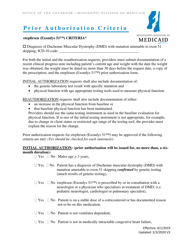
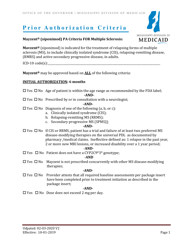
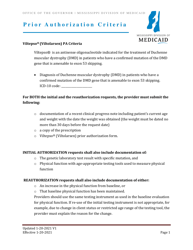
Prior Authorization Criteria - Kalydeco (Ivacaftor) - Mississippi
Prior Authorization Criteria - Kalydeco (Ivacaftor) is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is Kalydeco?
A: Kalydeco is a medication also known as Ivacaftor.
Q: What is Ivacaftor?
A: Ivacaftor is the generic name for the medication Kalydeco.
Q: What is prior authorization?
A: Prior authorization is a process where a healthcare provider needs approval from an insurance company before prescribing a certain medication.
Q: Why is prior authorization required?
A: Prior authorization is required to ensure the medication is medically necessary and is covered by the insurance plan.
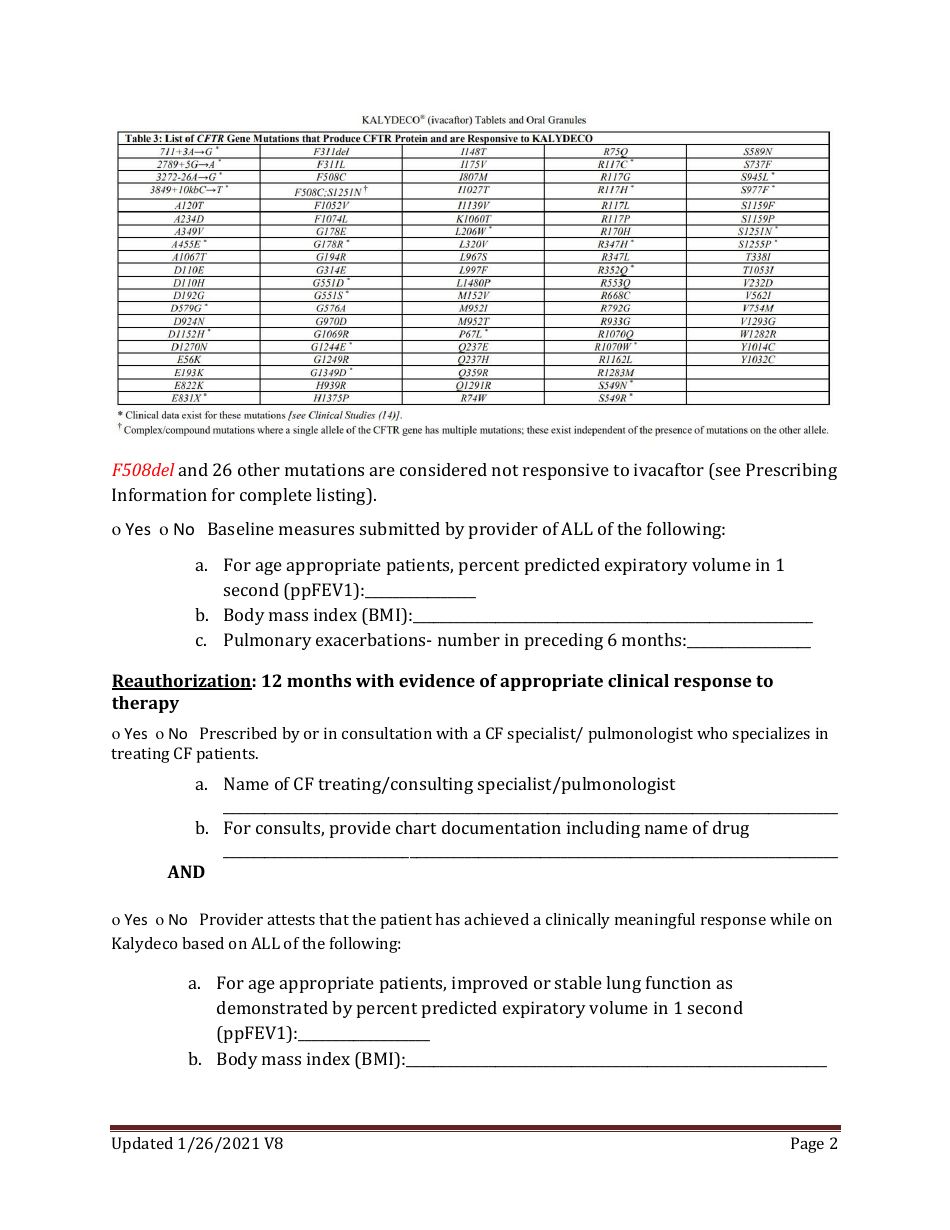
Q: What are the criteria for prior authorization for Kalydeco in Mississippi?
A: The specific criteria for Kalydeco prior authorization in Mississippi may vary. It is recommended to check with the insurance company or healthcare provider for the most up-to-date requirements.
Q: Are there any restrictions on Kalydeco?
A: There may be restrictions on Kalydeco depending on the insurance plan. It is best to consult with the insurance company or healthcare provider to understand the coverage and restrictions.
Q: Is Kalydeco covered by insurance?
A: Kalydeco may be covered by insurance, but coverage can vary depending on the insurance plan. It is important to check with the insurance company to verify coverage.
Q: How can I get prior authorization for Kalydeco?
A: To get prior authorization for Kalydeco, you will need to contact your healthcare provider and insurance company. They will guide you through the process and provide the necessary forms and information.
Q: What if my insurance doesn't cover Kalydeco?
A: If your insurance doesn't cover Kalydeco, you may explore other options such as patient assistance programs, manufacturer's discounts, or appealing the insurance company's decision.
Q: Can I appeal a prior authorization denial for Kalydeco?
A: Yes, you can appeal a prior authorization denial for Kalydeco. The appeal process will vary depending on the insurance company. It is recommended to consult with your healthcare provider and insurance company for guidance.
Form Details:
- Released on January 26, 2021;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.