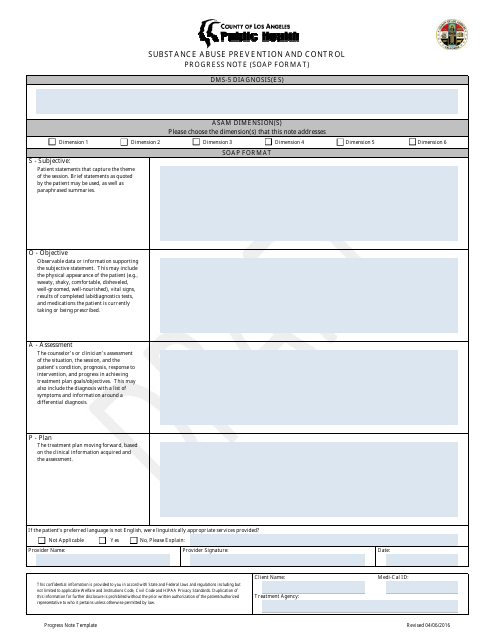
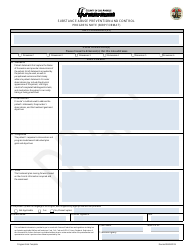
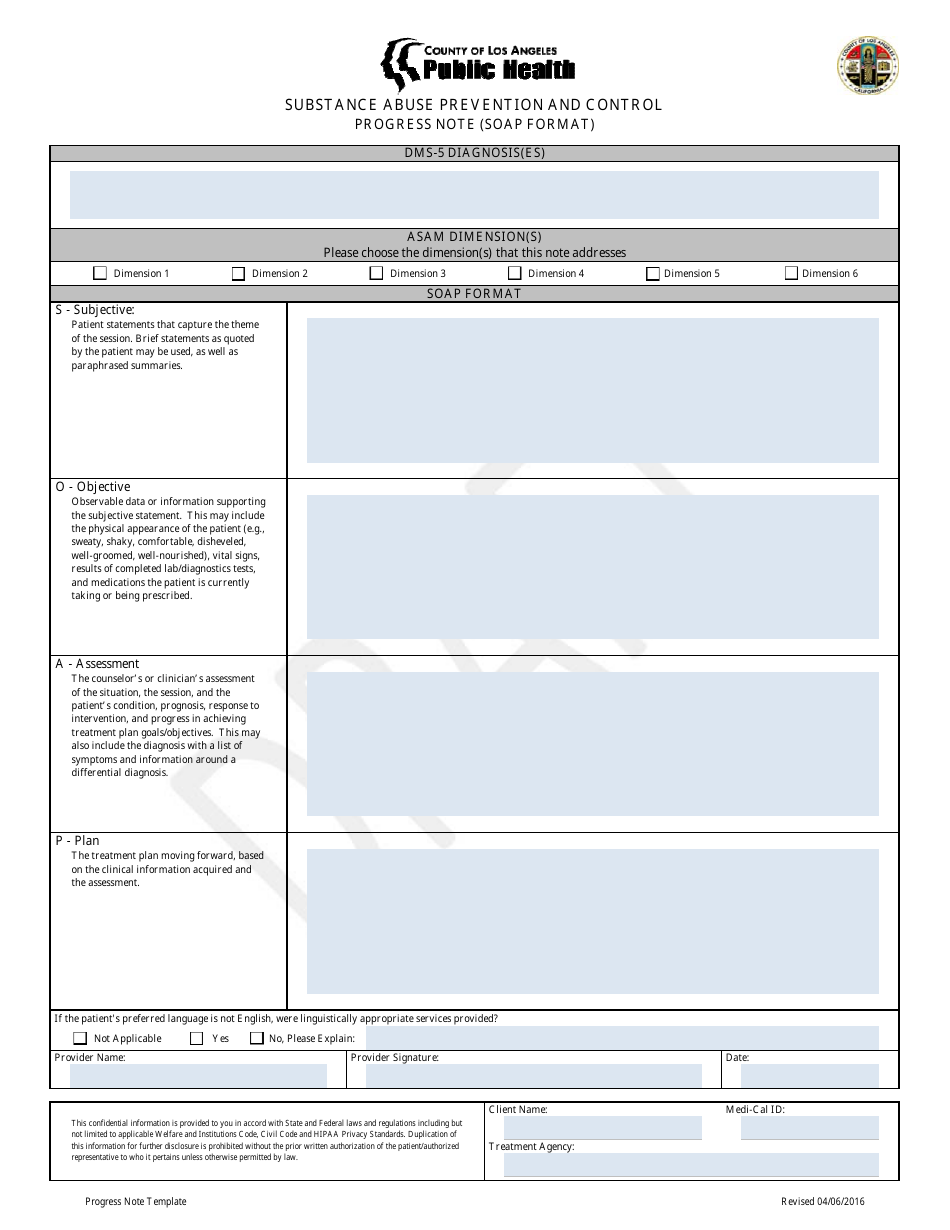
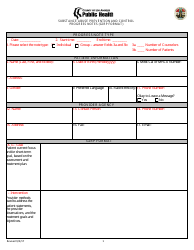
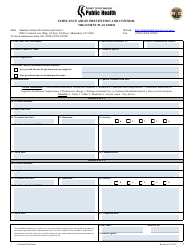
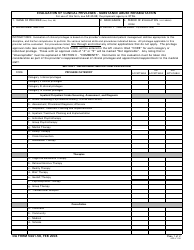
Substance Abuse Prevention and Control Progress Note (Soap Format) - County of Los Angeles, California
Substance Abuse Prevention and Control Progress Note (Soap Format) is a legal document that was released by the Department of Public Health - County of Los Angeles, California - a government authority operating within California. The form may be used strictly within County of Los Angeles.
FAQ
Q: What is the Substance Abuse Prevention and Control Progress Note?
A: The Substance Abuse Prevention and Control Progress Note is a documentation format used in Los Angeles County, California to track the progress of individuals receiving substance abuse treatment.
Q: What is the purpose of the Substance Abuse Prevention and Control Progress Note?
A: The purpose of the Substance Abuse Prevention and Control Progress Note is to monitor and assess the treatment progress, goals, and interventions of individuals receiving substance abuse treatment.
Q: What information is included in the Substance Abuse Prevention and Control Progress Note?
A: The Substance Abuse Prevention and Control Progress Note typically includes information about the client, treatment goals, interventions, progress made, any challenges faced, and plans for future treatment.
Q: Who uses the Substance Abuse Prevention and Control Progress Note?
A: The Substance Abuse Prevention and Control Progress Note is used by substance abuse treatment providers, clinicians, and counselors in Los Angeles County, California.
Q: Why is documenting treatment progress important?
A: Documenting treatment progress is important for tracking the effectiveness of treatment interventions, ensuring client safety, and maintaining transparency and accountability in the treatment process.
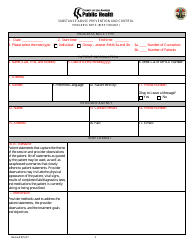
Q: What is the SOAP format?
A: The SOAP format is an acronym for Subjective, Objective, Assessment, and Plan. It is a commonly used structure in healthcare documentation, including the Substance Abuse Prevention and Control Progress Note.
Q: What does the Subjective section of the SOAP format include?
A: The Subjective section of the SOAP format includes subjective information provided by the client, such as their thoughts, feelings, and perceptions about their substance abuse treatment progress.
Q: What does the Objective section of the SOAP format include?
A: The Objective section of the SOAP format includes objective information observed or measured by the treatment provider, such as vital signs, lab results, and observed behaviors.
Q: What does the Assessment section of the SOAP format include?
A: The Assessment section of the SOAP format includes the treatment provider's professional assessment of the client's progress, including any identified issues, barriers, or achievements.
Q: What does the Plan section of the SOAP format include?
A: The Plan section of the SOAP format includes the treatment provider's plan for future treatment, including specific interventions, goals, and follow-up appointments.
Form Details:
- Released on April 6, 2016;
- The latest edition currently provided by the Department of Public Health - County of Los Angeles, California;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Department of Public Health - County of Los Angeles, California.