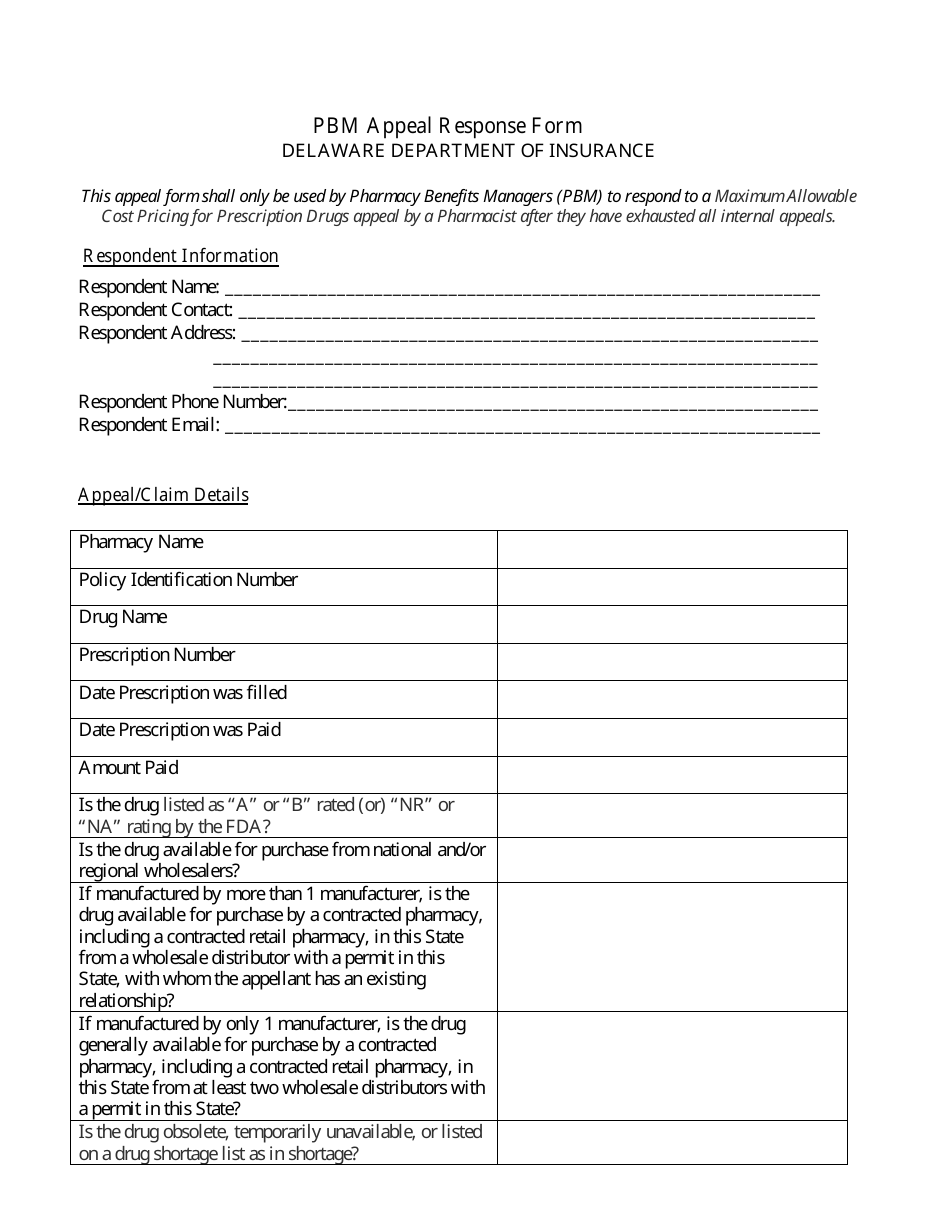
Pbm Appeal Response Form - Delaware
Pbm Appeal Response Form is a legal document that was released by the Delaware Department of Insurance - a government authority operating within Delaware.
FAQ
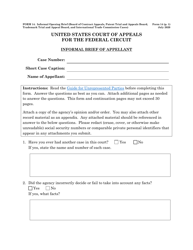
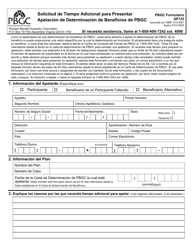
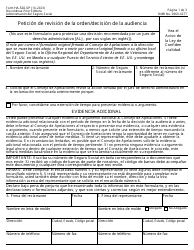
Q: What is a PBM appeal response form?
A: A PBM appeal response form is a document used to respond to a decision made by a Pharmacy Benefit Manager (PBM) regarding a prescription claim.
Q: What is a PBM?
A: A PBM stands for Pharmacy Benefit Manager. It is a third-party administrator that manages prescription drug plans for insurance companies, employers, and government programs.
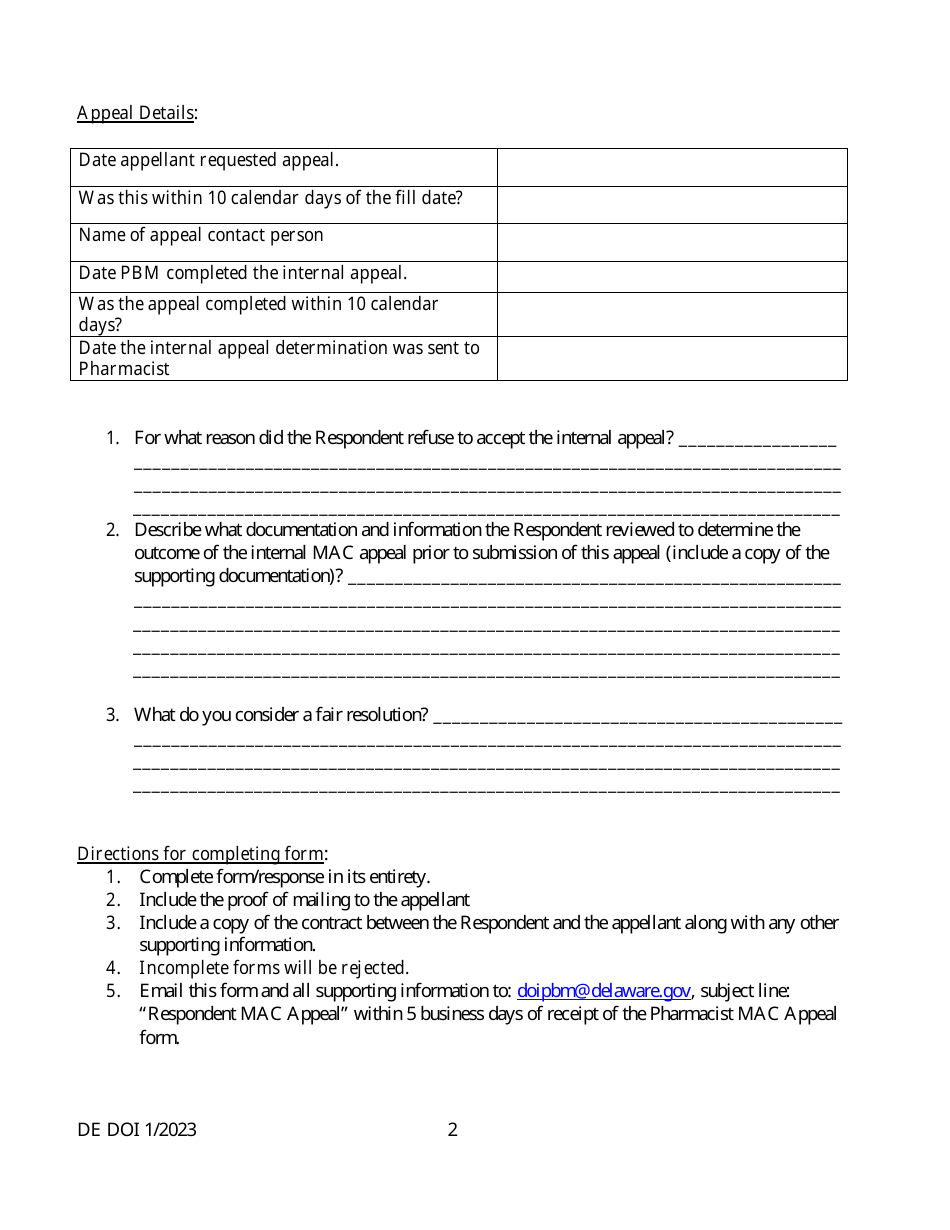
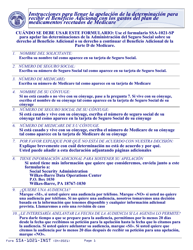
Q: How do I fill out a PBM appeal response form?
A: To fill out a PBM appeal response form, you typically need to provide your personal information, details about the prescription claim, and the reason for your appeal.
Q: Why would I need to fill out a PBM appeal response form?
A: You would need to fill out a PBM appeal response form if you disagree with a decision made by the PBM regarding your prescription claim and want to appeal that decision.
Form Details:
- Released on January 1, 2023;
- The latest edition currently provided by the Delaware Department of Insurance;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Delaware Department of Insurance.