This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
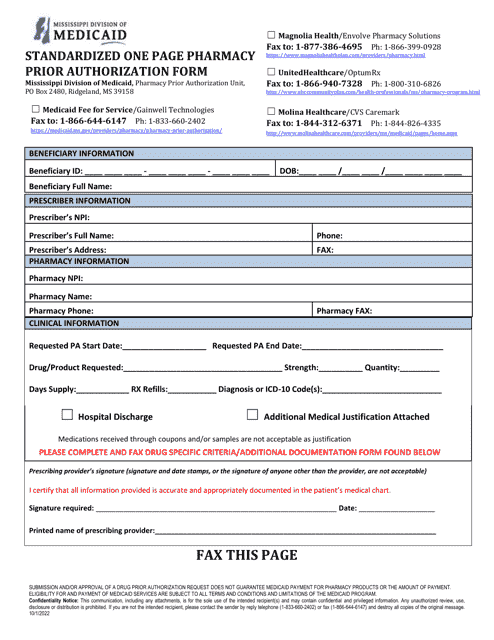
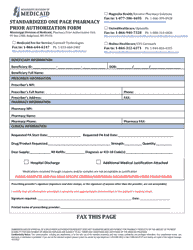
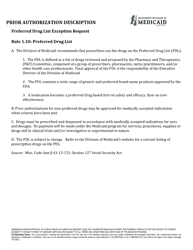
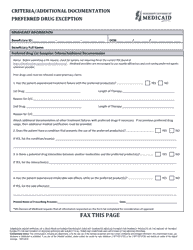
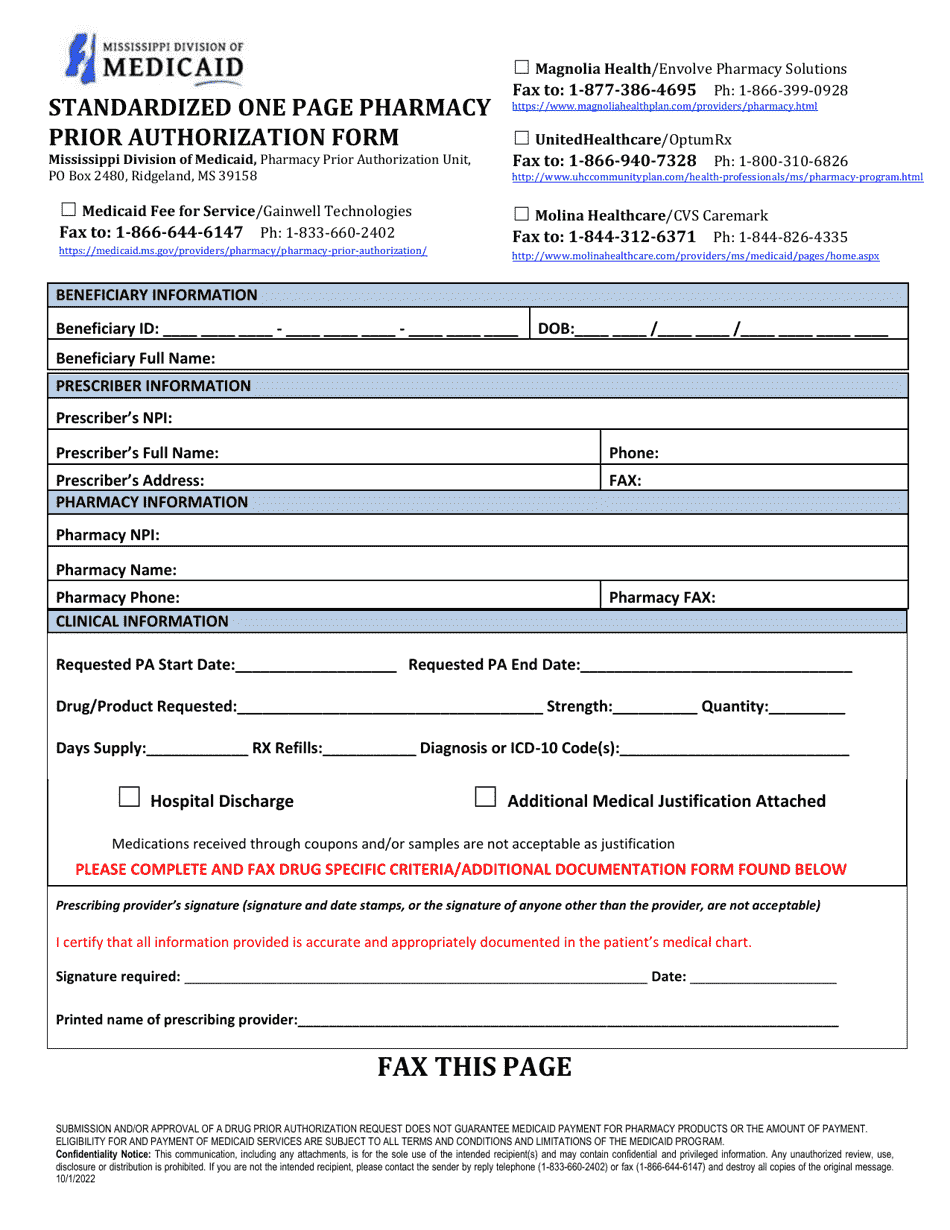
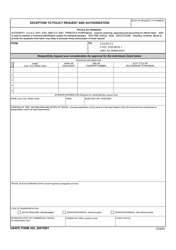
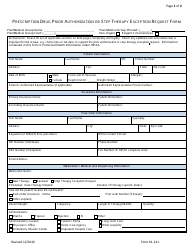
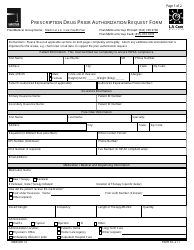
Prior Authorization Packet - Preferred Drug List Exception Request - Mississippi
Prior Authorization Packet - Preferred Drug List Exception Request is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is a prior authorization packet?
A: A prior authorization packet is a set of documents that need to be completed in order to request coverage for a medication that is not included in the preferred drug list.
Q: What is a preferred drug list exception request?
A: A preferred drug list exception request is a request to obtain coverage for a medication that is not on the preferred drug list.
Q: How do I request a preferred drug list exception in Mississippi?
A: To request a preferred drug list exception in Mississippi, you need to complete and submit a prior authorization packet.
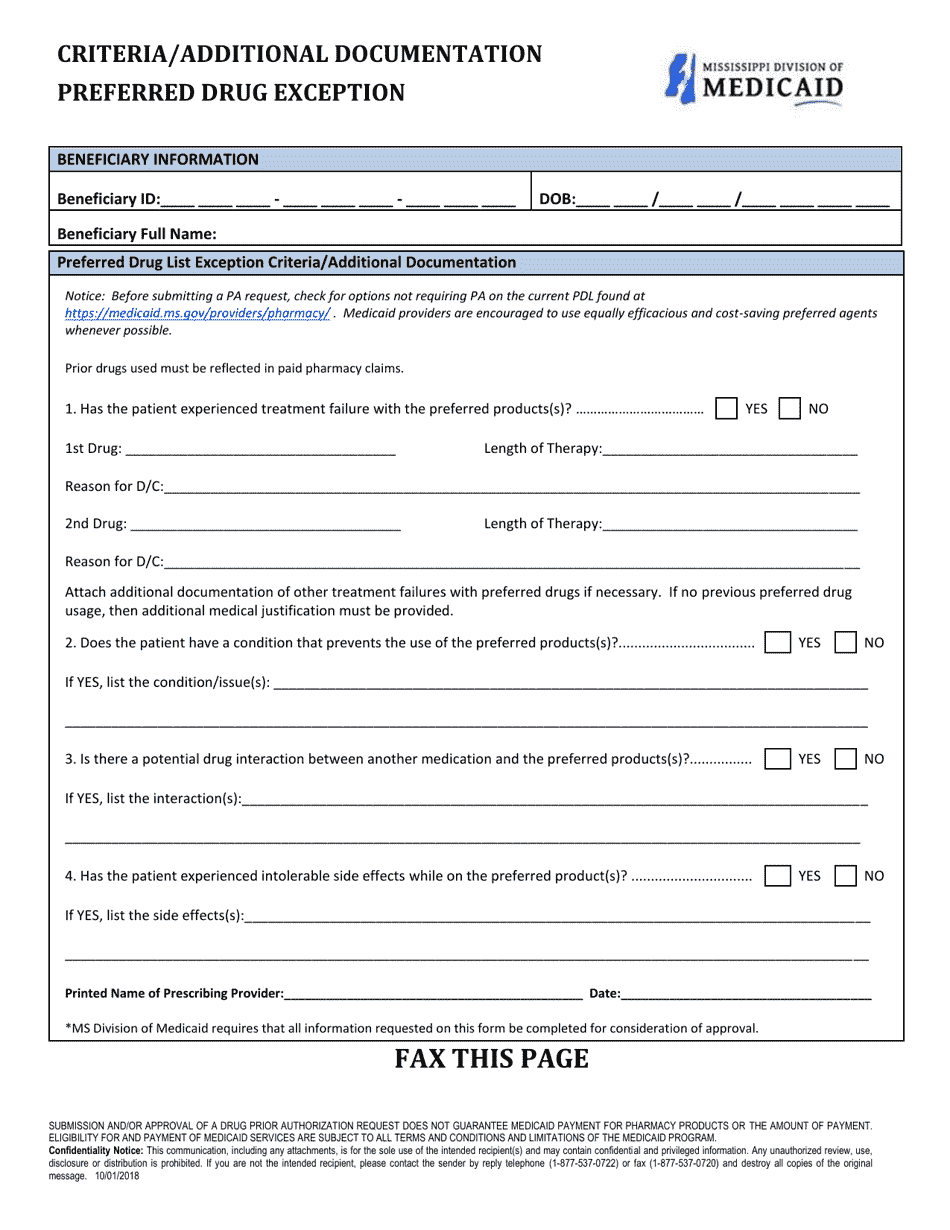
Q: What documents are required for a prior authorization packet?
A: The documents required for a prior authorization packet may vary, but generally include a completed request form, supporting documentation from a healthcare provider, and relevant medical records.
Q: How long does it take to process a preferred drug list exception request in Mississippi?
A: The processing time for a preferred drug list exception request in Mississippi can vary, but it typically takes around 5-10 business days.
Q: Will I be notified of the decision on my preferred drug list exception request?
A: Yes, you should receive a notification regarding the decision on your preferred drug list exception request.
Q: Can I appeal the decision if my preferred drug list exception request is denied?
A: Yes, if your preferred drug list exception request is denied, you have the right to appeal the decision.
Q: What are the possible outcomes of a preferred drug list exception request?
A: The possible outcomes of a preferred drug list exception request include approval, denial, or approval with conditions.
Q: Do I have to pay for the medication if my preferred drug list exception request is approved?
A: The cost of the medication will depend on your health insurance plan's coverage and your cost-sharing responsibilities.
Form Details:
- Released on October 1, 2022;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.