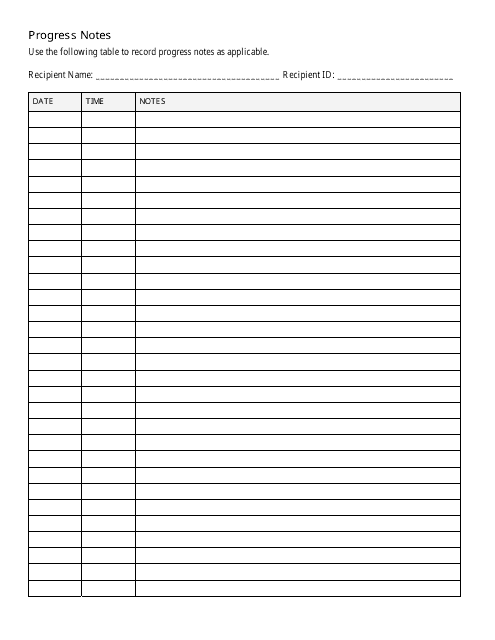
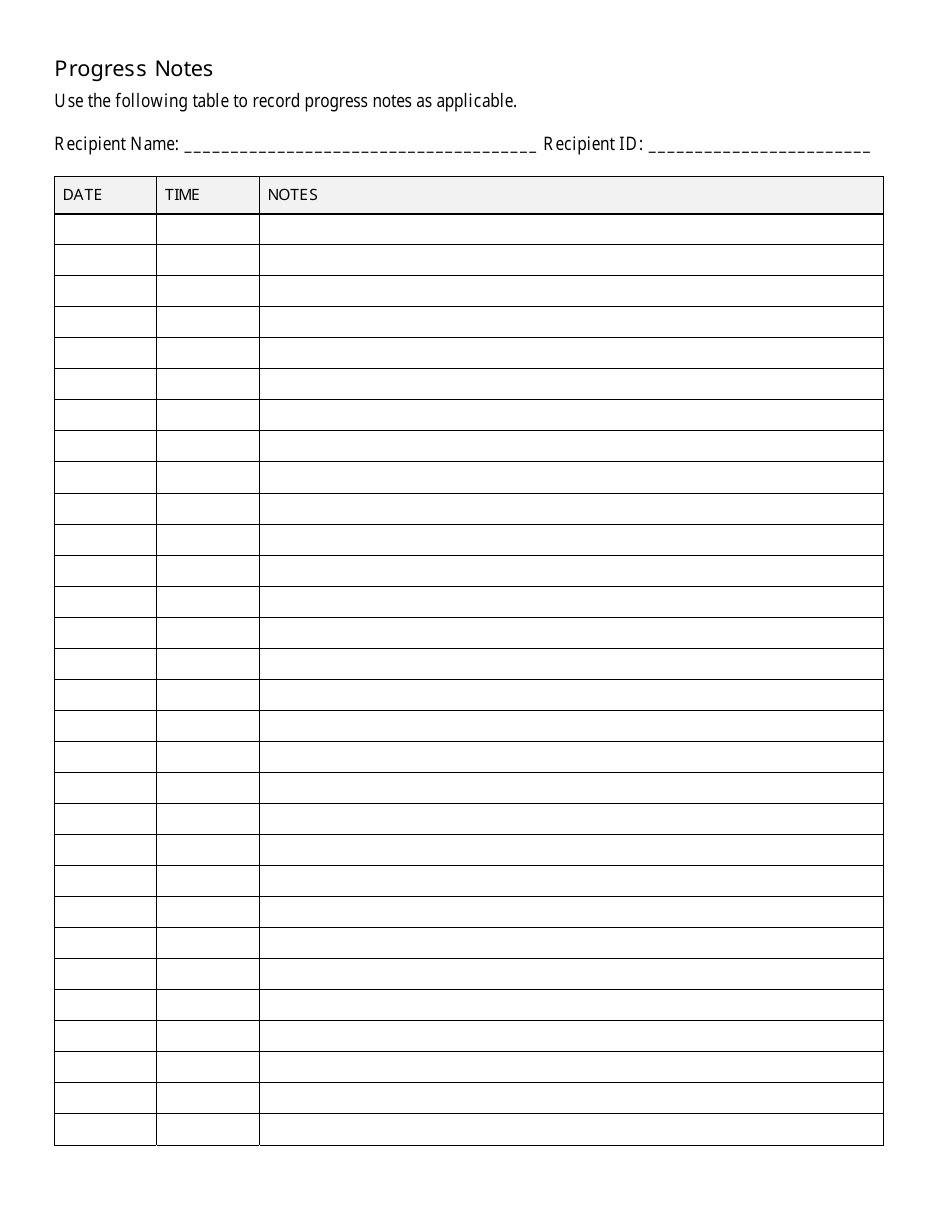
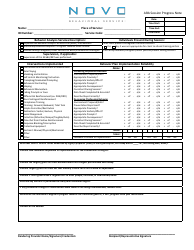
Progress Notes - Recipient
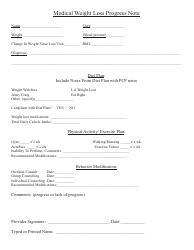
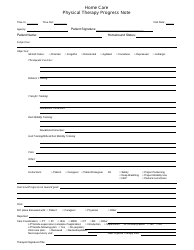
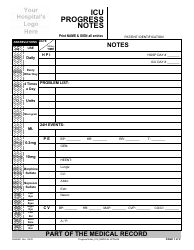
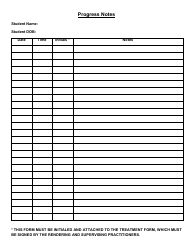
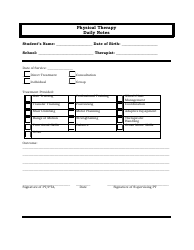
Progress Notes - Recipient is a document typically used in the healthcare sector, particularly in areas like mental health services, physical therapy, and social work. It serves as an essential tool for healthcare providers to track a patient's treatment progress, changes in their conditions, and the efficiency of a particular treatment or intervention.
This document summarizes each interaction that healthcare professionals have with their patients including the health services provided and the patient’s medical status, responses to treatment, and progress made toward goals. Communication between healthcare providers can also be tracked and facilitated using this document.
In essence, Progress Notes - Recipient helps to provide the best possible collaborative care for the patients and reduces the chances of errors while delivering medical services.
Progress notes are usually filed by healthcare providers that are directly involved in a patient's care. This typically includes doctors, nurses, therapists, and other medical professionals. They use these notes to document a patient's condition and treatment progress. The recipient does not typically file the progress notes, but they may be granted access to them on request or as per the healthcare policies of the respective country. In terms of the countries mentioned - the USA, Canada, India, and Australia - this is generally the standard practice. The scenarios might vary depending on specific healthcare systems and patient dataprivacy laws within these countries.
FAQ
Q: What are progress notes?
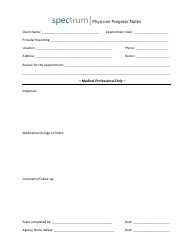
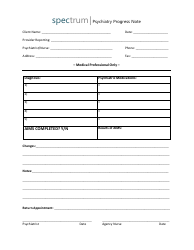
A: Progress notes are documents that healthcare professionals create to record information about patient treatment progress. They include details about the individual's diagnosis, treatment plan, patient's progress or lack thereof, and future treatment plans.
Q: What is the function of progress notes?
A: Progress notes serve as a record of a patient's treatment course. They provide a chronological account of patient care, serve as a communication tool among healthcare teams, and are essential for reviewing treatment plans and changes in patient's health.
Q: Who writes progress notes?
A: Progress notes are typically written by the healthcare professional directly involved in a patient's care. This could be a doctor, nurse, therapist, or social worker.
Q: Are progress notes confidential?
A: Yes, progress notes are confidential. They are part of a patient's medical record, which is protected under HIPAA in the US. Unauthorized access or disclosure of this information could result in penalties.
Q: How often are progress notes written?
A: The frequency of writing progress notes can depend on the clinical setting and the patient's condition. In some cases, they may be written daily, while in other situations, they may be written after each patient interaction.
Q: What information is included in a progress note?
A: Progress notes typically include facts like date and time of the note, patient's physical and mental health condition, treatment provided, patient's response to the treatment, changes in patient's condition, and any adjustments made to the treatment plan.
Q: What is the difference between progress notes and medical notes?
A: Medical notes include a broader range of information including medical history, diagnoses, tests, and treatments. Progress notes, on the other hand, are more specific to the ongoing care and treatment progress of a patient.