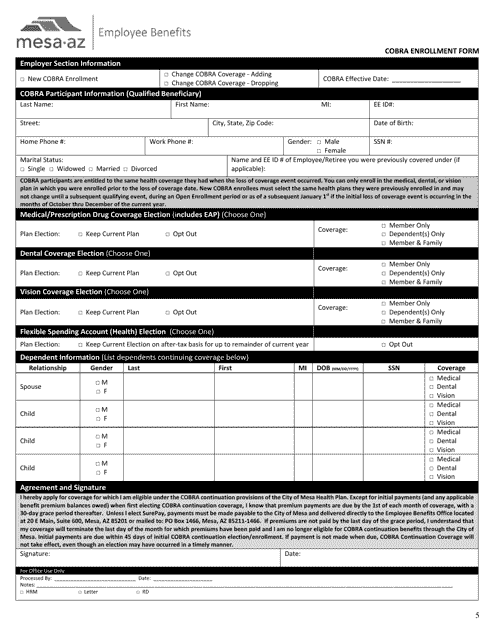
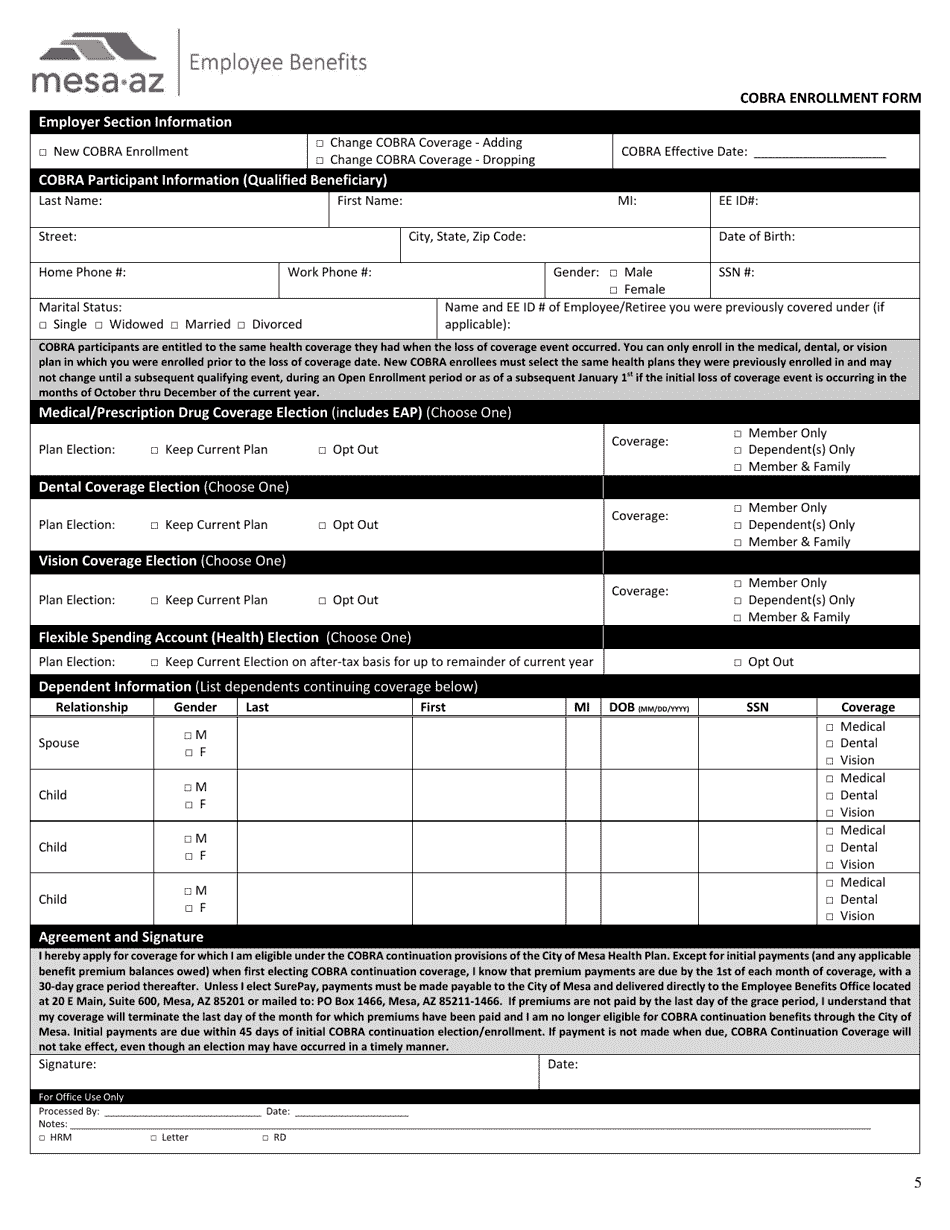
Cobra Enrollment Form - City of Mesa, Arizona
Cobra Enrollment Form is a legal document that was released by the Employee Benefits Department - City of Mesa, Arizona - a government authority operating within Arizona. The form may be used strictly within City of Mesa.
FAQ
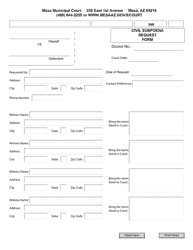
Q: What is the Cobra Enrollment Form?
A: The Cobra Enrollment Form is a form that allows individuals to enroll in Cobra coverage.
Q: Who is eligible to use the Cobra Enrollment Form?
A: Employees and their dependents who lose their group health coverage may be eligible for Cobra and can use the Cobra Enrollment Form.
Q: How does the Cobra Enrollment Form work?
A: By completing the Cobra Enrollment Form, you are indicating your interest in continuing your health coverage under Cobra.
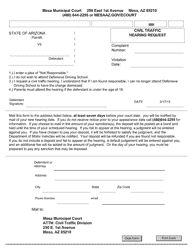
Q: Is there a deadline to submit the Cobra Enrollment Form?
A: Yes, you usually have 60 days from the date of your coverage termination to submit the Cobra Enrollment Form.
Q: What happens after I submit the Cobra Enrollment Form?
A: After submitting the Cobra Enrollment Form, you will receive information about your Cobra coverage and how to make premium payments.
Q: How long does Cobra coverage last?
A: Cobra coverage typically lasts for 18 months, although it may be extended under certain circumstances.
Q: Is Cobra coverage the same as my previous group health coverage?
A: No, Cobra coverage is similar to your previous coverage, but it may have different costs and benefits.
Q: How much does Cobra coverage cost?
A: The cost of Cobra coverage can vary, but it is generally the full premium amount plus a 2% administrative fee.
Q: Can I cancel my Cobra coverage?
A: Yes, you can cancel your Cobra coverage at any time, but you may not be able to re-enroll in a group health plan until the next open enrollment period.
Form Details:
- The latest edition currently provided by the Employee Benefits Department - City of Mesa, Arizona;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
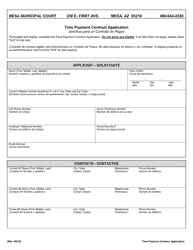
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Employee Benefits Department - City of Mesa, Arizona.