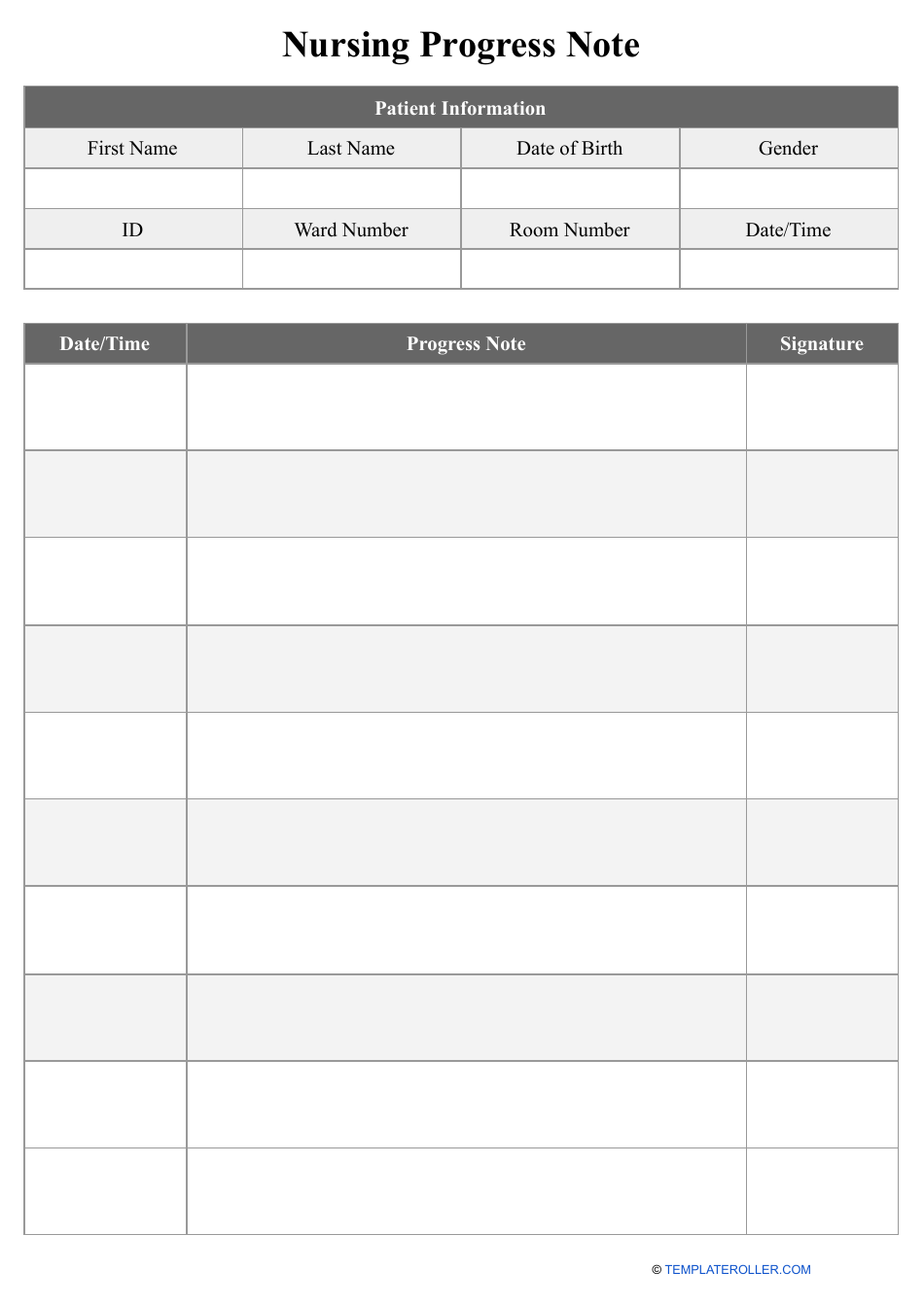
Nursing Progress Note Template
Nursing Progress Note Template: What Is It?
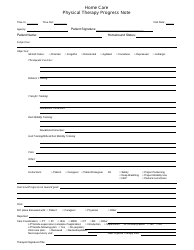
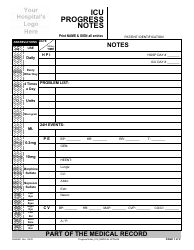
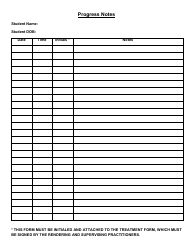
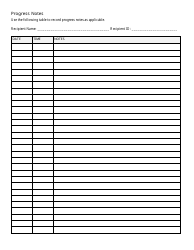
A Nursing Progress Note is a document that records the details of medical care received by a hospitalized patient. It can be completed by a doctor, nurse, physical therapist, and other healthcare professionals that monitor the health of a particular individual during their stay at a hospital - it is hard to imagine a single doctor can be present in the patient's room 24 hours a day, and this is why it is important to give other people visiting the patient and checking on them an opportunity to fill in the gaps and ensure the continuity of healthcare.
Download a Nursing Progress Note template via the link below.
What Should Be Included in Nursing Progress Notes?
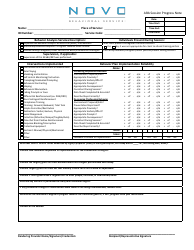
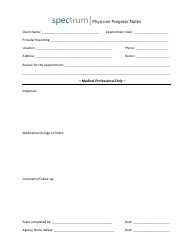
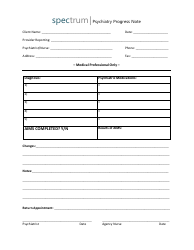
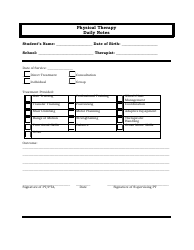
Here is what a member of the medical staff is supposed to include in a Nursing Progress Note:
-
General information . Identify the patient by their full name, date of birth, and number you have assigned to them (if applicable). State the date and time of the visit which customarily coincides with the time you are writing this note - in case you are recording the details later, it has to be properly reflected in the document.
-
Details of the diagnosis. Briefly mention the reason for the hospitalization and refer to the symptoms the patient has experienced upon appearing in your clinic - remember that you are not obliged to describe their entire medical history in this tool.
-
Observations made during a physical check-up . This section of the instrument is typically lengthy when the patient has just been hospitalized - it is the duty of a doctor to gather as much data as possible for further analysis; after that, the examination is usually brief unless the person's condition has worsened. Describe the general appearance of the patient, note any changes in their breathing and heart rate, and elaborate on the effects of the medication that has been selected.
-
List of medications given to the patient . We suggest you draw a table - it will be easier to enter the name of the drug and the dosage; doctors and nurses can tick the box and write down the time to confirm when the medication was received so that there is no overdose and the intervals between doses are maintained.
-
Summary of the visit . Indicate any positive and negative changes in the patient's physical and mental state based on the evidence you have on hand and treatment that has already been implemented.
How to Write Nursing Progress Notes?
Follow these tips for writing Nursing Progress Notes in order to enhance the quality of medical care your institution offers and meet the needs of a patient in a suitable way:
-
Record every single intervention you have made during the visit . Whether you have lowered the dosage of medication or asked the patient to lay on their side and not on their back, every little detail may have consequences for their health - it is crucial to be accurate and honest when completing this formal instrument.
-
Opt for a professional tone that lacks emotions and does not contain any assumptions related to a possible diagnosis or treatment you may consider in the future . Nursing Progress Notes are based on facts and events of the day - for instance, you are listing the medication prescribed to a patient as well as painful sensations they have told you about. Moreover, it is advised to be clear in terms of who performed a specific action - active voice will allow the person filling out the template to identify themselves while passive voice may lead to confusion.
-
Avoid vague wording and abbreviations other people that work with you right now or belong to the same field would not understand - it is likely you will deal with a referral, ask a fellow doctor to examine the patient to obtain a second opinion regarding their treatment, or disclose information put in writing to an insurance provider which is why it is necessary to create documentation that will be comprehensible without additional clarifications. When interacting with a patient, make sure they precise words instead of descriptions that can be misinterpreted in the future.
Still looking for a particular template? Take a look at the related templates and forms below: