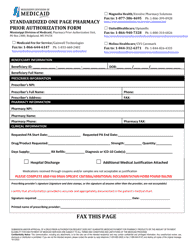
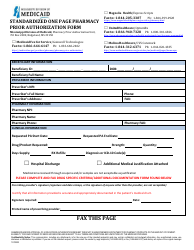
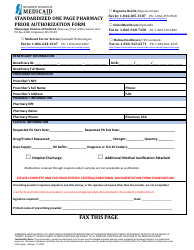
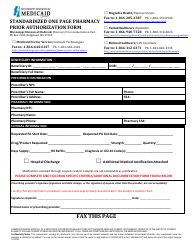
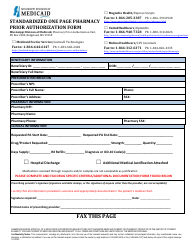
This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
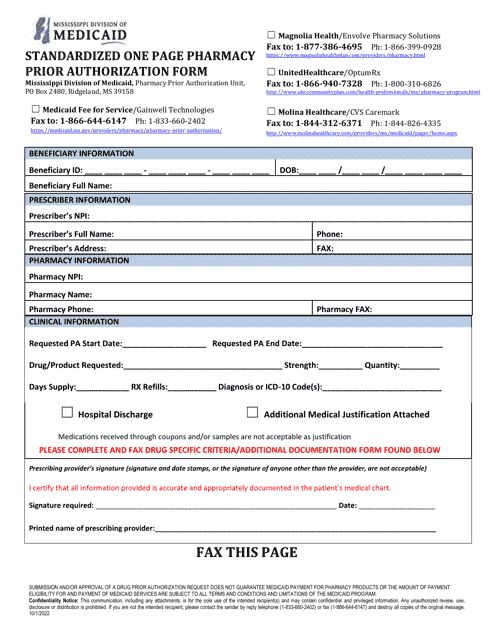
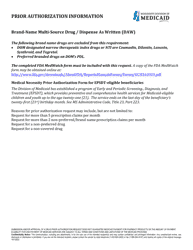
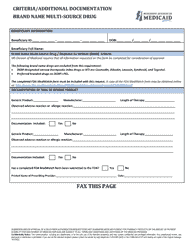
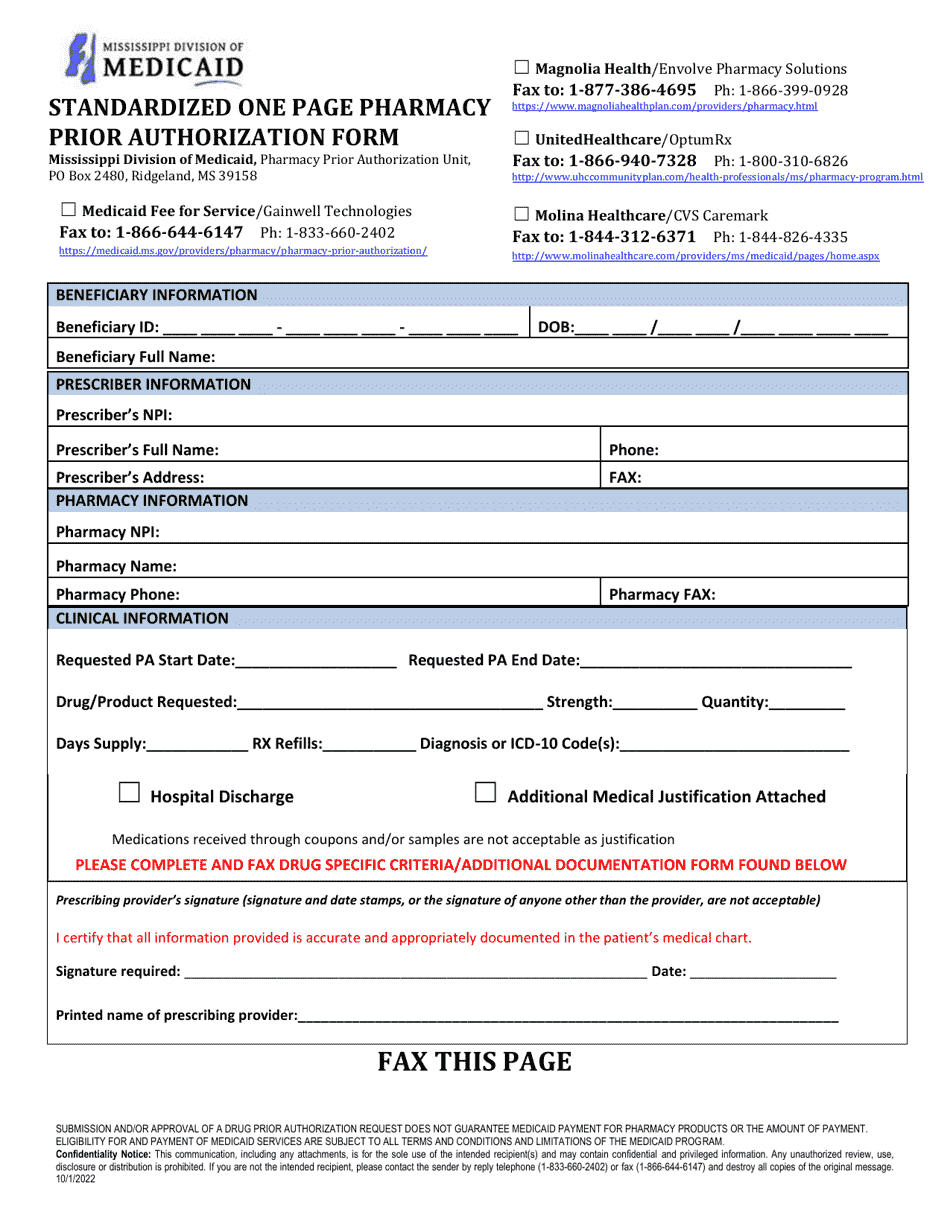
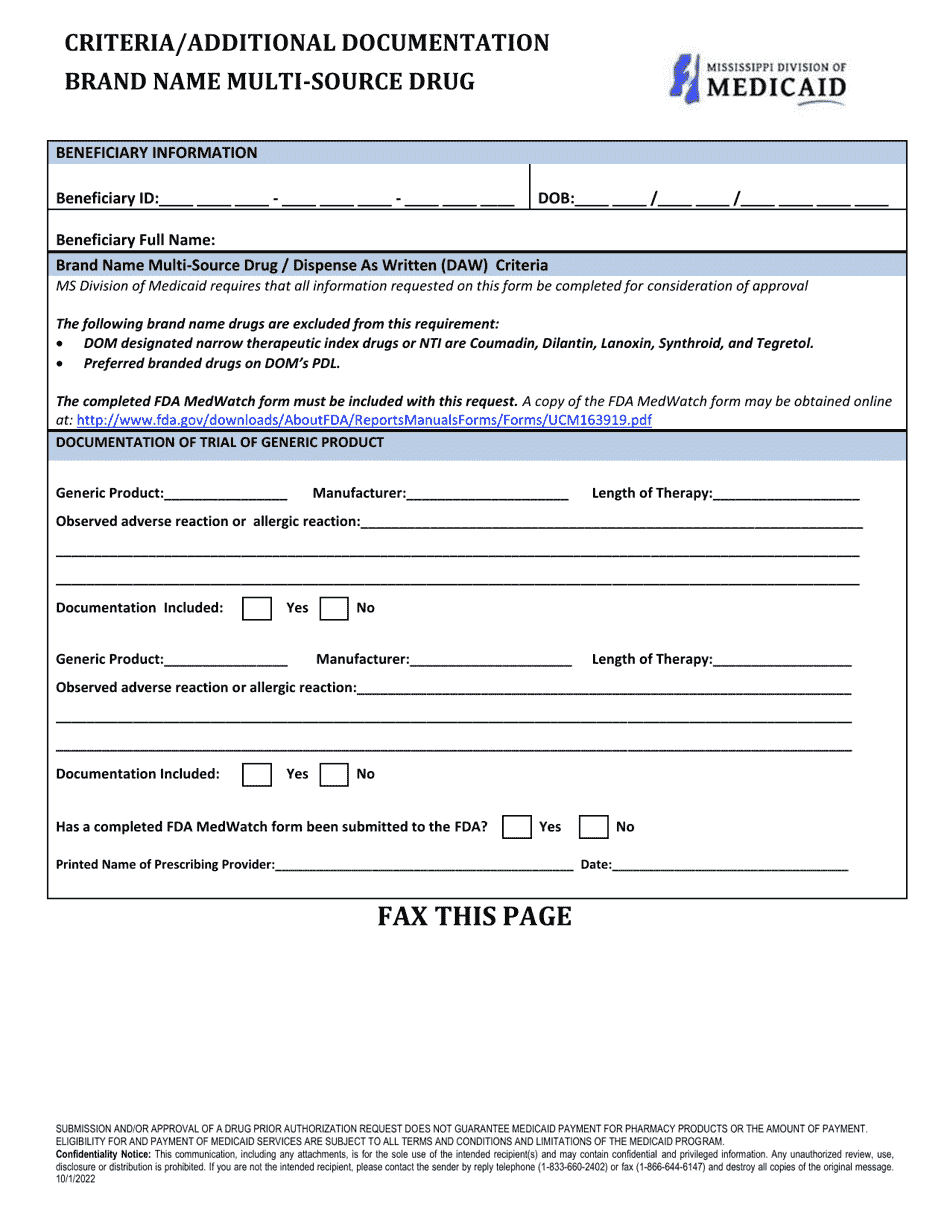
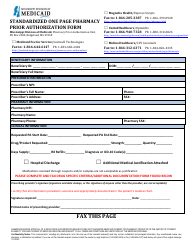
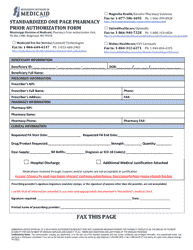
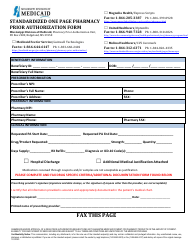
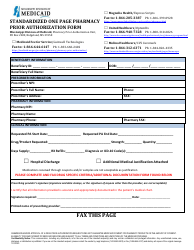
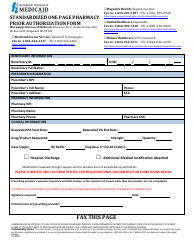
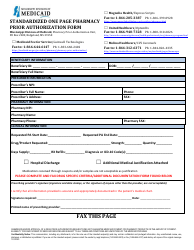
Prior Authorization Packet - Brand Name Multi-Source - Mississippi
Prior Authorization Packet - Brand Name Multi-Source is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is a prior authorization?
A: A prior authorization is a process where your doctor must get approval from your insurance company before prescribing certain medications.
Q: Why is a prior authorization required for brand name multi-source medications?
A: A prior authorization may be required for brand name multi-source medications to ensure that they are medically necessary and cost-effective.
Q: What is a brand name multi-source medication?
A: A brand name multi-source medication is a medication that is available in both brand name and generic versions.
Q: What should I do if my doctor prescribes a brand name multi-source medication that requires a prior authorization?
A: You should contact your insurance company to find out what specific information and forms are required for the prior authorization.
Q: How long does it take to get a prior authorization?
A: The time it takes to get a prior authorization can vary, but it is usually within a few days.
Q: What happens if my prior authorization request is denied?
A: If your prior authorization request is denied, you have the right to appeal the decision.
Q: Can my doctor help with the prior authorization process?
A: Yes, your doctor's office can assist you with the prior authorization process by providing the necessary documentation and communicating with your insurance company.
Form Details:
- Released on October 1, 2022;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.