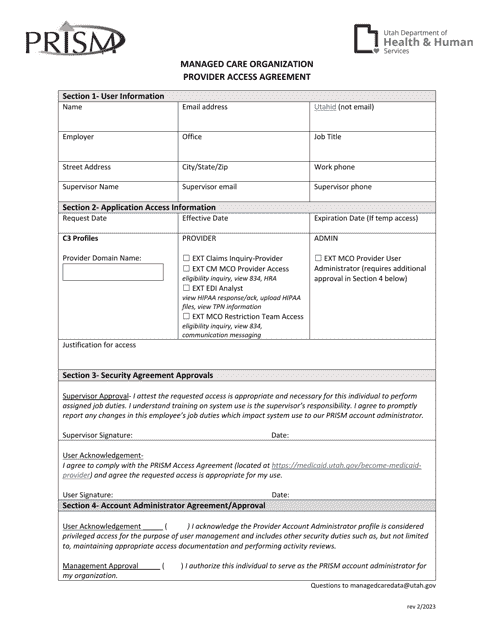
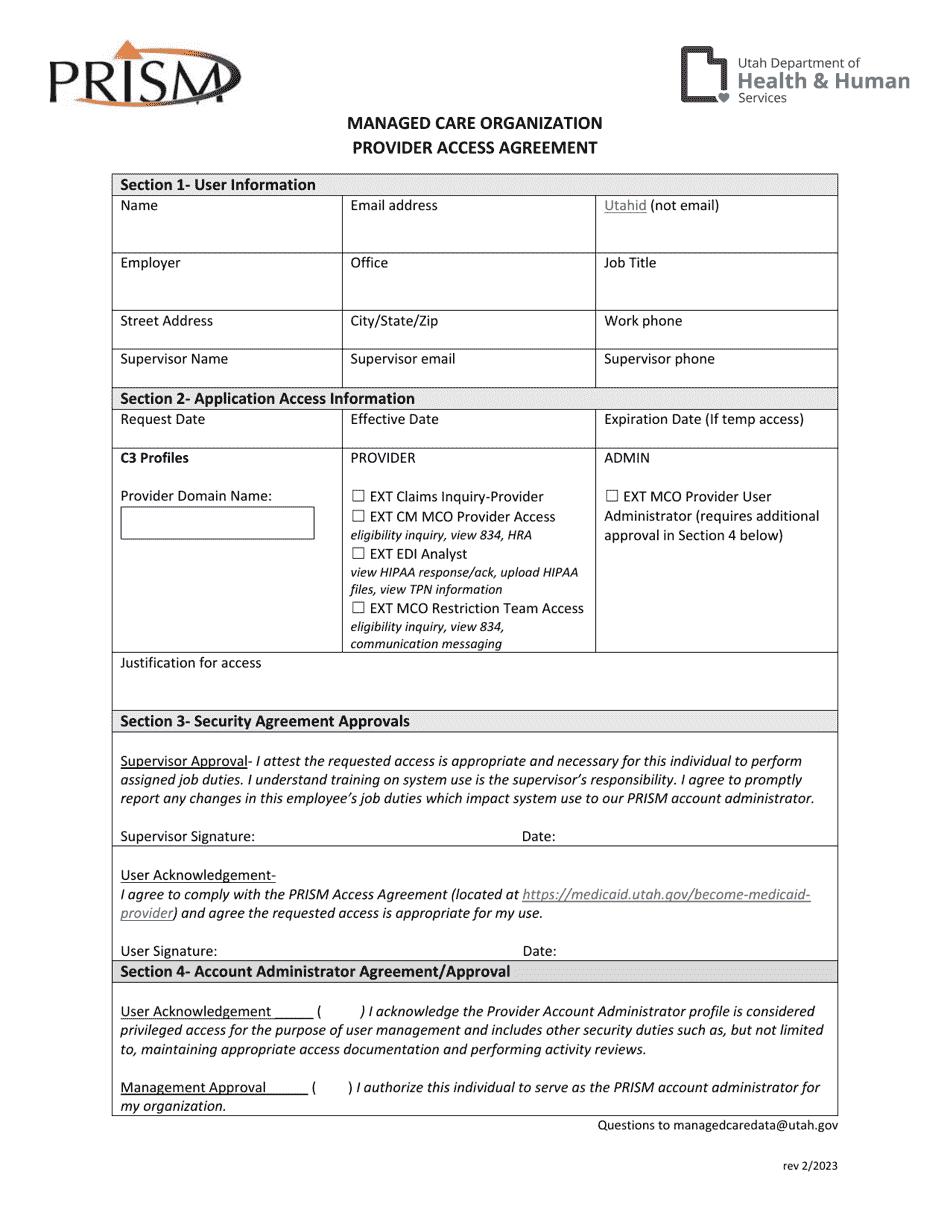
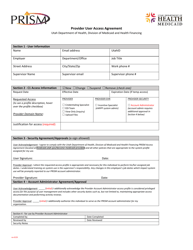
Managed Care Organization Provider Access Agreement - Utah
Managed Care Organization Provider Access Agreement is a legal document that was released by the Utah Department of Health and Human Services - a government authority operating within Utah.
FAQ
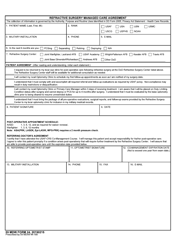
Q: What is a Managed Care Organization (MCO)?
A: A Managed Care Organization (MCO) is a healthcare provider that coordinates and manages the healthcare services for a group of people.
Q: What is a Provider Access Agreement?
A: A Provider Access Agreement is a legal contract between a healthcare provider and a Managed Care Organization (MCO) that outlines the terms and conditions for the provider's participation in the MCO's network.
Q: Why is a Provider Access Agreement important?
A: A Provider Access Agreement is important as it sets forth the rights, obligations, and expectations of both the healthcare provider and the Managed Care Organization (MCO) in their working relationship.
Q: What does a Provider Access Agreement typically include?
A: A Provider Access Agreement typically includes details about reimbursement rates, service requirements, quality standards, confidentiality, termination clauses, and dispute resolution procedures.
Q: How can a healthcare provider join a Managed Care Organization's (MCO) network?
A: To join a Managed Care Organization (MCO)'s network, a healthcare provider typically needs to sign a Provider Access Agreement and meet the MCO's eligibility criteria.
Q: Are healthcare providers required to participate in a Managed Care Organization's (MCO) network?
A: Participation in a Managed Care Organization (MCO) network is typically voluntary for healthcare providers, although some providers may choose to join to increase their patient base and access to insurance reimbursements.
Form Details:
- Released on February 1, 2023;
- The latest edition currently provided by the Utah Department of Health and Human Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Utah Department of Health and Human Services.