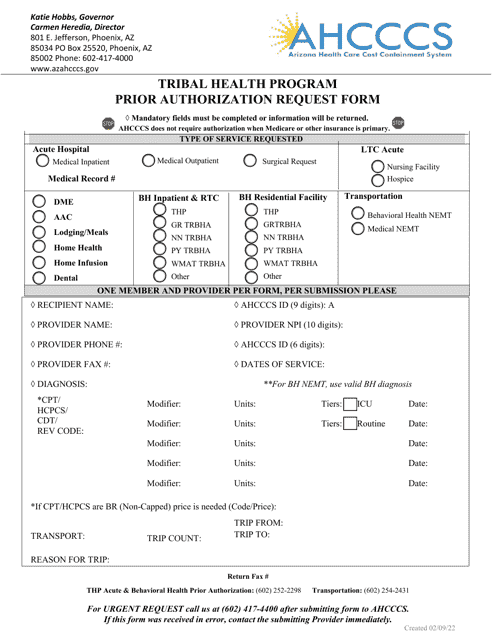
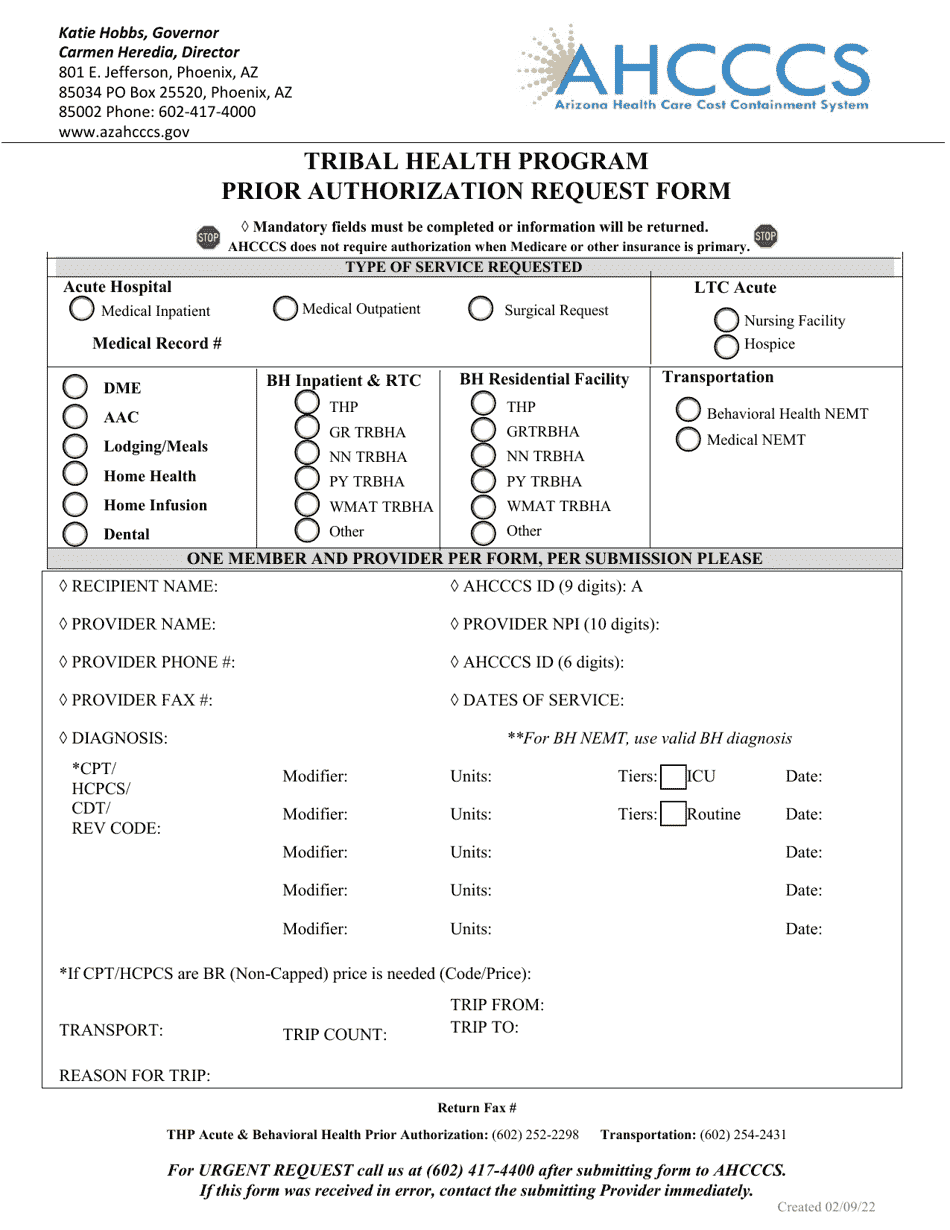
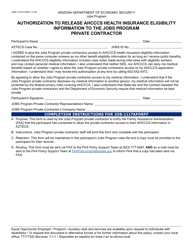
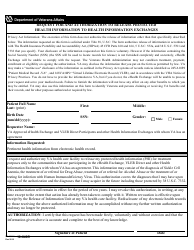
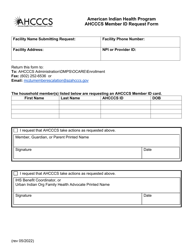
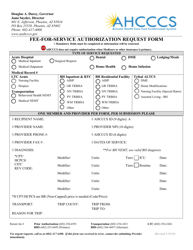
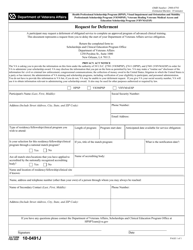
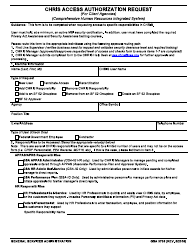
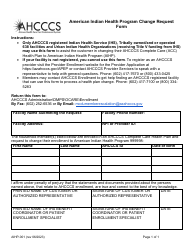
Prior Authorization Request Form - Tribal Health Program - Arizona
Prior Authorization Request Form - Tribal Health Program is a legal document that was released by the Arizona Health Care Cost Containment System - a government authority operating within Arizona.
FAQ
Q: What is the Prior Authorization Request Form for?
A: The form is for the Tribal Health Program in Arizona.
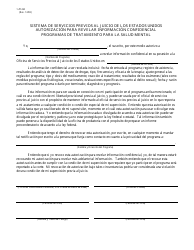
Q: What is a prior authorization?
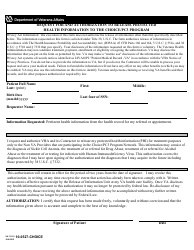
A: Prior authorization is the process of obtaining approval from the health insurance plan before receiving certain medical services or medications.
Q: Why is a prior authorization required?
A: Insurance plans may require prior authorization to ensure medical services or medications meet their coverage criteria.
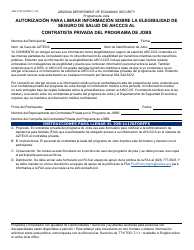
Q: Who needs to complete the Prior Authorization Request Form?
A: Healthcare providers or members of the Tribal Health Program in Arizona may need to complete the form.
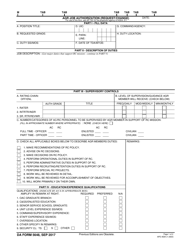
Q: What information is needed to complete the form?
A: The form will require details about the requested services or medications, as well as patient information and healthcare provider information.
Q: How long does it take to process a prior authorization?
A: The processing time can vary, but it typically takes a few business days for a prior authorization to be reviewed and approved.
Q: What happens after a prior authorization is approved?
A: After approval, the requested medical services or medications can be obtained and may be covered by the insurance plan.
Q: What should I do if my prior authorization request is denied?
A: If your request is denied, you may have the option to appeal the decision or explore alternative treatment options with your healthcare provider.
Q: Are there any fees associated with prior authorization?
A: The fees associated with prior authorization may vary depending on the insurance plan and the specific services or medications being requested.
Form Details:
- Released on February 9, 2022;
- The latest edition currently provided by the Arizona Health Care Cost Containment System;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Arizona Health Care Cost Containment System.