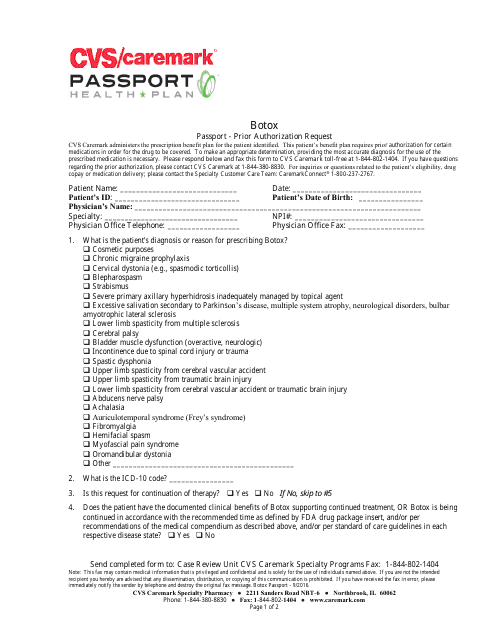
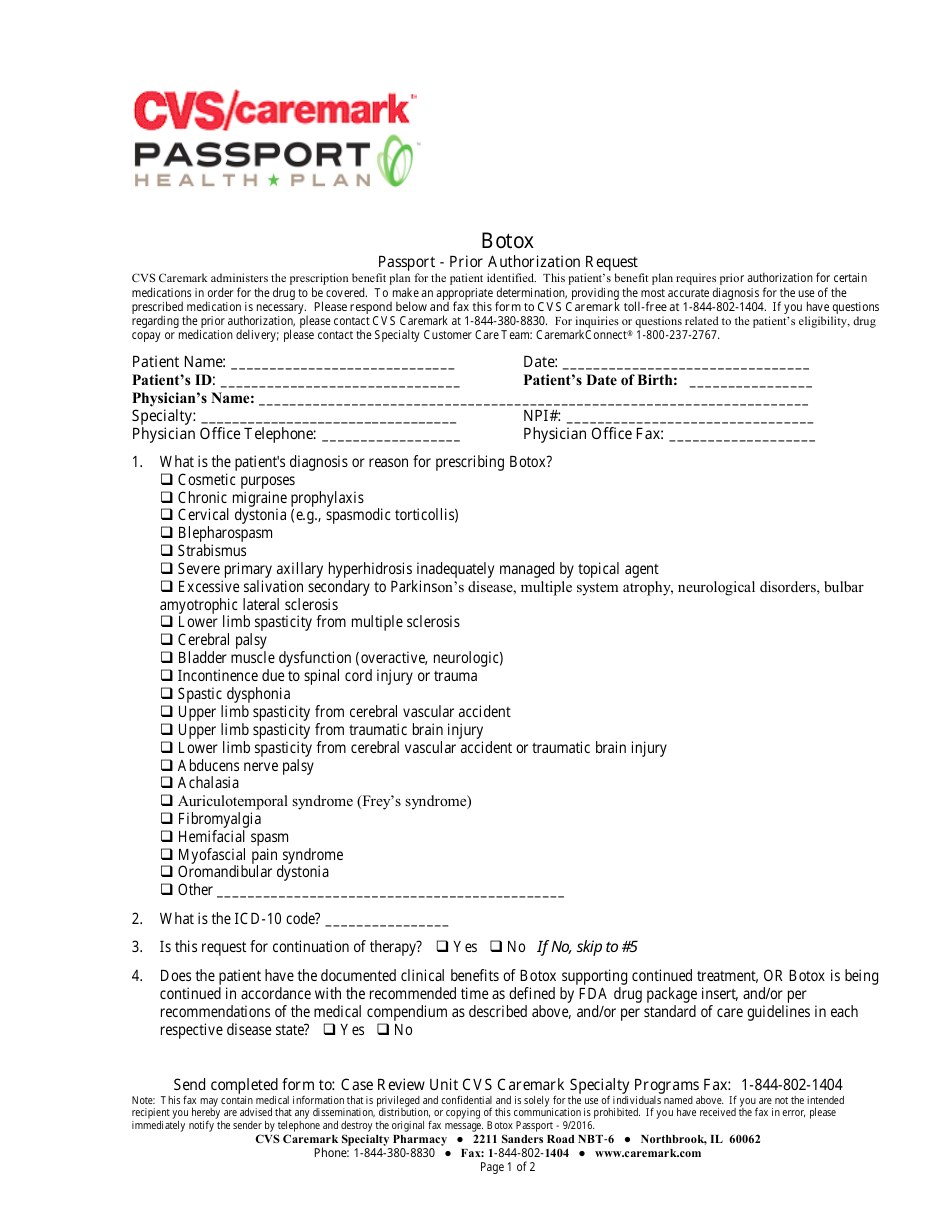
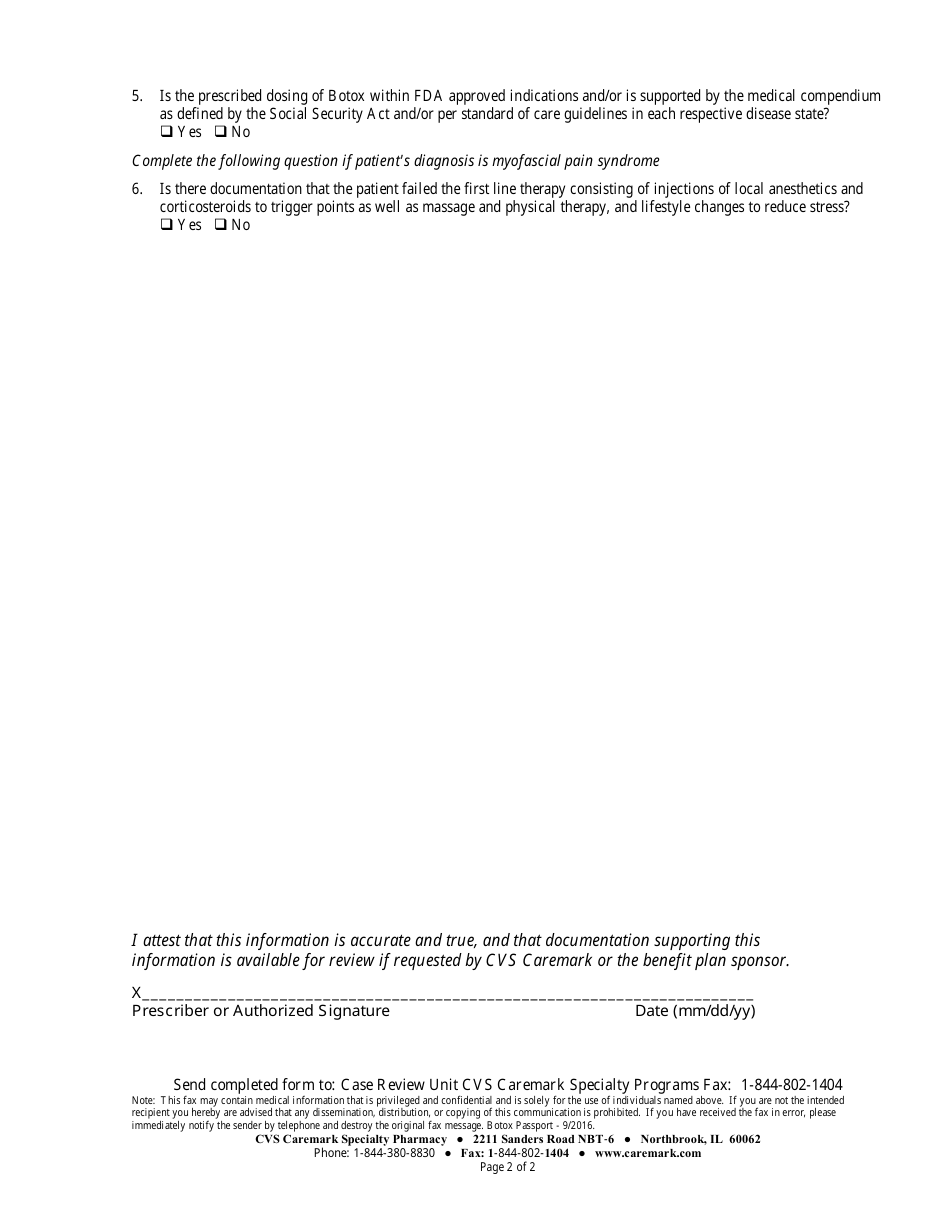
Botox Passport - Prior Authorization Request Form - Cvs Caremark
The Botox Passport - Prior Authorization Request Form is used by CVS Caremark for obtaining prior authorization for Botox treatments. It is a necessary document to be completed and submitted to CVS Caremark in order to request coverage for Botox injections.
FAQ
Q: What is the Botox Passport?
A: The Botox Passport is a prior authorization request form.
Q: Who is it for?
A: It is for individuals seeking prior authorization for Botox treatments.
Q: What is prior authorization?
A: Prior authorization is a process where approval is needed from an insurer before certain medications or treatments are covered.
Q: What is CVS Caremark?
A: CVS Caremark is a pharmacy benefits manager that handles prescription drug plans for various health insurance companies.
Q: Why would I need prior authorization for Botox?
A: Many insurance companies require prior authorization for Botox and other similar treatments to ensure medical necessity and appropriate use.
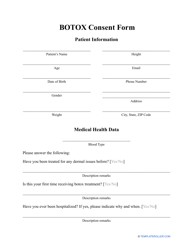
Q: How do I fill out the Botox Passport form?
A: You need to provide information about the patient, healthcare provider, diagnosis, treatment plan, and other relevant details as requested in the form.
Q: What happens after I submit the Botox Passport form?
A: The form will be reviewed by CVS Caremark to determine if prior authorization is approved.
Q: How long does the prior authorization process take?
A: The duration may vary, but it typically takes a few days to a few weeks for the prior authorization process to be completed.
Q: Is prior authorization guaranteed?
A: No, prior authorization is not guaranteed. Approval is subject to review and evaluation of the submitted information.
Q: Do I need to submit the Botox Passport form for every treatment?
A: Yes, you will need to submit the form for each Botox treatment that requires prior authorization.
Q: Can I appeal if my prior authorization request is denied?
A: Yes, you have the option to appeal the decision if your prior authorization request is denied. Contact CVS Caremark for more information on the appeals process.