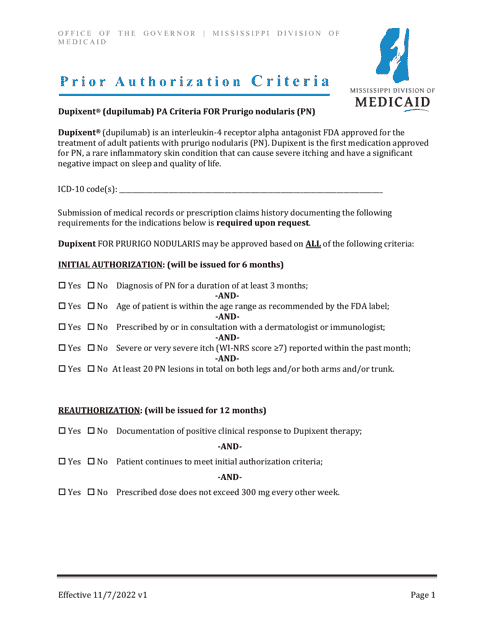
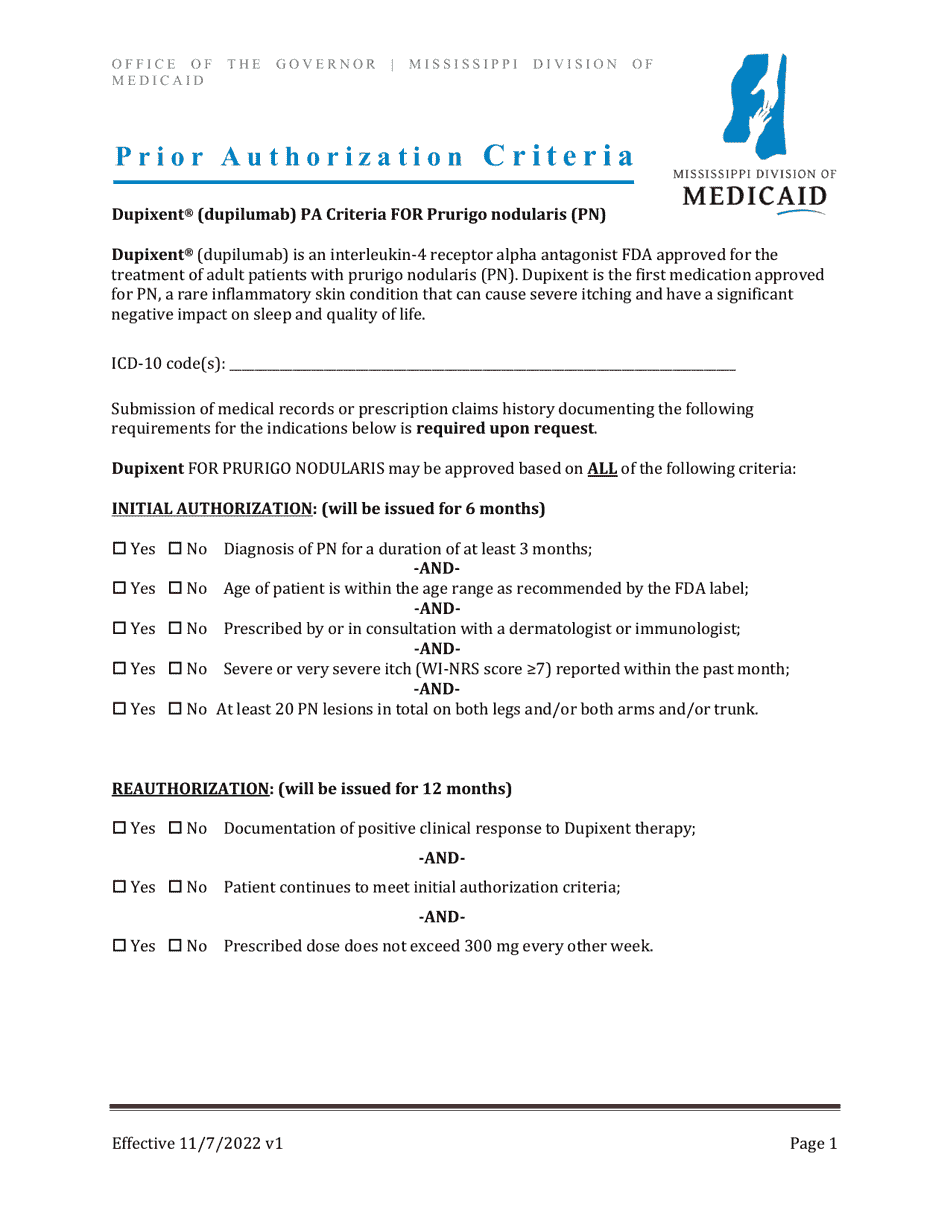
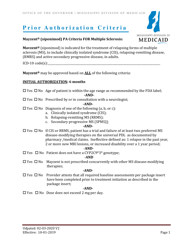
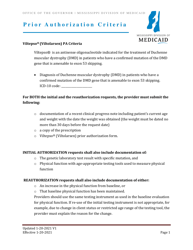
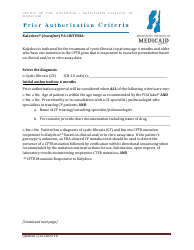
Prior Authorization Criteria - Dupixent - Prurigo Nodularis - Mississippi
Prior Authorization Criteria - Dupixent - Prurigo Nodularis is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is Dupixent?
A: Dupixent is a medication used to treat certain skin conditions.
Q: What is Prurigo Nodularis?
A: Prurigo Nodularis is a chronic skin condition characterized by itchy nodules or bumps.
Q: What is prior authorization?
A: Prior authorization refers to the process of getting approval from your insurance company before they will cover the cost of a medication.
Q: What are prior authorization criteria?
A: Prior authorization criteria are the specific requirements set by your insurance company that you must meet in order to receive coverage for a medication.
Q: How can I find the prior authorization criteria for Dupixent for Prurigo Nodularis in Mississippi?
A: You can find the specific prior authorization criteria for Dupixent for the treatment of Prurigo Nodularis in Mississippi by contacting your insurance company or reviewing your plan documents.
Q: What should I do if I don't meet the prior authorization criteria?
A: If you don't meet the prior authorization criteria, you may need to explore alternative treatment options or work with your healthcare provider to address the issue.
Q: Can my healthcare provider help with the prior authorization process?
A: Yes, your healthcare provider can assist you with the prior authorization process by providing necessary documentation and working with your insurance company to obtain approval.
Q: Is prior authorization required for all medications?
A: No, not all medications require prior authorization. It depends on your insurance plan and the specific medication being prescribed.
Q: How long does the prior authorization process take?
A: The length of the prior authorization process can vary, but it typically takes a few days to a few weeks.
Q: Can the prior authorization decision be appealed?
A: Yes, if your prior authorization request is denied, you have the right to appeal the decision and provide additional information to support your case.
Form Details:
- Released on November 7, 2022;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.