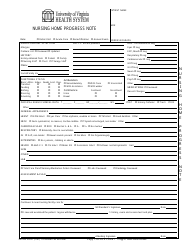
Soap Note Template - Amc
The SOAP note template (Amc) is used by medical professionals to document patient encounters and track their progress over time. It helps organize the subjective, objective, assessment, and plan information of a patient's visit.
The Soap Note Template is usually filed by healthcare professionals, such as doctors or nurses, at the relevant healthcare facility or clinic.
FAQ
Q: What is a SOAP note template?
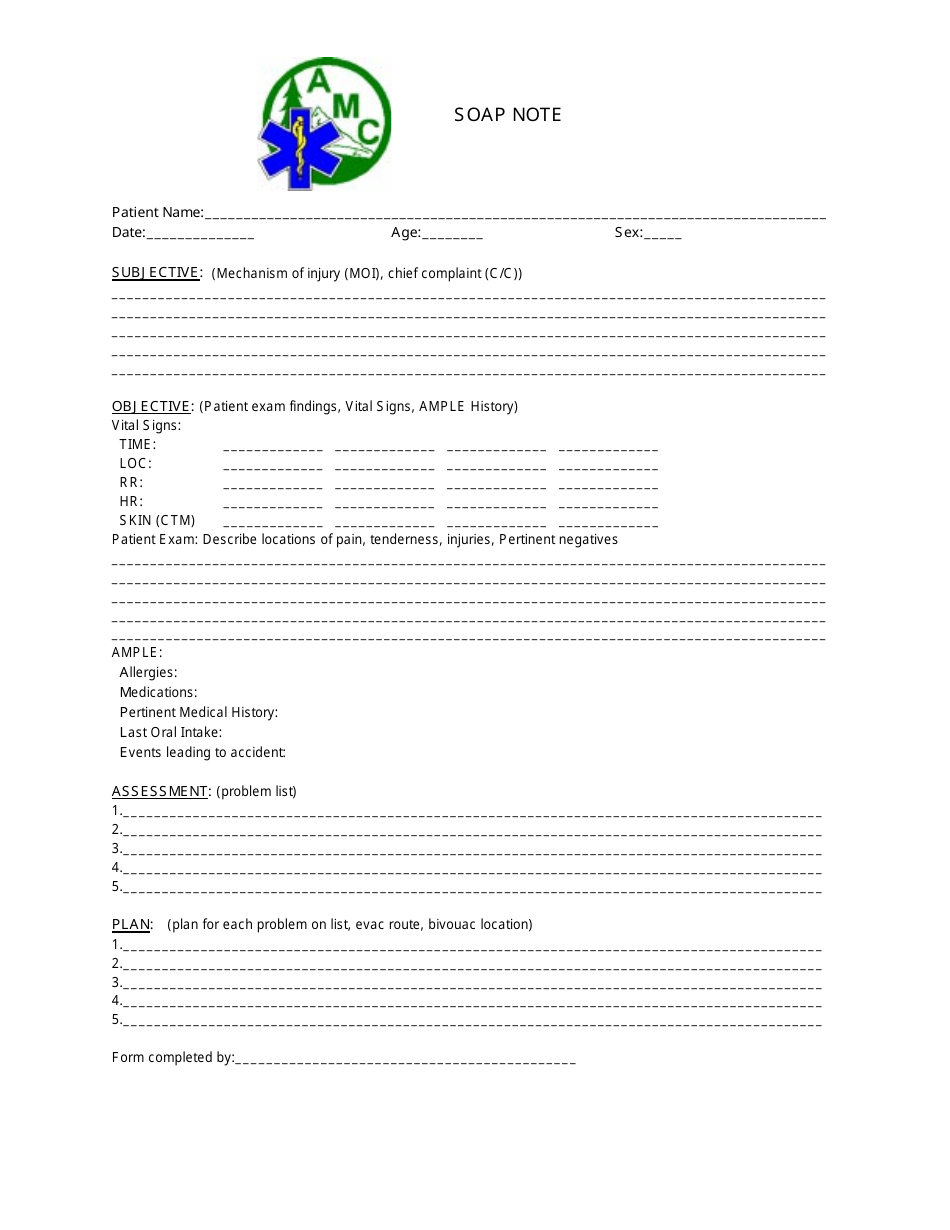
A: A SOAP note template is a standardized format used by healthcare professionals to document patient encounters, including subjective information (S), objective findings (O), assessment (A), and plan (P).
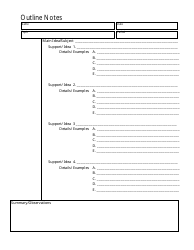
Q: How is a SOAP note template structured?
A: A SOAP note template typically consists of four sections: Subjective, Objective, Assessment, and Plan. Each section provides specific information about the patient's condition, examination findings, diagnosis, and treatment plan.
Q: What is included in the Subjective section of a SOAP note?
A: The Subjective section of a SOAP note includes information provided by the patient about their symptoms, medical history, and any relevant personal or social factors. It focuses on the patient's perspective and feelings.
Q: What is included in the Objective section of a SOAP note?
A: The Objective section of a SOAP note includes measurable and observable data obtained through physical examination, diagnostic tests, or imaging. It provides an objective evaluation of the patient's condition.
Q: What is included in the Assessment section of a SOAP note?
A: The Assessment section of a SOAP note includes the healthcare professional's evaluation and diagnosis based on the subjective and objective information. It summarizes the patient's current condition.
Q: What is included in the Plan section of a SOAP note?
A: The Plan section of a SOAP note outlines the treatment plan, including medications, procedures, referrals, and follow-up instructions. It also includes patient education and counseling.
Q: Why is a SOAP note template important?
A: A SOAP note template provides a standardized and organized way for healthcare professionals to document patient encounters. It ensures accurate and consistent recording of information, facilitating communication and continuity of care.
Q: Who uses SOAP note templates?
A: SOAP note templates are primarily used by healthcare professionals, including doctors, nurses, physical therapists, and other providers involved in patient care. They are commonly used in various healthcare settings, such as hospitals, clinics, and private practices.