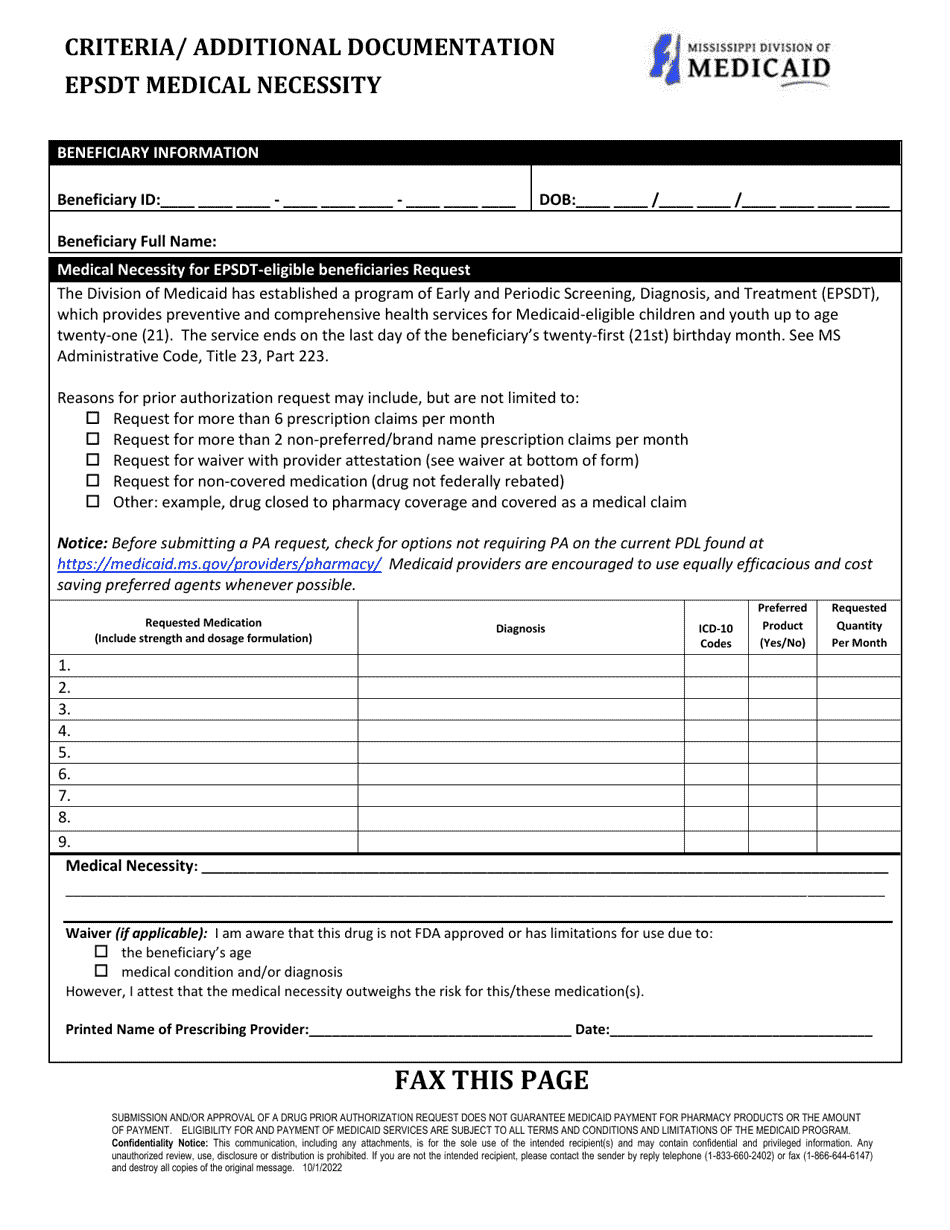
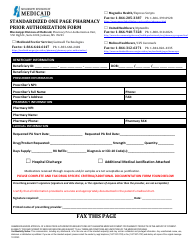
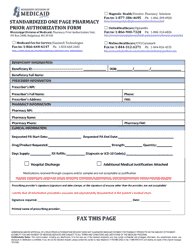
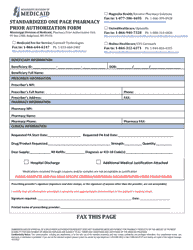
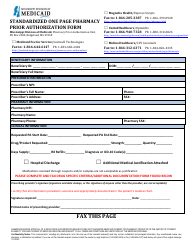
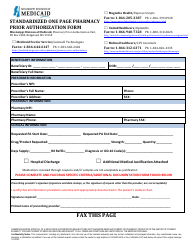
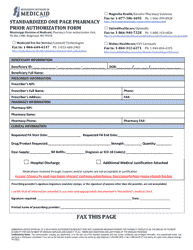
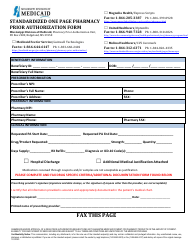
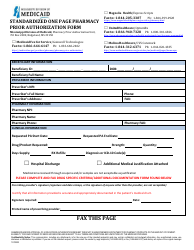
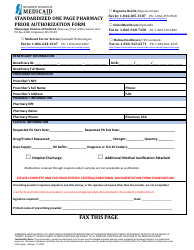
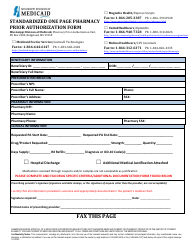
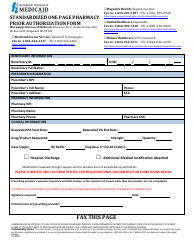
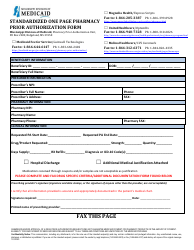
Prior Authorization Packet - Epsdt - Beneficiaries Under 21 - Mississippi
Prior Authorization Packet - Epsdt - Beneficiaries Under 21 is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
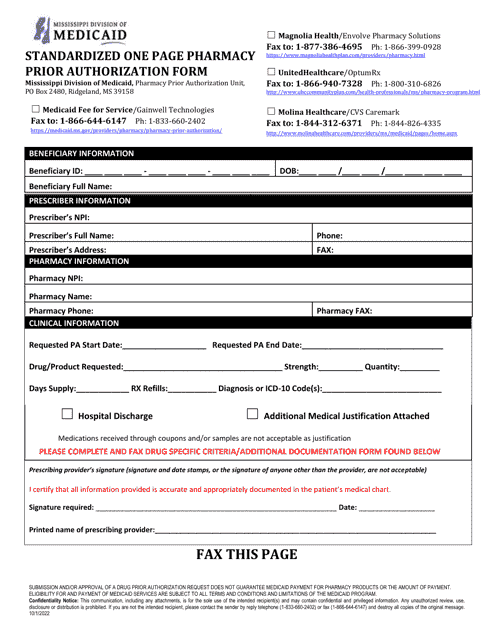
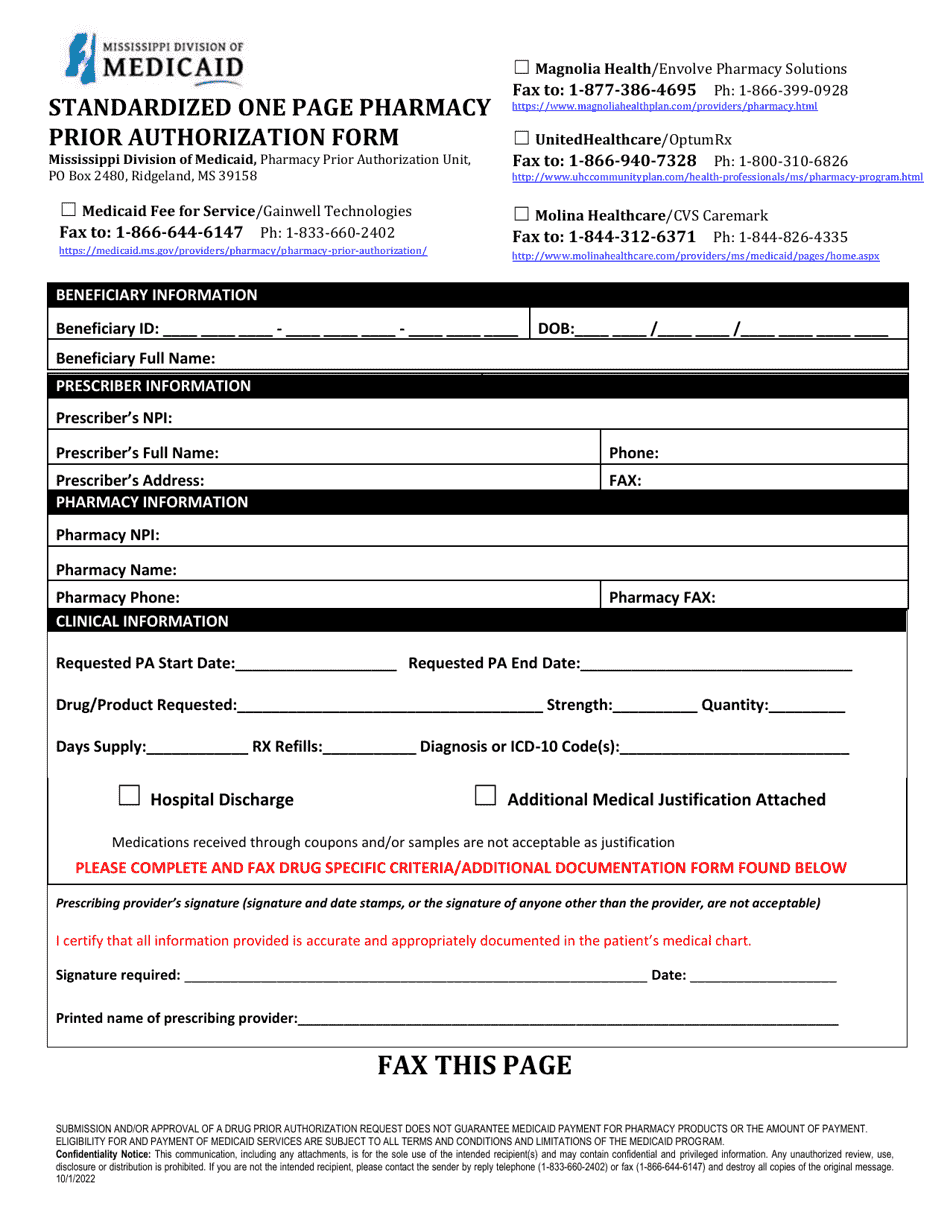
Q: What is a prior authorization packet?
A: A prior authorization packet is a collection of documents and forms that need to be submitted to an insurance company or Medicaid program to request approval for certain medical services or treatments.
Q: What is EPSDT?
A: EPSDT stands for Early and Periodic Screening, Diagnostic, and Treatment. It is a Medicaid program that provides comprehensive and preventive healthcare services to children and youth under the age of 21.
Q: Who are beneficiaries under 21?
A: Beneficiaries under 21 refers to individuals who are eligible for Medicaid and are under the age of 21.
Q: What is the purpose of the prior authorization packet for beneficiaries under 21 in Mississippi?
A: The prior authorization packet is necessary to obtain approval for certain medical services or treatments for beneficiaries under 21 in Mississippi.
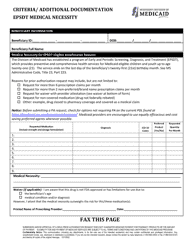
Q: What documents are typically included in a prior authorization packet for beneficiaries under 21 in Mississippi?
A: The specific documents required may vary, but typically a prior authorization packet for beneficiaries under 21 in Mississippi may include medical records, treatment plans, prescriptions, and a completed authorization form.
Q: How long does it take to get approval after submitting a prior authorization packet for beneficiaries under 21 in Mississippi?
A: The approval timeline can vary, but generally it takes a few days to a few weeks to receive a decision after submitting a prior authorization packet.
Q: What should I do if my prior authorization packet for beneficiaries under 21 in Mississippi is denied?
A: If your prior authorization packet is denied, you may have the option to appeal the decision. Contact the Mississippi Division of Medicaid or your healthcare provider for assistance and guidance on the appeals process.
Q: Are all medical services and treatments covered by Medicaid for beneficiaries under 21 in Mississippi?
A: Not all medical services and treatments are automatically covered by Medicaid for beneficiaries under 21 in Mississippi. Prior authorization is often required to ensure that the requested services are medically necessary and appropriate.
Form Details:
- Released on October 1, 2022;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.