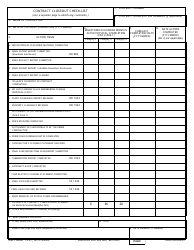
Discharge Planning Checklist
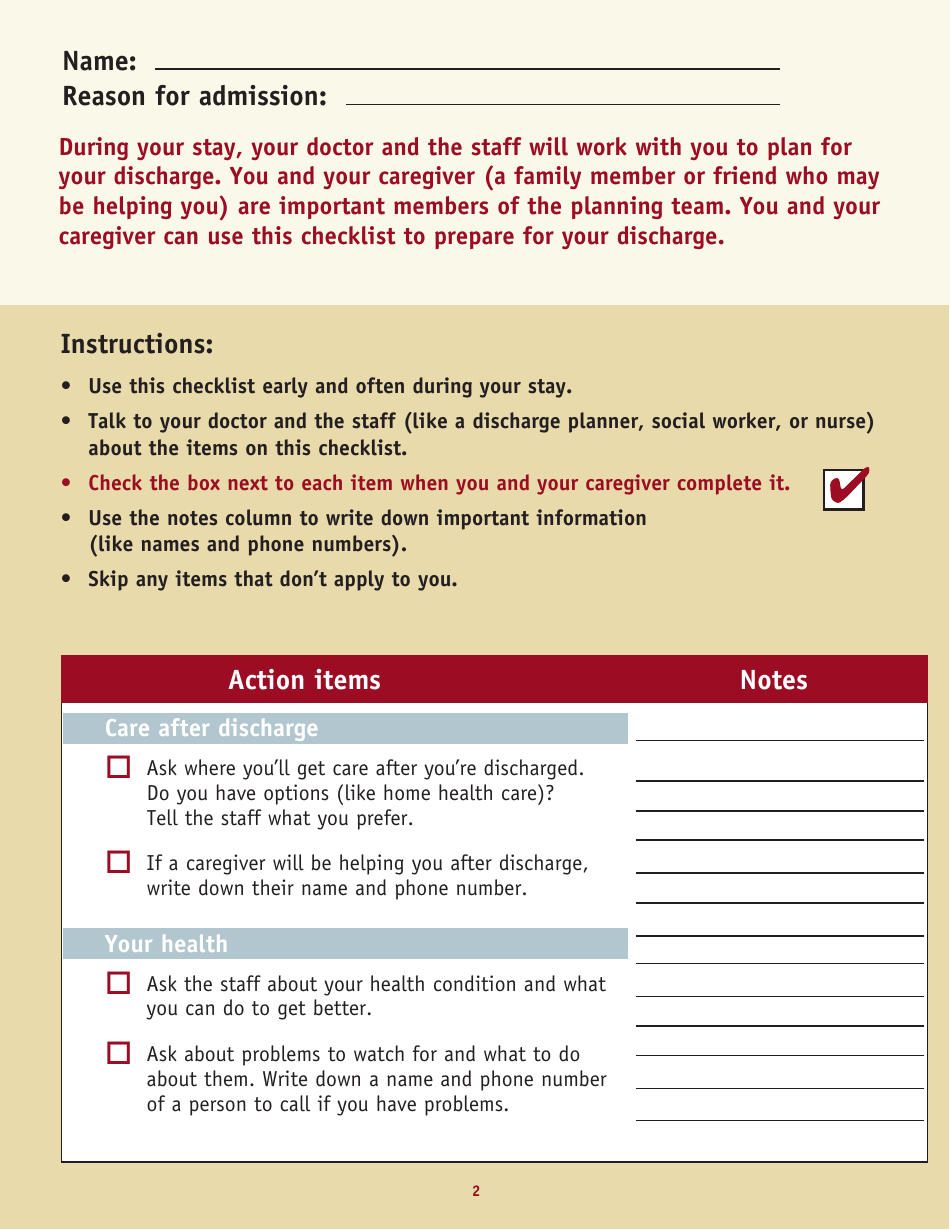
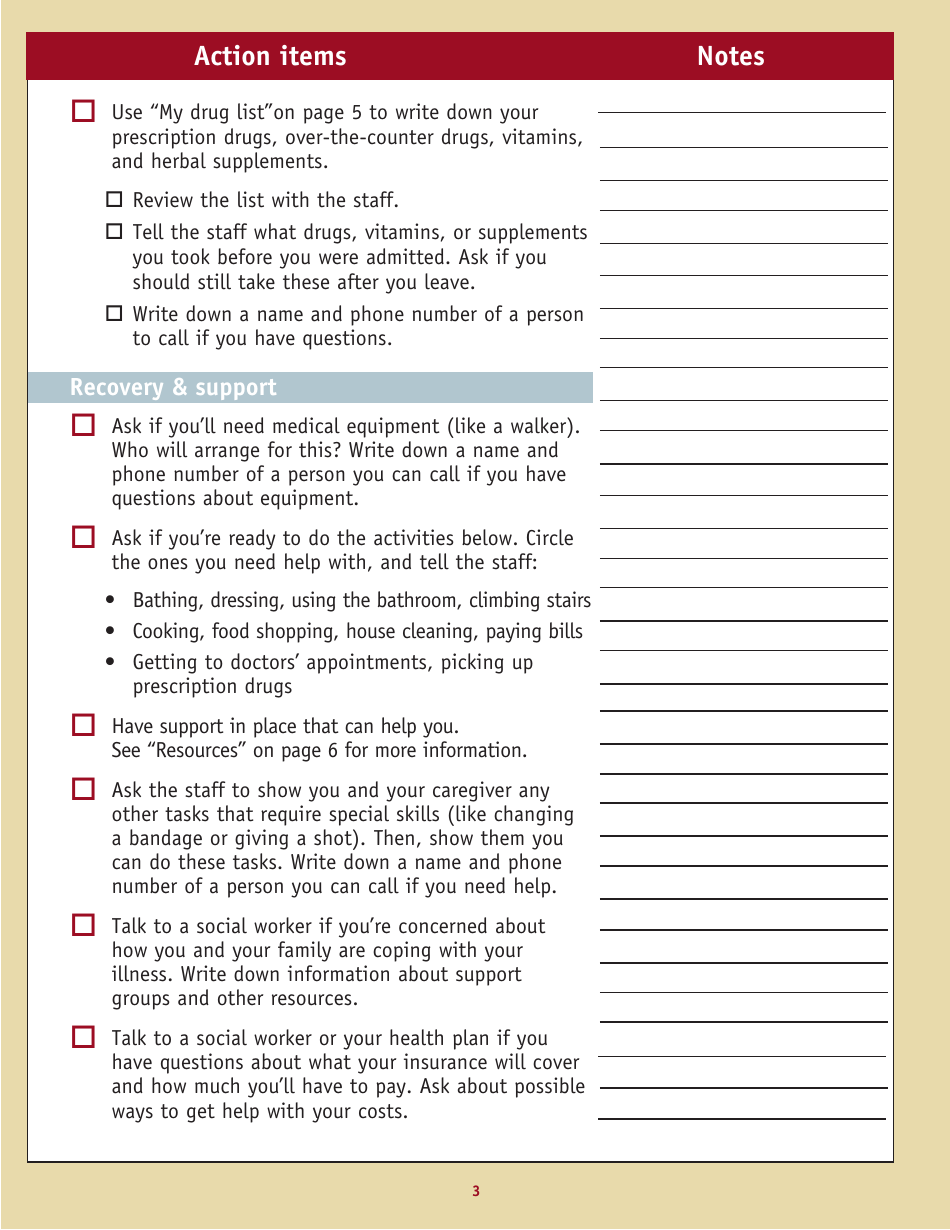
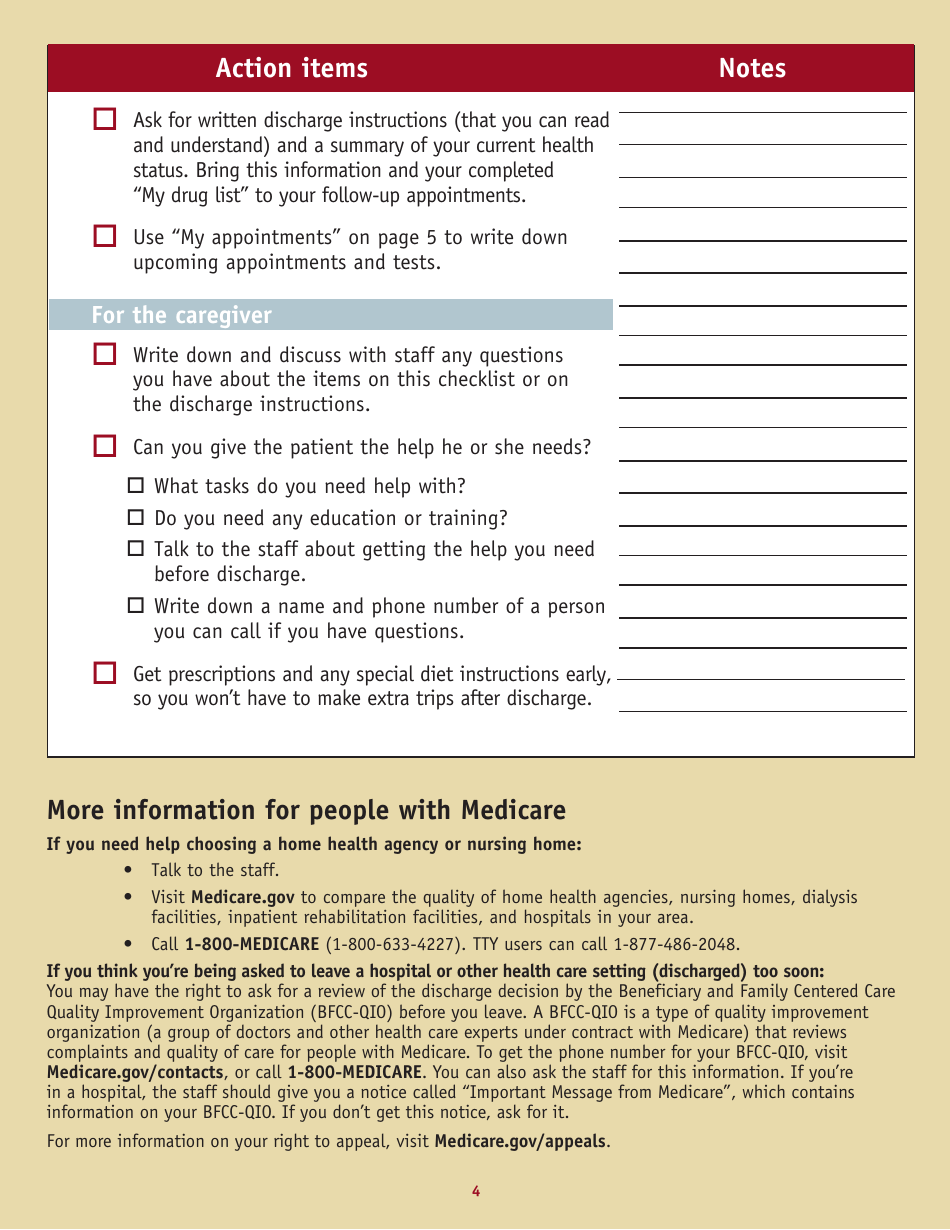
A Discharge Planning Checklist is a tool used to ensure a smooth transition for a patient from hospital care back to their home or another healthcare facility. This checklist is crucial for care coordination and includes information about medication management, appointment scheduling, therapy instructions, dietary concerns, and other aspects of post-hospital care. The primary aim is to promote continuity of care, reduce the chance of readmission, and enhance the patient's overall health and wellbeing after hospitalization.
The Discharge Planning Checklist is typically filed by healthcare providers in hospitals or healthcare facilities. It is part of patient care coordination upon their release from the hospital. The checklist helps ensure that patients can safely manage their health care needs and routines when they return to their homes or move to another healthcare facility. The staff involved can include nurses, social workers, physicians, and other members of the healthcare team.
FAQ
Q: What is a discharge planning checklist?
A: A discharge planning checklist is a tool used by medical professionals which outlines tasks to be completed before a patient is released from the hospital. It can include items such as medication instructions, follow-up appointments, and necessary home care arrangements.
Q: Why is a discharge planning checklist important?
A: The discharge planning checklist is important because it ensures healthcare professionals don't miss any crucial steps in preparing a patient for discharge. It improves patient safety, reduces readmission rates, and facilitates a smooth transition from the hospital to home or another care facility.
Q: What are some common elements found in a discharge planning checklist?
A: Some common elements found in a discharge planning checklist may include: assessment of the patient's healthcare needs after discharge, coordination with home care services if needed, medication reconciliation, scheduling follow-up appointments, and educating the patient and family about the patient’s condition and care instructions.
Q: Who is responsible for completing the discharge planning checklist?
A: The healthcare team is typically responsible for completing the discharge planning checklist. This can include doctors, nurses, social workers, and other healthcare professionals involved in the patient's care.
Q: Can patients and family members contribute to the discharge planning checklist?
A: Yes, input from patients and their family members is crucial in creating an effective discharge plan. Their understanding about the medical condition, responsibilities, and any potential barriers following discharge are important considerations and should be incorporated into the plan.
Q: How is a discharge planning checklist used in the USA?
A: In the USA, a discharge planning checklist is used in all healthcare facilities to ensure the smooth transition of patients from a hospital or another mid-term care facility back to their homes or to another long term care facility. It aims at reducing patient readmission rates and improved patient health outcomes by ensuring they receive the appropriate level and type of care following discharge.