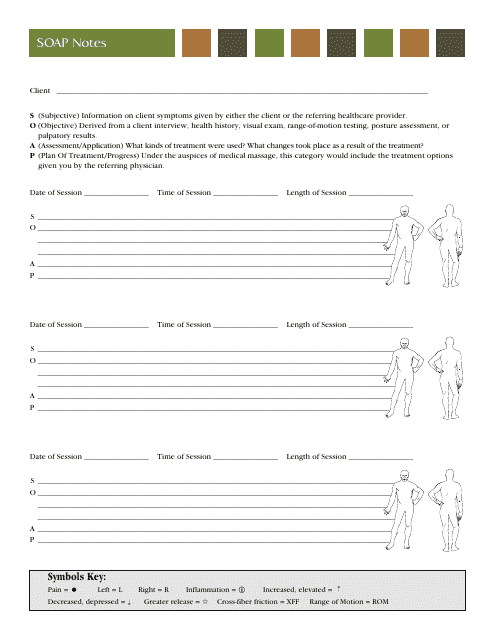
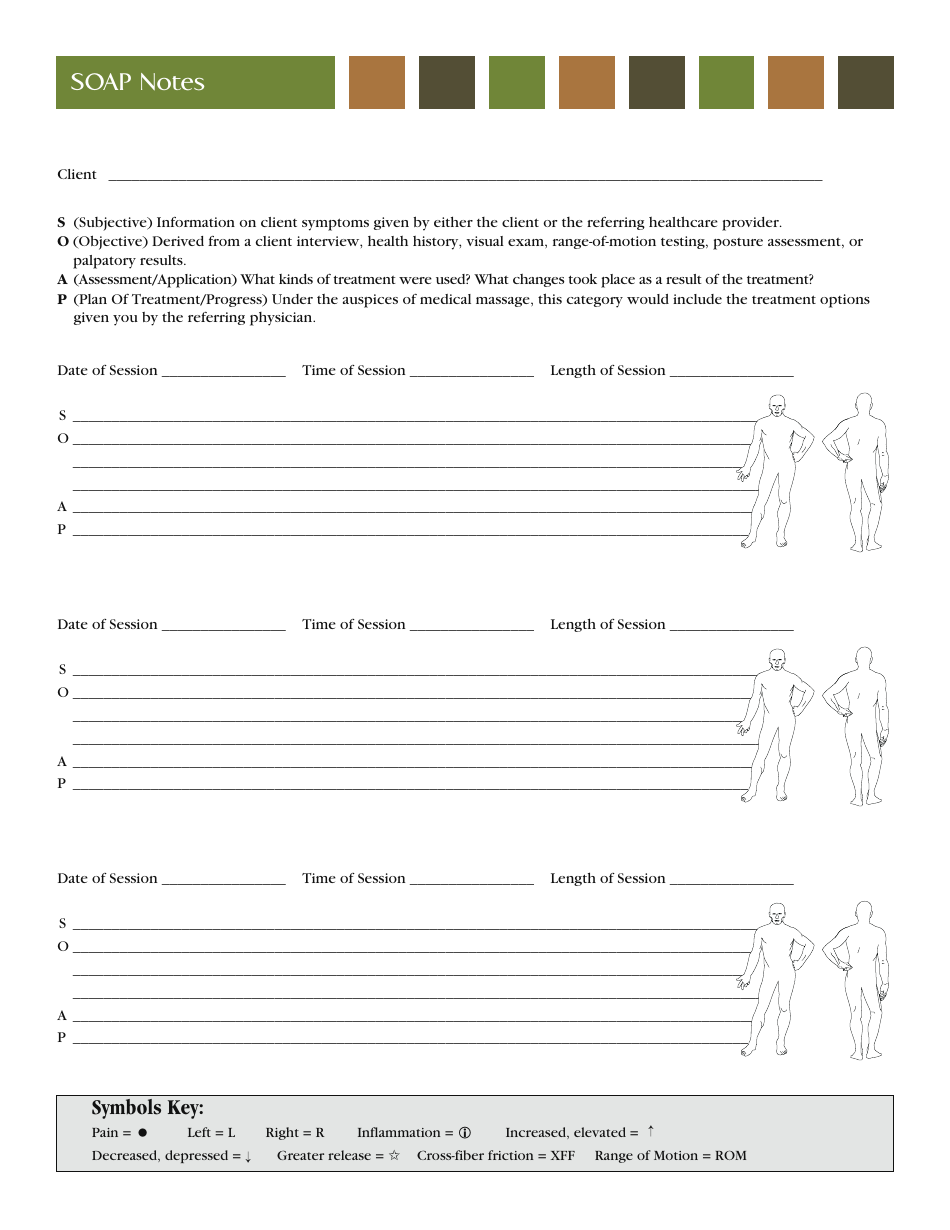
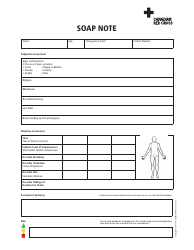
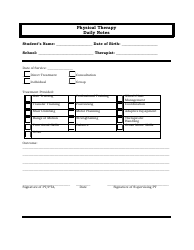
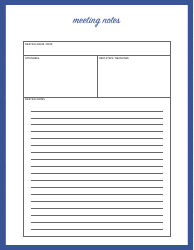
Soap Notes Template
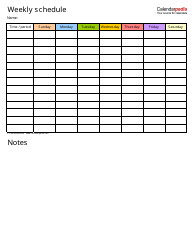
Soap Notes Template is commonly used by healthcare professionals, including doctors and nurses, to document patient encounters in a structured manner. It stands for Subjective, Objective, Assessment, and Plan, and it helps healthcare providers organize and document pertinent information about a patient's health condition, including their symptoms, physical examination findings, diagnosis, and treatment plan.
Soap notes are typically filed by healthcare professionals, such as doctors, nurses, or other medical providers, after they have provided care or treatment to a patient.
FAQ
Q: What is a soap note?
A: A soap note is a medical documentation format used by healthcare professionals to document patient encounters.
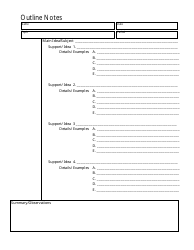
Q: What does SOAP stand for in soap notes?
A: SOAP stands for Subjective, Objective, Assessment, and Plan. It represents the different sections of a soap note.
Q: What is included in the subjective section of a soap note?
A: The subjective section of a soap note includes information provided by the patient, such as their symptoms and medical history.
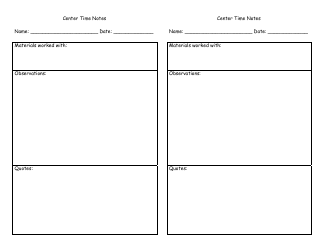
Q: What is included in the objective section of a soap note?
A: The objective section of a soap note includes measurable and observable data, such as vital signs and physical examination findings.
Q: What is included in the assessment section of a soap note?
A: The assessment section of a soap note includes the healthcare professional's evaluation and diagnosis of the patient's condition.
Q: What is included in the plan section of a soap note?
A: The plan section of a soap note includes the proposed treatment plan and recommendations for the patient.
Q: Why are soap notes important?
A: Soap notes are important for effective communication between healthcare providers, continuity of patient care, and documentation for legal and insurance purposes.