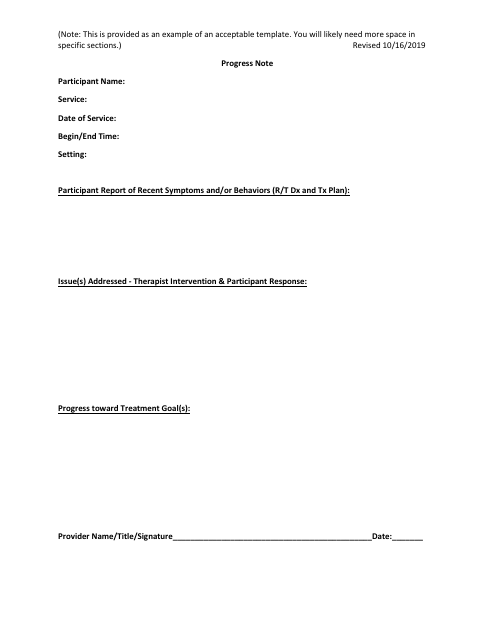
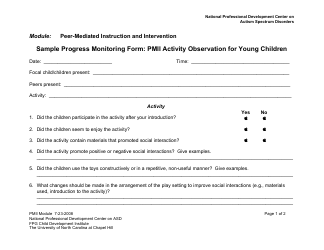
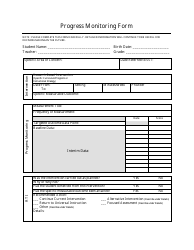
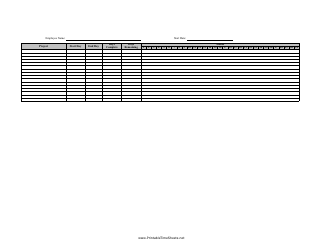
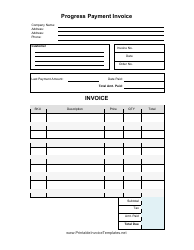
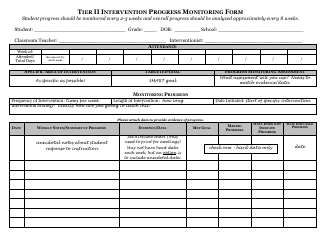
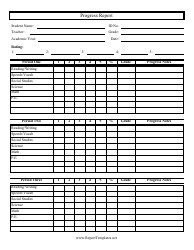
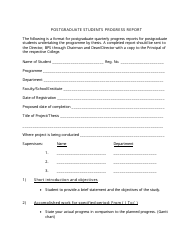
Progress Note
A progress note is used by healthcare professionals to document the progress and treatment of a patient during their ongoing medical care. It includes details such as the patient's symptoms, vital signs, diagnosis, treatment plans, and any changes in their condition. This helps track the patient's progress and ensures continuity of care.
The progress note is typically filed by a healthcare professional or provider, such as a doctor, nurse, or therapist, who is responsible for documenting and updating the patient's medical progress.
FAQ
Q: What is a progress note?
A: A progress note is a document that records the details of a patient's healthcare treatment and progress.
Q: Who writes progress notes?
A: Progress notes are typically written by healthcare professionals, such as doctors, nurses, and therapists.
Q: What information is included in a progress note?
A: A progress note usually includes the patient's medical history, current symptoms, medications, vital signs, and any changes in their condition.
Q: Why are progress notes important?
A: Progress notes are important for continuity of care, as they provide a record of the patient's treatment and progress over time.
Q: Who has access to progress notes?
A: Access to progress notes is typically limited to healthcare professionals involved in the patient's care, although patients may also have access to their own progress notes.