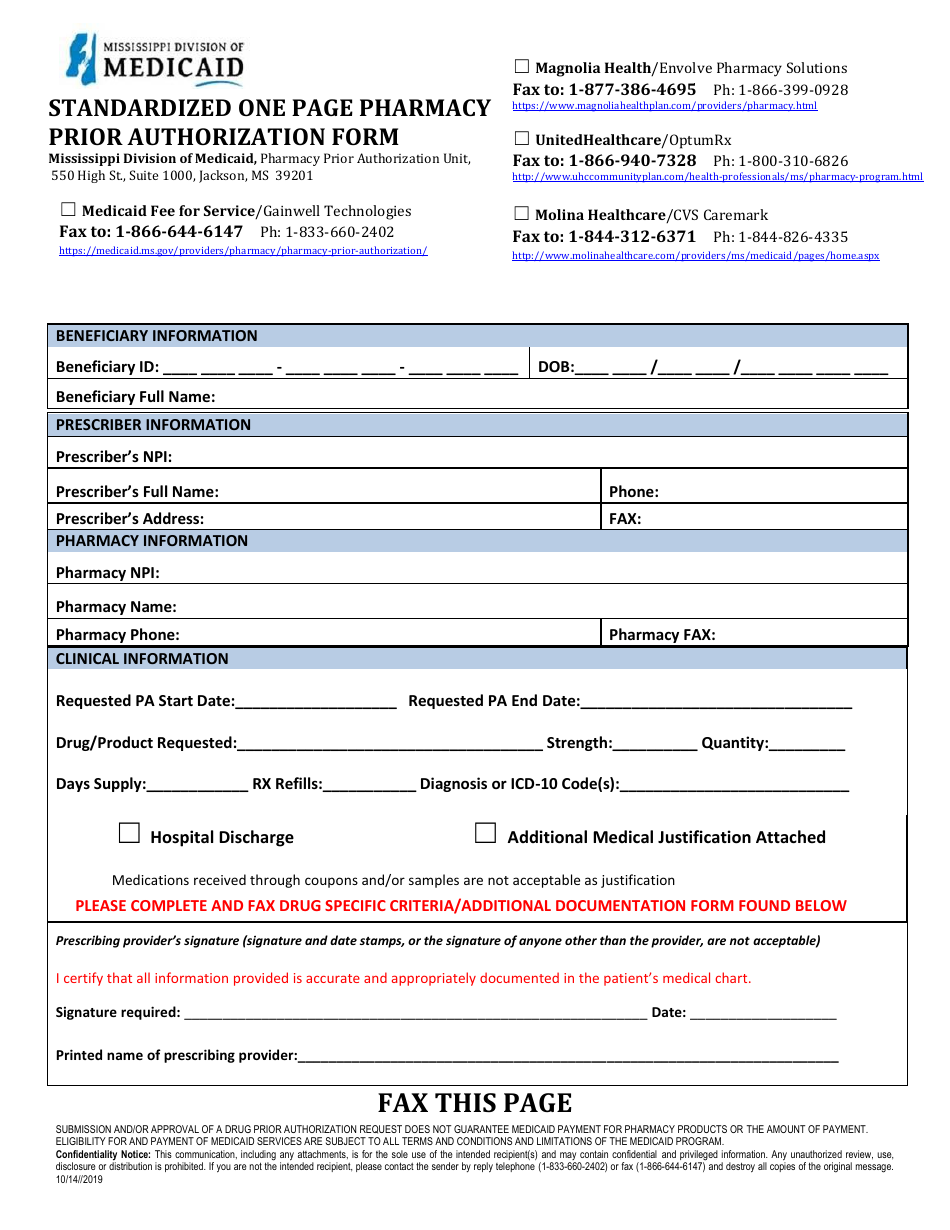
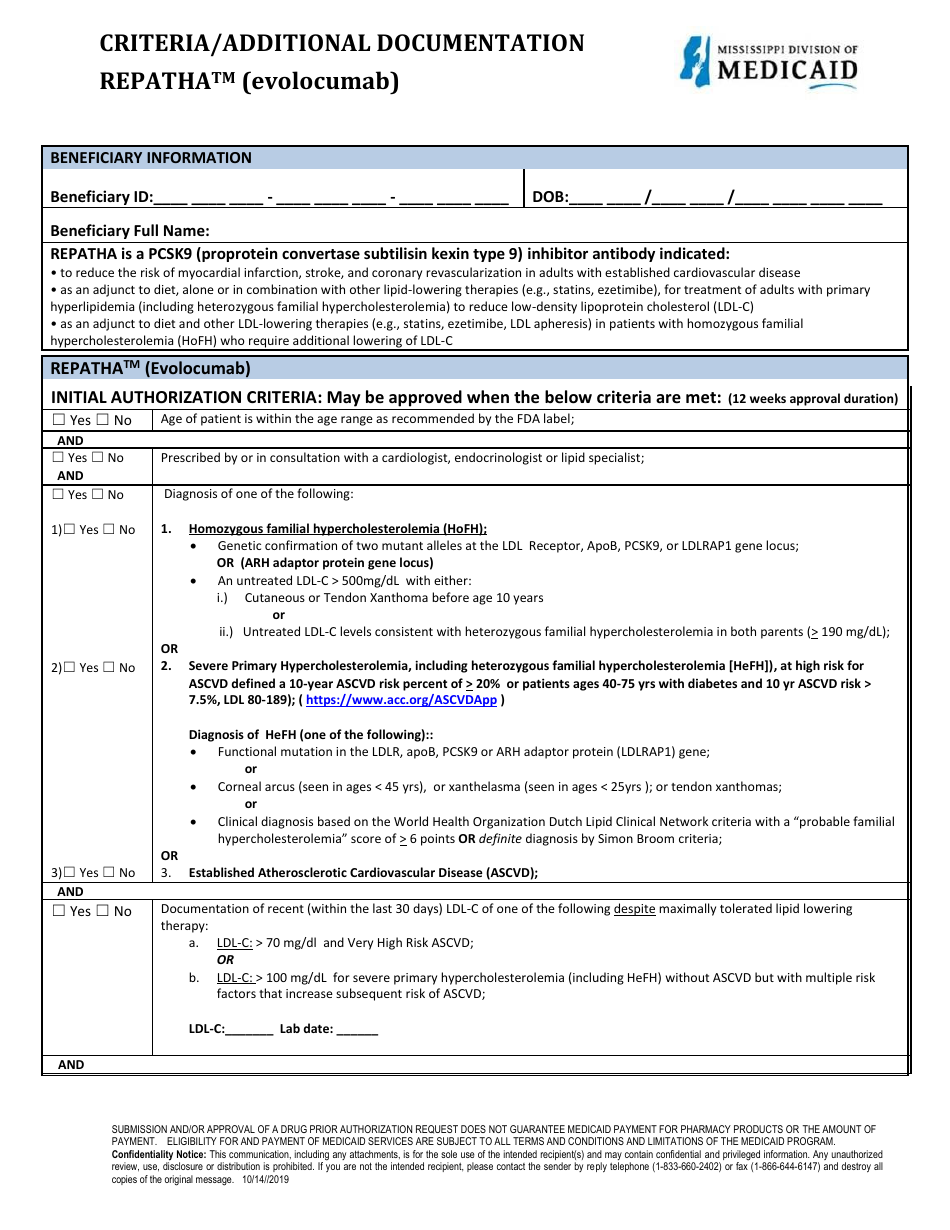
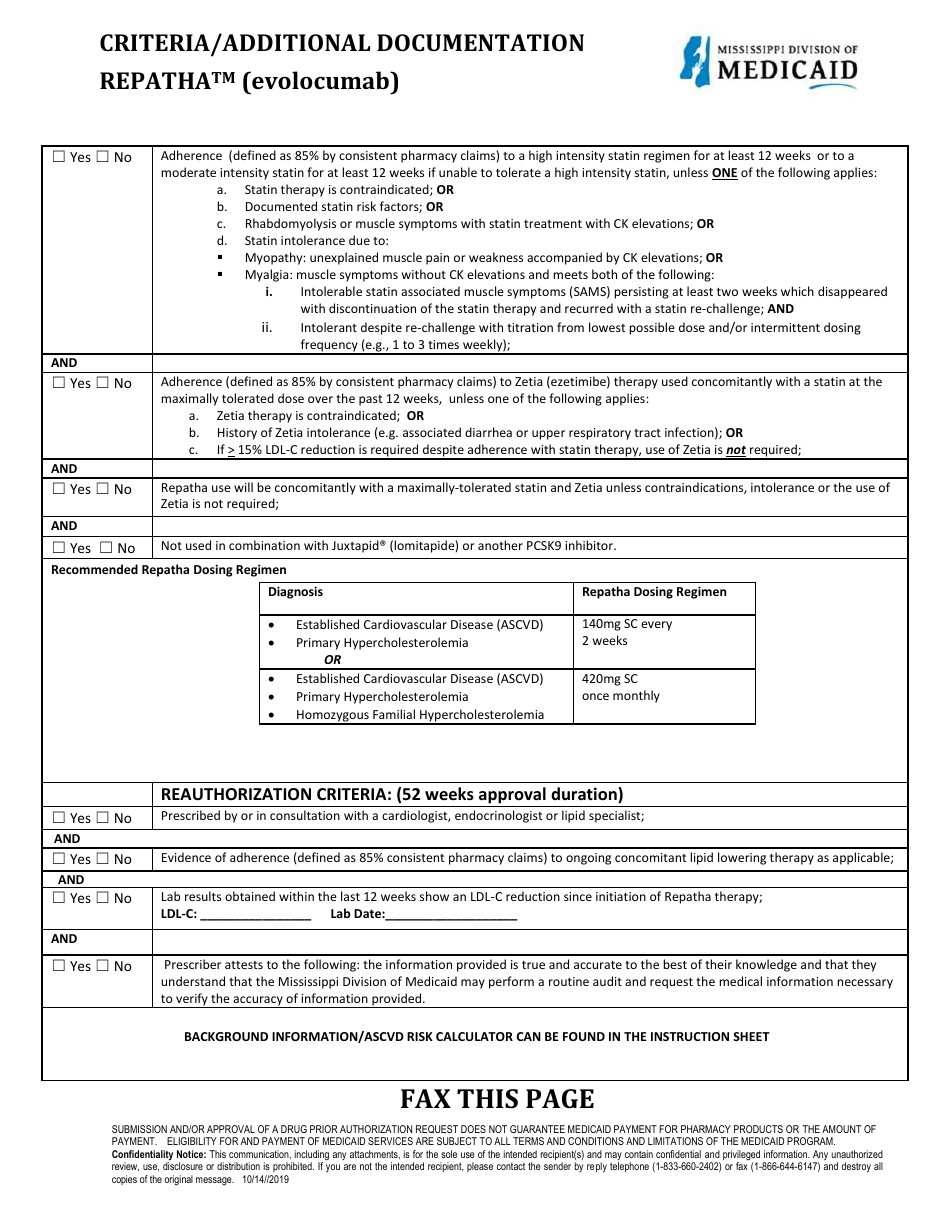
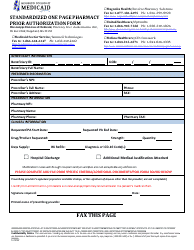
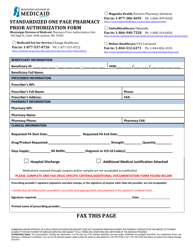
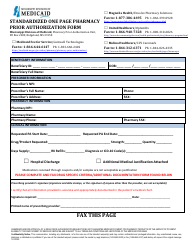
Standardized One Page Pharmacy Prior Authorization Form - Repatha - Mississippi
Standardized One Page Pharmacy Prior Authorization Form - Repatha is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is a pharmacy prior authorization form?
A: A pharmacy prior authorization form is a document that is used by insurance companies to determine if a medication is medically necessary and should be covered.
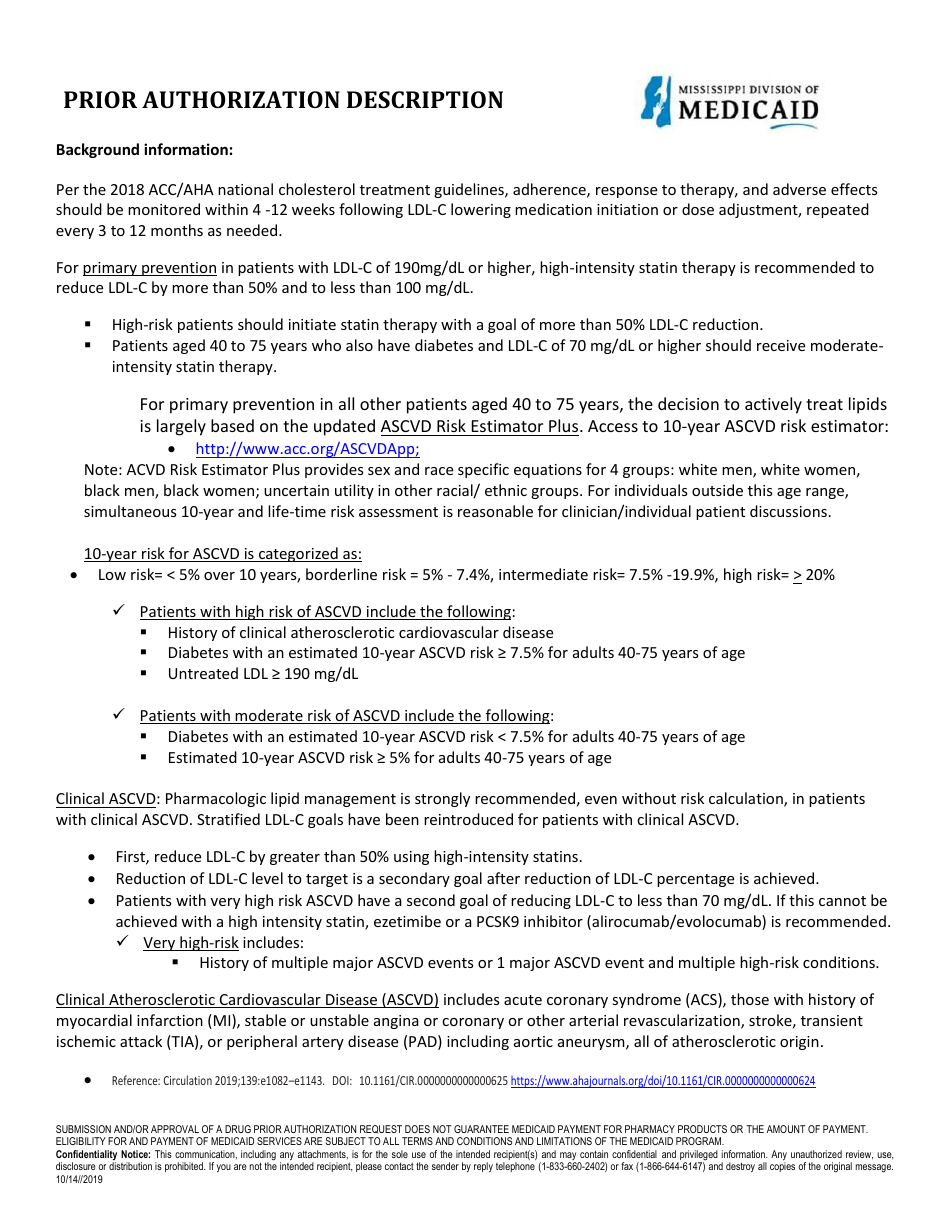
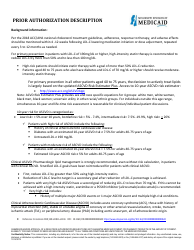
Q: What is Repatha?
A: Repatha is a medication used to treat high cholesterol and reduce the risk of heart attacks and strokes.
Q: Why do I need a prior authorization for Repatha?
A: Insurance companies often require prior authorization for Repatha to ensure that the medication is being used for appropriate patients and that other treatment options have been tried first.
Q: How do I obtain a pharmacy prior authorization form for Repatha in Mississippi?
A: You can obtain a standardized one-page pharmacy prior authorization form for Repatha in Mississippi from your healthcare provider or your insurance company.
Q: What information is required on the pharmacy prior authorization form?
A: The form typically requires information such as the patient's name, insurance information, prescribing healthcare provider's information, diagnosis, and supporting documentation.
Q: How long does it take to get a prior authorization for Repatha?
A: The time it takes to get a prior authorization for Repatha varies depending on the insurance company, but it usually takes a few days to a couple of weeks.
Q: What happens after I submit the pharmacy prior authorization form?
A: After you submit the form, the insurance company will review the information and make a decision on whether to approve or deny the prior authorization request.
Q: What should I do if the prior authorization is denied?
A: If the prior authorization for Repatha is denied, you can appeal the decision with your insurance company and provide additional supporting documentation if necessary.
Q: Is there a fee for obtaining a pharmacy prior authorization for Repatha?
A: There is usually no fee associated with obtaining a pharmacy prior authorization form for Repatha, but it is best to check with your insurance company to confirm.
Q: Can I get assistance with the prior authorization process?
A: Yes, you can often get assistance with the prior authorization process from your healthcare provider's office or your insurance company's customer service department.
Form Details:
- Released on October 14, 2019;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.