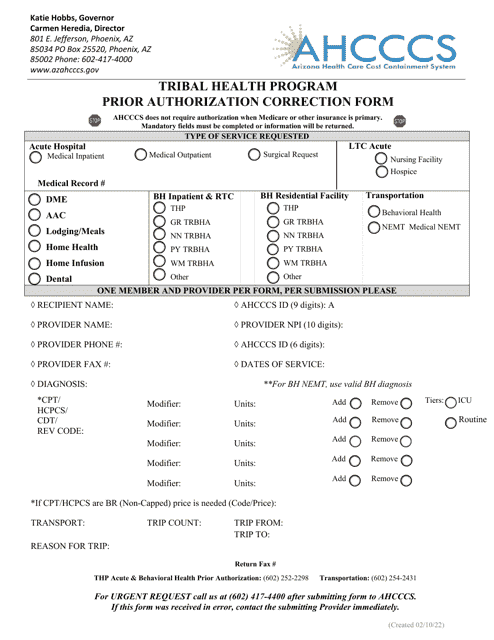
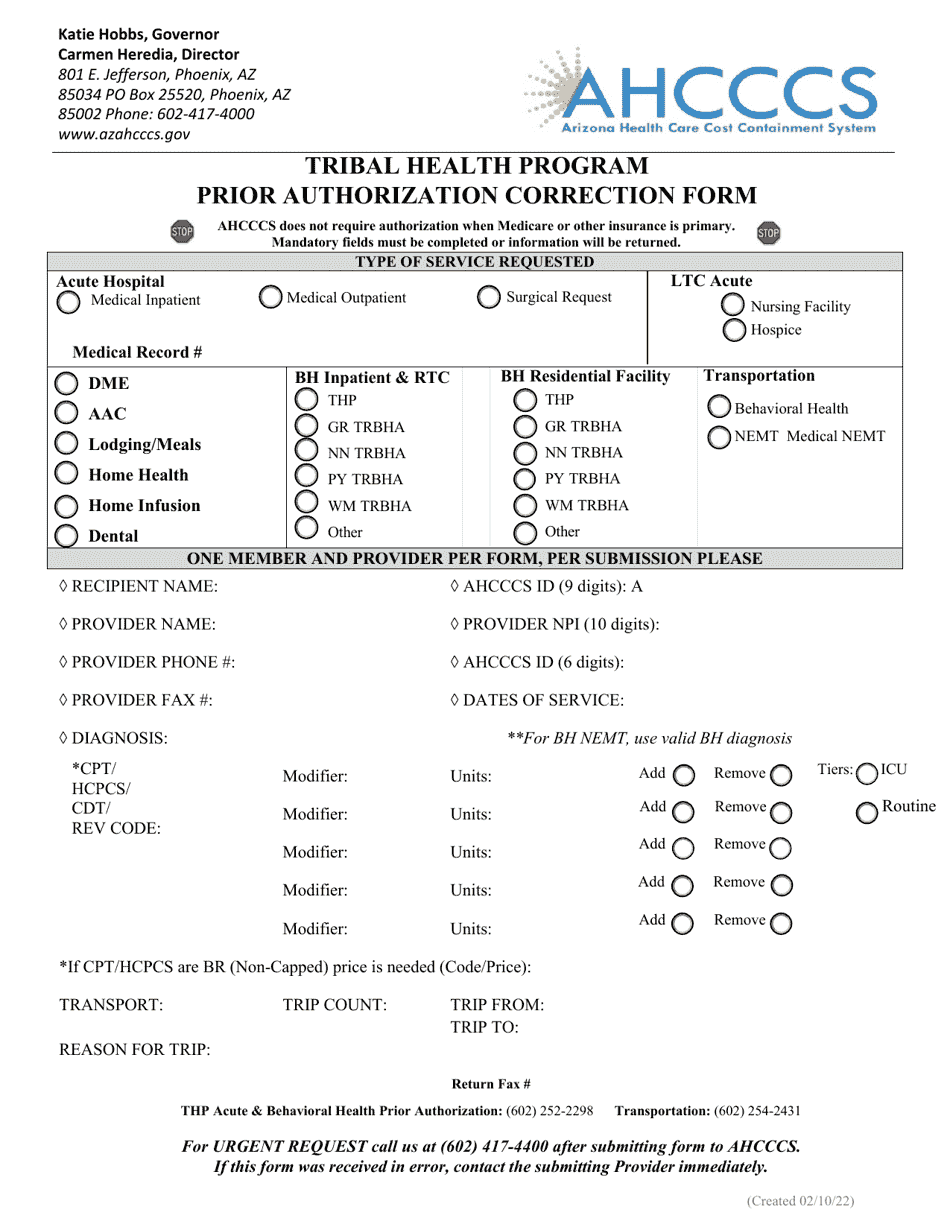
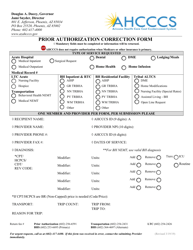
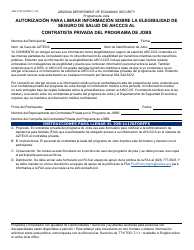
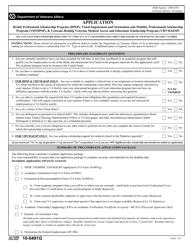
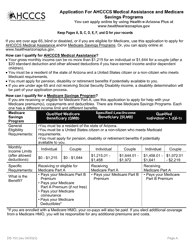
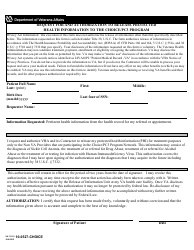
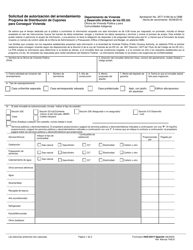
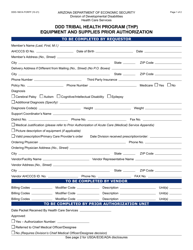
Prior Authorization Correction Form - Tribal Health Program - Arizona
Prior Authorization Correction Form - Tribal Health Program is a legal document that was released by the Arizona Health Care Cost Containment System - a government authority operating within Arizona.
FAQ
Q: What is the Prior Authorization Correction Form?
A: The Prior Authorization Correction Form is a form used for the Tribal Health Program in Arizona.
Q: Who can use the Prior Authorization Correction Form?
A: The Prior Authorization Correction Form is specifically for the Tribal Health Program in Arizona.
Q: What is a prior authorization?
A: A prior authorization is a requirement from an insurance company or healthcare provider that must be obtained before certain medical services or medications will be covered.
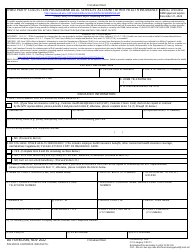
Q: Why would I need to use the Prior Authorization Correction Form?
A: You would need to use the Prior Authorization Correction Form if there was an error or discrepancy in a prior authorization request for the Tribal Health Program in Arizona.
Form Details:
- Released on February 10, 2022;
- The latest edition currently provided by the Arizona Health Care Cost Containment System;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Arizona Health Care Cost Containment System.