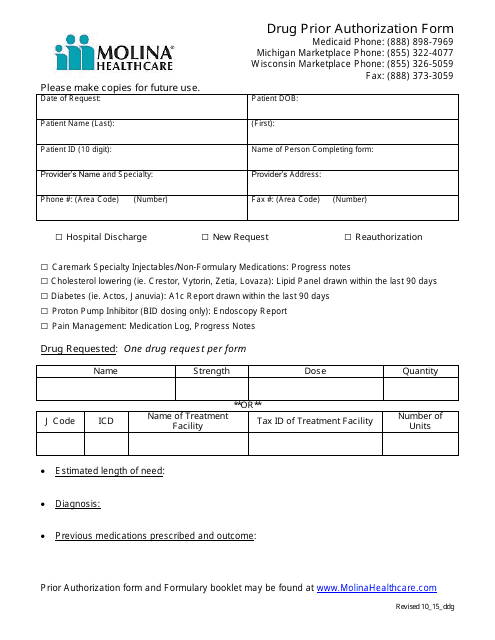
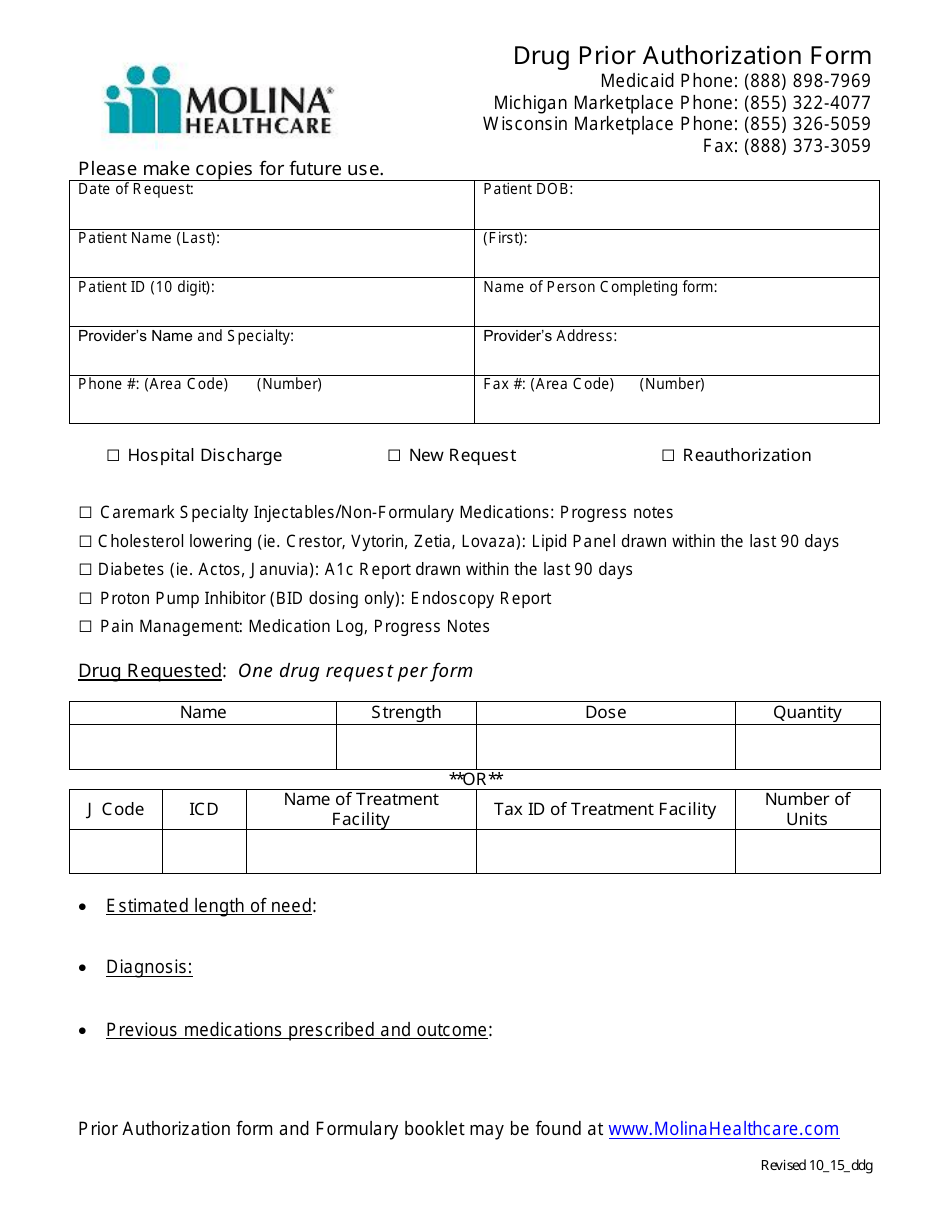
Drug Prior Authorization Form - Molina Healthcare
A Drug Prior Authorization Form for Molina Healthcare is used to request approval from the insurance company for coverage of a specific medication. It helps ensure that the medication prescribed is appropriate and necessary before it is covered by insurance.
FAQ
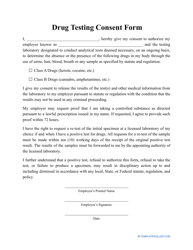
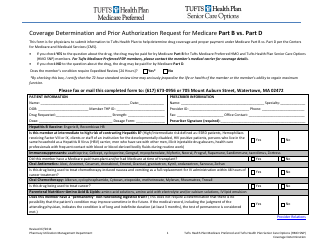
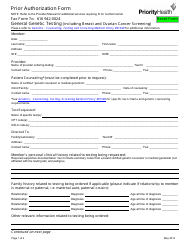
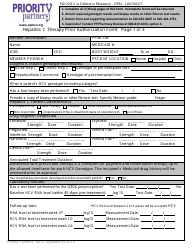
Q: What is a drug prior authorization form?
A: A drug prior authorization form is a request for approval from your healthcare provider to prescribe a specific medication.
Q: Why do I need a drug prior authorization form?
A: You may need a drug prior authorization form to ensure that the medication you need is covered by your insurance and to avoid any out-of-pocket costs.
Q: How do I obtain a drug prior authorization form?
A: You can obtain a drug prior authorization form from your healthcare provider or your insurance company.
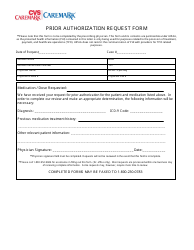
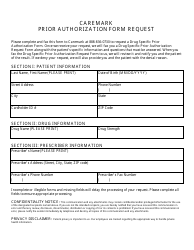
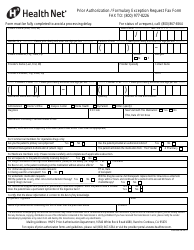
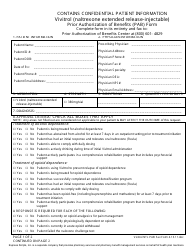
Q: What information is required on a drug prior authorization form?
A: A drug prior authorization form typically requires information such as the medication name, dosage, diagnosis, and supporting medical documentation.
Q: What happens after I submit a drug prior authorization form?
A: After you submit a drug prior authorization form, your healthcare provider's request will be reviewed by the insurance company to determine if the medication is medically necessary and covered by your insurance.
Q: How long does it take for a drug prior authorization form to be approved?
A: The time it takes for a drug prior authorization form to be approved can vary, but typically it can take a few days to a few weeks.
Q: What should I do if my drug prior authorization form is denied?
A: If your drug prior authorization form is denied, you can work with your healthcare provider to explore alternative medications or appeal the denial with your insurance company.