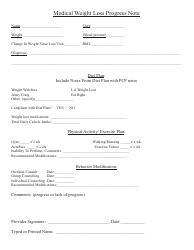
Doctor's Note to Return to Work
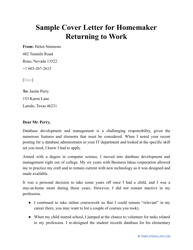
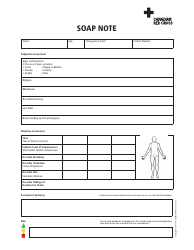
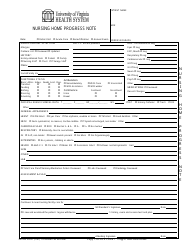
A Doctor's Note to Return to Work is typically used when an employee has been on medical leave and needs authorization from a healthcare professional to resume their responsibilities. It confirms that the employee is healthy enough to return to work and provides a timeline for their recovery.
In most cases, it is the responsibility of the employee to provide the doctor's note to their employer when they are ready to return to work.
FAQ
Q: What is a doctor's note to return to work?
A: A doctor's note to return to work is a document provided by a healthcare professional that certifies an individual's ability to resume work after a period of illness or injury.
Q: Why would I need a doctor's note to return to work?
A: You may need a doctor's note to return to work if your employer requires medical documentation to confirm that you are fit to resume your duties.
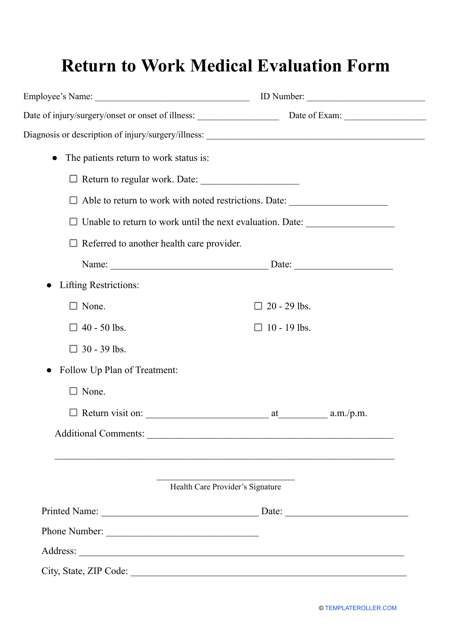
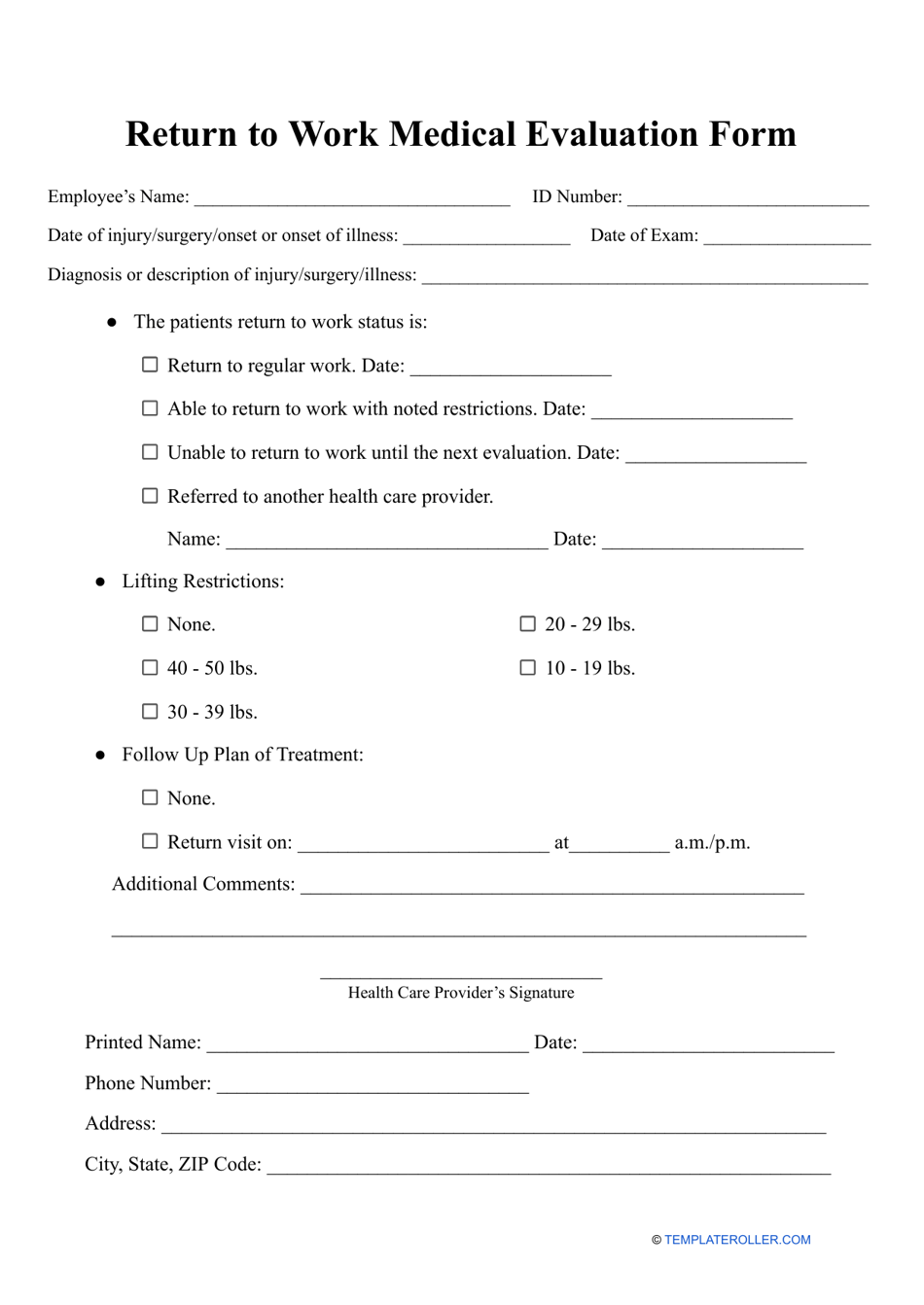
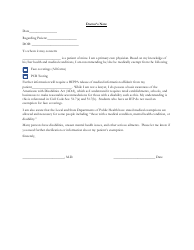
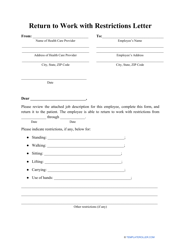
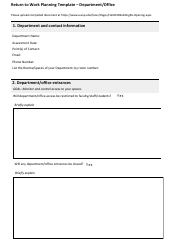
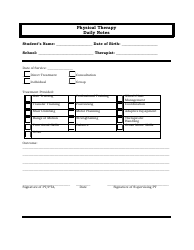
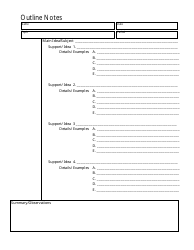
Q: What should be included in a doctor's note to return to work?
A: A doctor's note to return to work should include the date, the healthcare provider's contact information, the dates of the medical leave, the reason for the leave, and a statement indicating your fitness to return to work.
Q: How long does a doctor's note to return to work typically cover?
A: The duration covered by a doctor's note to return to work depends on the specific circumstances and the healthcare provider's assessment. It can range from a few days to several weeks.
Q: Can my employer request additional information besides a doctor's note?
A: Yes, your employer may request additional information or documentation if they have specific policies or legal requirements. However, they should do so in a manner consistent with privacy and employment laws.