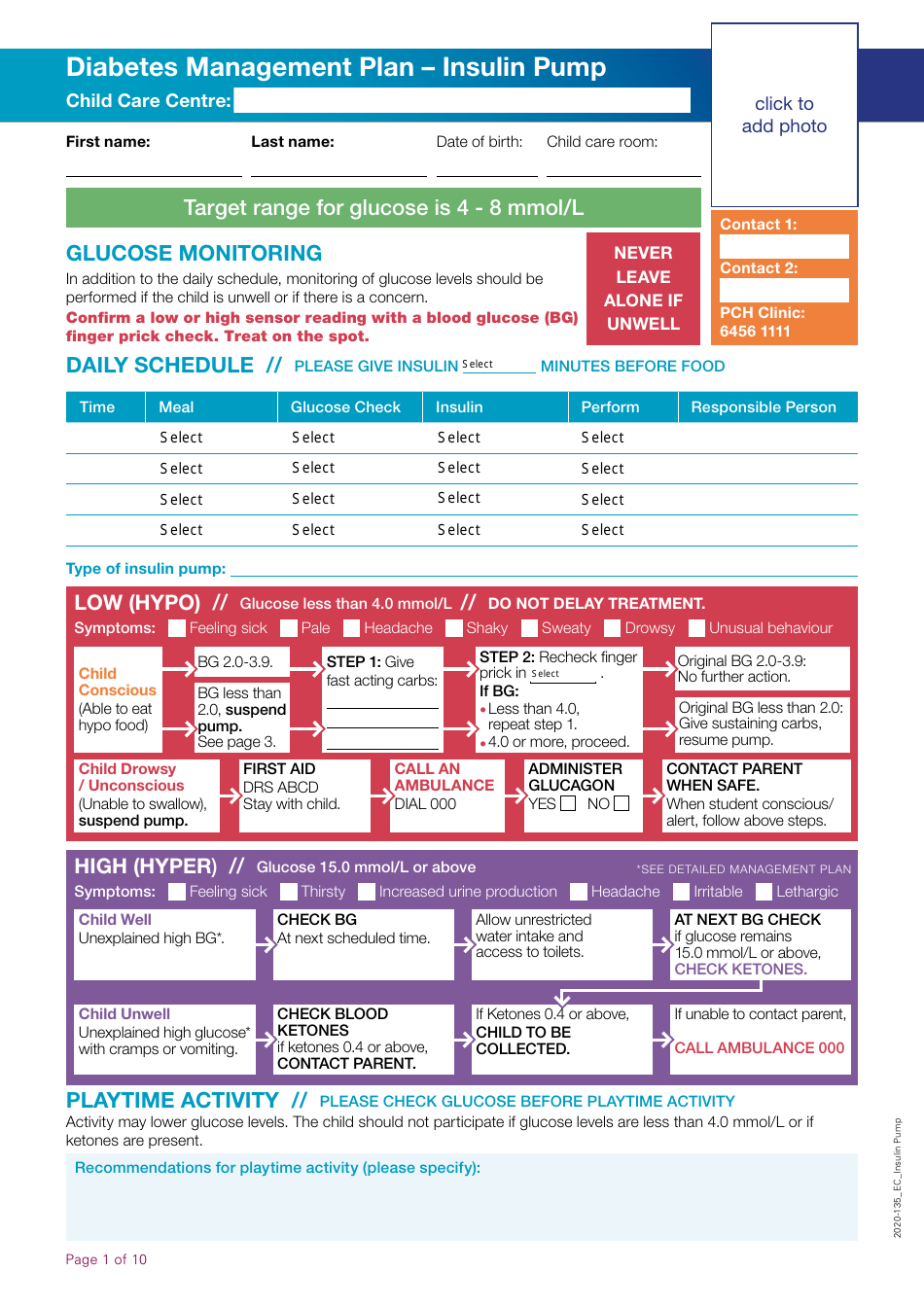
Diabetes Management Plan - Insulin Pump
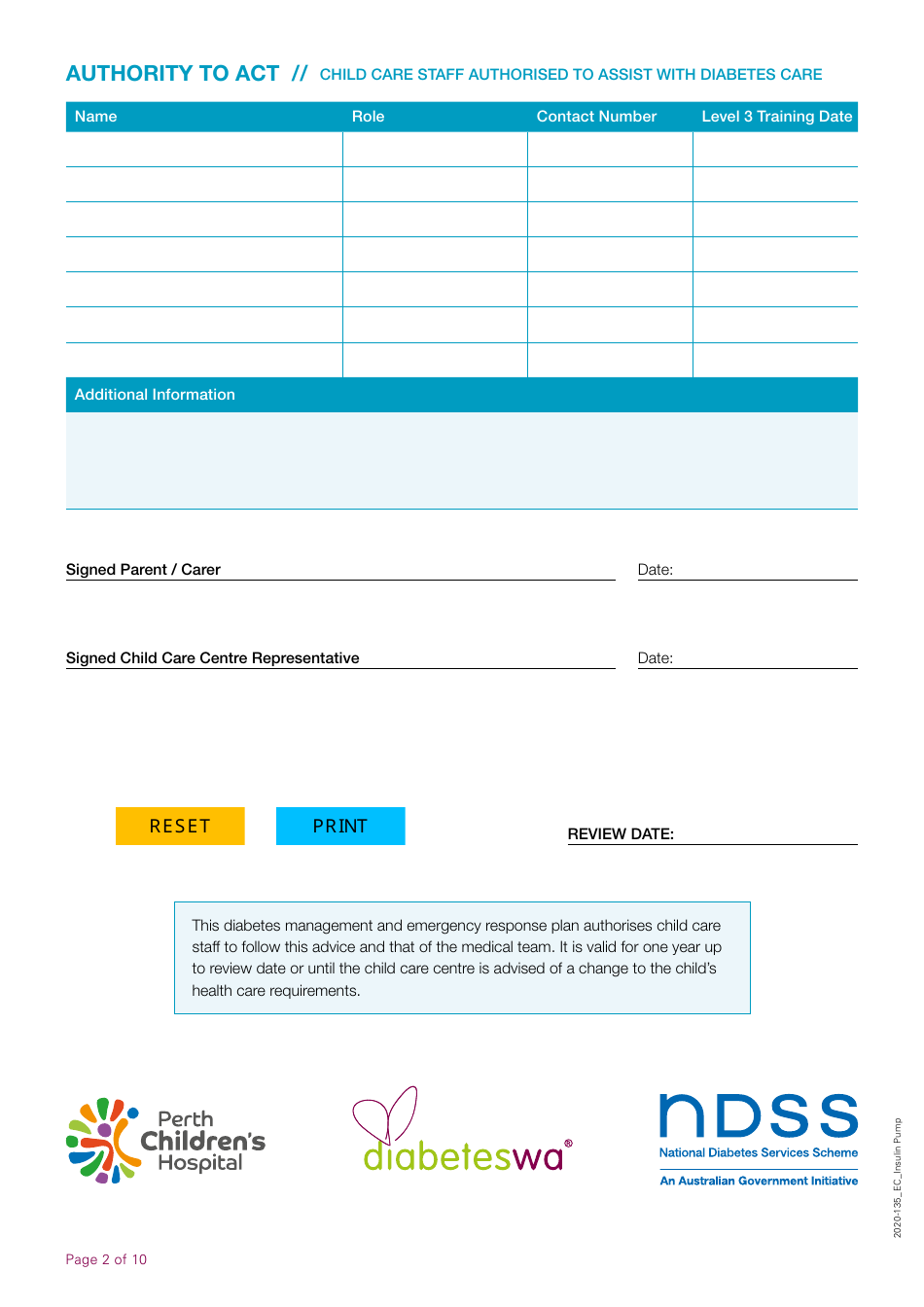
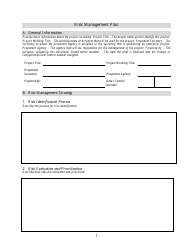
The Diabetes Management Plan - Insulin Pump is a document generally devised by healthcare professionals that outlines effective management strategies for individuals who are using an insulin pump for their diabetes. This plan typically includes details like the individual's scheduled insulin doses, their meal plans, their exercise regimen as well as instructions on what to do during emergencies, how to manage blood sugar levels, and when and how to use the insulin pump. This document is designed to control and manage blood sugar levels and to ensure the user is using the insulin pump correctly, minimizing potential risks and complications associated with diabetes.
The Diabetes Management Plan - Insulin Pump is typically filed by the patient's healthcare provider, which may include a primary care physician, endocrinologist, diabetes educator or nurse. The plan outlines the detailed management strategy for a patient with diabetes who is using an insulin pump. This will include information about medication dosage, monitoring blood sugar levels, diet, and exercise. It aids in ensuring that the patient receives consistent and effective diabetes care. This document is usually shared with the patient and their caregivers to understand and manage the condition effectively. However, the actual process can vary based on the healthcare system of different countries. For instance, in countries like the USA or Canada, the process might be led by a healthcare team whereas, in countries like India and Australia, it could also involve local diabetes educational organizations.
FAQ
Q: What is an insulin pump?
A: An insulin pump is a small device that delivers insulin into your body. It is used as a part of a diabetes management plan to control blood sugar levels in people with insulin-dependent diabetes.
Q: How does an insulin pump work?
A: An insulin pump works by delivering insulin to your body in two ways: basal rate and bolus dose. The basal rate is a continuous, small dose of insulin that's delivered throughout the day. The bolus dose is a larger dose delivered before meals to cover the rise in blood sugar that occurs after eating.
Q: Are insulin pumps effective for diabetes management?
A: Yes, insulin pumps can be an effective tool for managing diabetes. They allow for more precise control of insulin doses and can lead to improved blood sugar control. However, they require careful management and education to use correctly.
Q: What are the benefits of an insulin pump?
A: Insulin pumps offer several benefits such as more precise control over insulin dosing, flexibility in lifestyle, potentially better blood sugar control, and fewer injections.
Q: What are the potential risks or drawbacks of an insulin pump?
A: Some potential risks or drawbacks include the chance of insulin pump malfunctions leading to high or low blood sugars, the risk of infection at the infusion site, the costs, and the need for continuous self management and monitoring.
Q: Does insurance cover insulin pumps in the USA?
A: Most insurance plans in the USA, including Medicare and Medicaid, do cover insulin pumps under durable medical equipment. However, coverage may vary and it's best to check directly with your insurance provider.
Q: Who can use an insulin pump?
A: Insulin pumps can be used by people of all ages who have insulin-dependent diabetes. Doctors usually suggest it for patients with type 1 diabetes and sometimes for those with type 2 diabetes who are not achieving their blood glucose targets with multiple daily injections.
Q: Do all people with Diabetes need an insulin pump?
A: No, not everyone with diabetes needs an insulin pump. The need for an insulin pump depends on various factors such as the type and severity of diabetes, blood sugar control, lifestyle, and patient's willingness and capability to use the device.
Q: Are insulin pumps a one-time purchase?
A: No, while the insulin pump itself may be a one-time purchase, there are ongoing costs for supplies like insulin, infusion sets, batteries, etc.
Q: Can insulin pumps be removed?
A: Yes, insulin pumps can be removed temporarily for activities where it might get wet like swimming or showering, or when playing contact sports. However, it's important to reconnect it again to keep getting insulin.