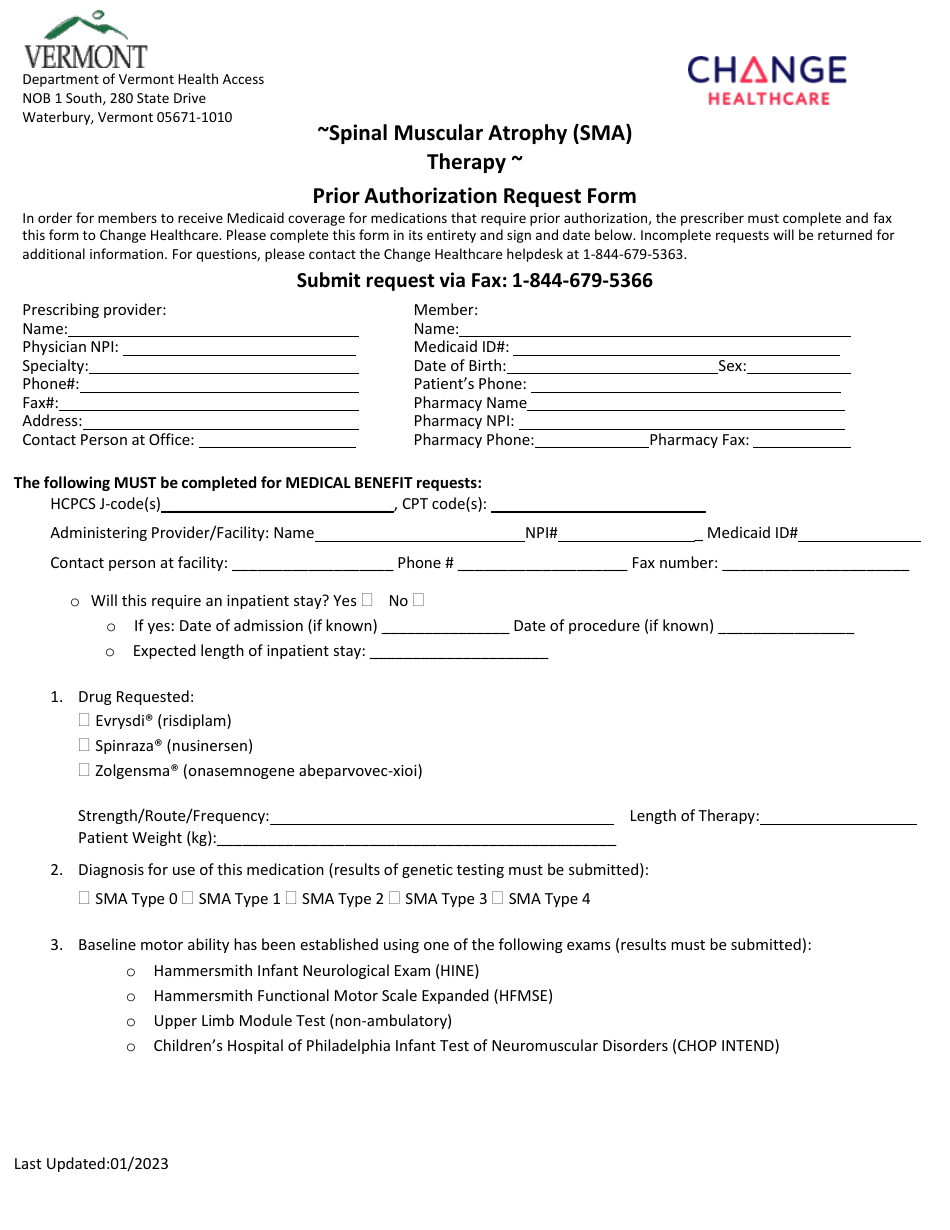
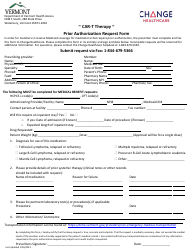
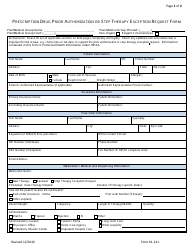
Spinal Muscular Atrophy (Sma) Therapy Prior Authorization Request Form - Vermont
Spinal Muscular Atrophy (Sma) Therapy Prior Authorization Request Form is a legal document that was released by the Department of Vermont Health Access - a government authority operating within Vermont.
FAQ
Q: What is the Spinal Muscular Atrophy (SMA) Therapy?
A: SMA Therapy is a treatment for Spinal Muscular Atrophy, a genetic disorder affecting the muscles.
Q: What is a Prior Authorization Request Form?
A: A Prior Authorization Request Form is a document that needs to be filled out to request coverage for a specific treatment or medication.
Q: What is the purpose of the Prior Authorization Request Form for SMA Therapy?
A: The purpose of the Prior Authorization Request Form for SMA Therapy is to request approval for coverage of the treatment.
Q: Who needs to fill out the Prior Authorization Request Form?
A: The Prior Authorization Request Form needs to be filled out by the healthcare provider or the patient's representative.
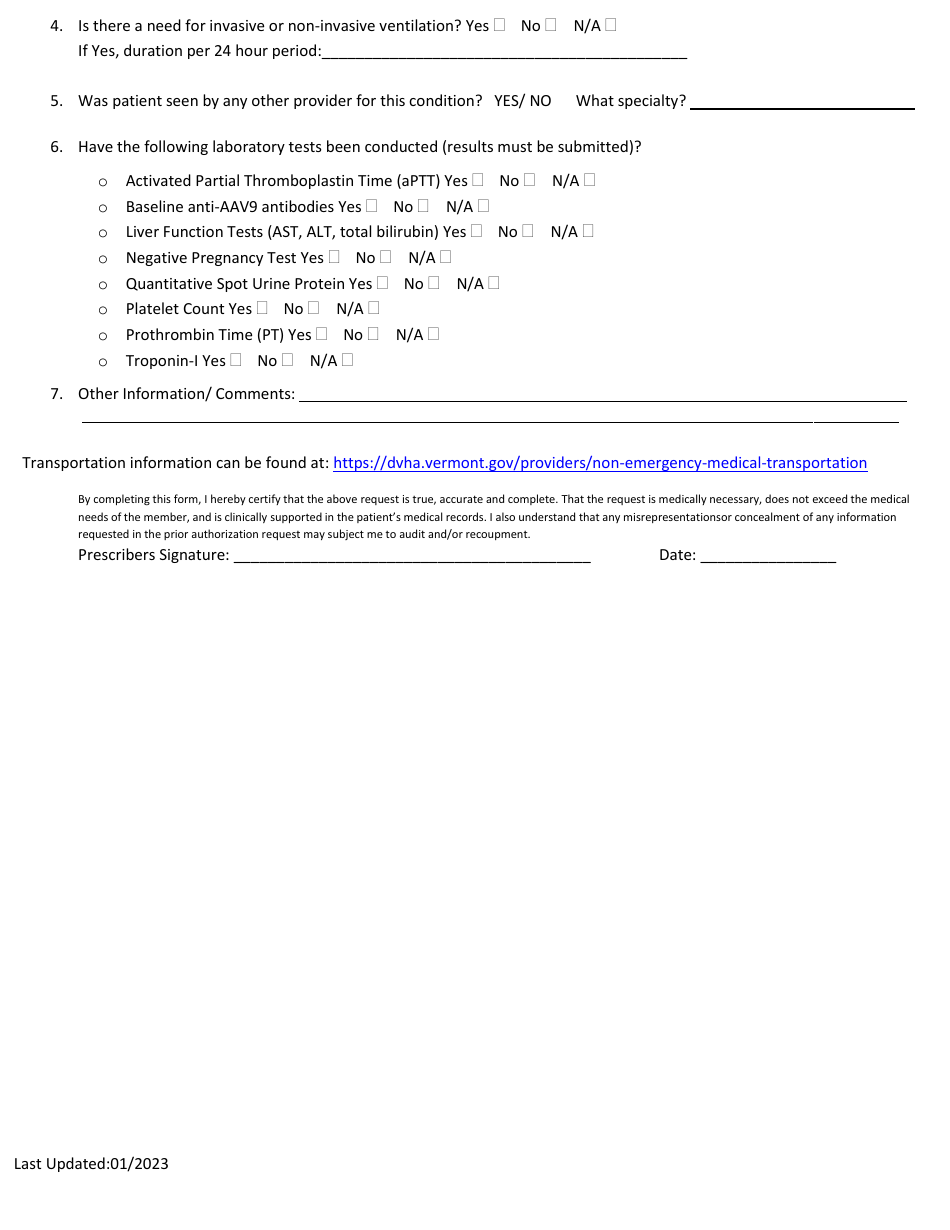
Q: What information is required in the Prior Authorization Request Form for SMA Therapy?
A: The form typically requires information about the patient, medical history, treatment plan, and supporting documentation.
Q: How long does it take for the Prior Authorization Request to be approved?
A: The approval time for a Prior Authorization Request can vary, but it typically takes a few days to a few weeks.
Q: What should I do if my Prior Authorization Request is denied?
A: If your Prior Authorization Request is denied, you can appeal the decision or explore other options with your healthcare provider or insurance company.
Q: Does the Prior Authorization Request Form guarantee coverage for SMA Therapy?
A: No, the Prior Authorization Request Form does not guarantee coverage. The final decision is made by the insurance company based on their coverage policies.
Form Details:
- Released on January 1, 2023;
- The latest edition currently provided by the Department of Vermont Health Access;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Department of Vermont Health Access.