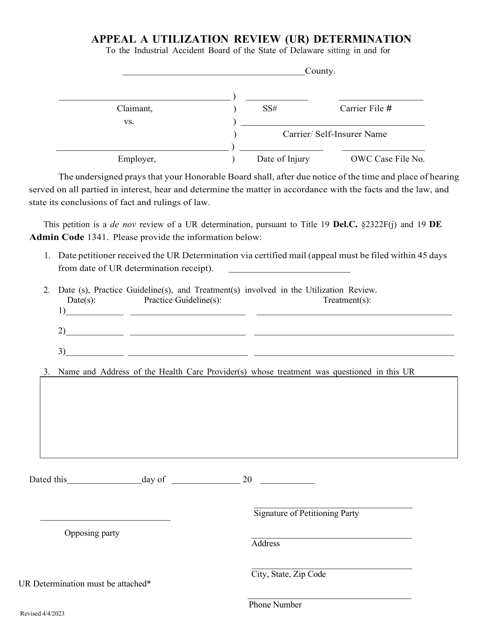
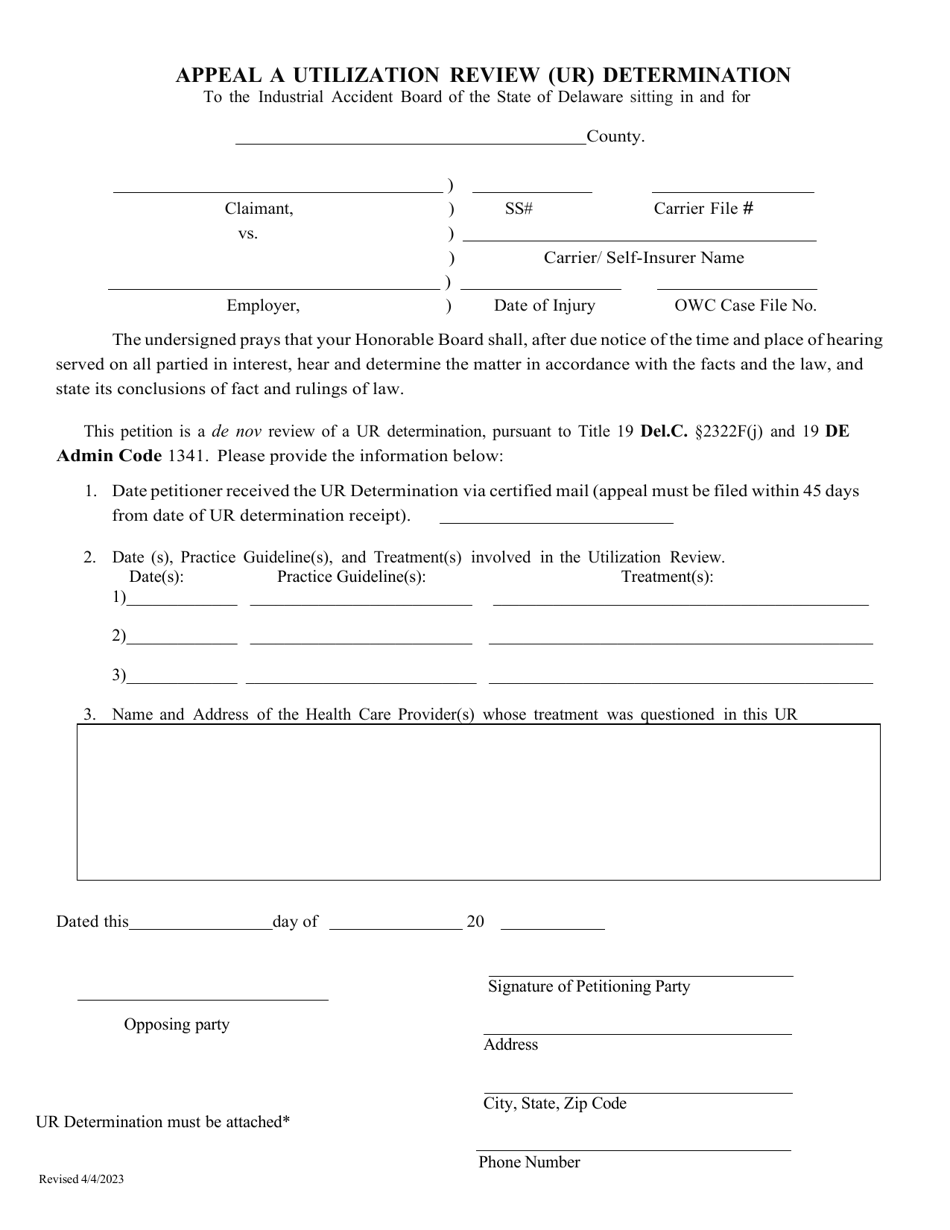
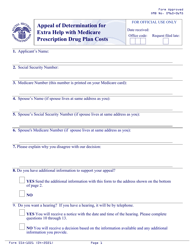
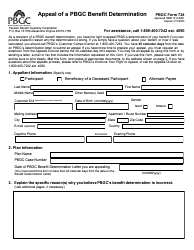
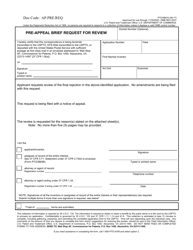
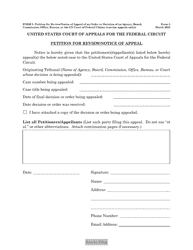
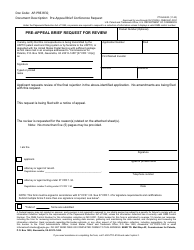
Appeal a Utilization Review (Ur) Determination - Delaware
Appeal a Utilization Review (Ur) Determination is a legal document that was released by the Delaware Department of Labor - a government authority operating within Delaware.
FAQ
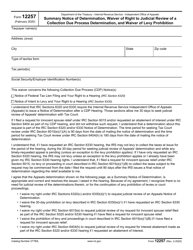
Q: What is a Utilization Review (UR) determination?
A: A Utilization Review (UR) determination is a decision made by a healthcare insurer or managed care organization regarding the medical necessity or appropriateness of a requested treatment or service.
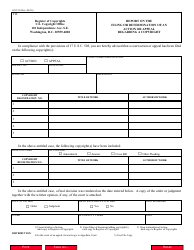
Q: Why would I need to appeal a Utilization Review (UR) determination?
A: You may need to appeal a UR determination if you believe that the decision made by your healthcare insurer or managed care organization is incorrect or unfair.
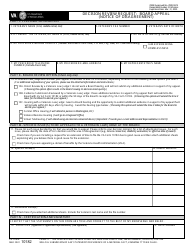
Q: How can I appeal a Utilization Review (UR) determination in Delaware?
A: To appeal a UR determination in Delaware, you can contact your healthcare insurer or managed care organization for instructions on the appeals process.
Q: What should I include in my appeal of a Utilization Review (UR) determination?
A: In your appeal, you should include any relevant medical records, documentation from healthcare professionals, and a written explanation of why you believe the UR determination is incorrect or unfair.
Q: What happens after I submit an appeal of a Utilization Review (UR) determination?
A: After you submit an appeal, your healthcare insurer or managed care organization will review your appeal and make a decision. They are required to notify you in writing of their decision within a certain timeframe.
Q: What if my appeal of a Utilization Review (UR) determination is denied?
A: If your appeal is denied, you may have the option to further appeal the decision through an external appeals process. You should contact your healthcare insurer or managed care organization for more information on external appeals.
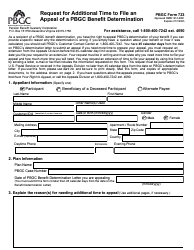
Form Details:
- Released on April 4, 2023;
- The latest edition currently provided by the Delaware Department of Labor;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Delaware Department of Labor.