This version of the form is not currently in use and is provided for reference only. Download this version of
Form HLTH5388
for the current year.
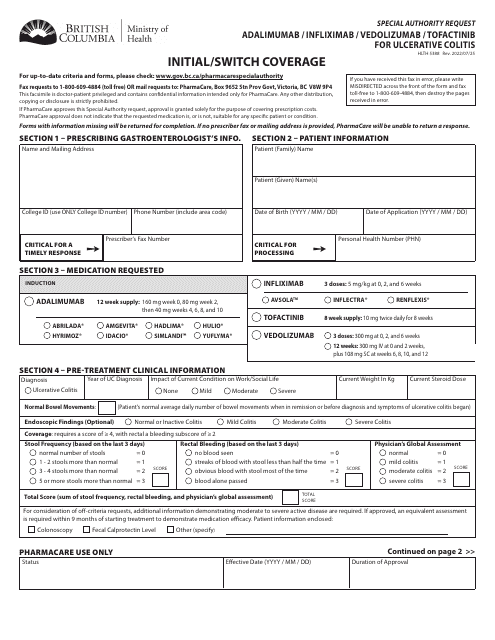
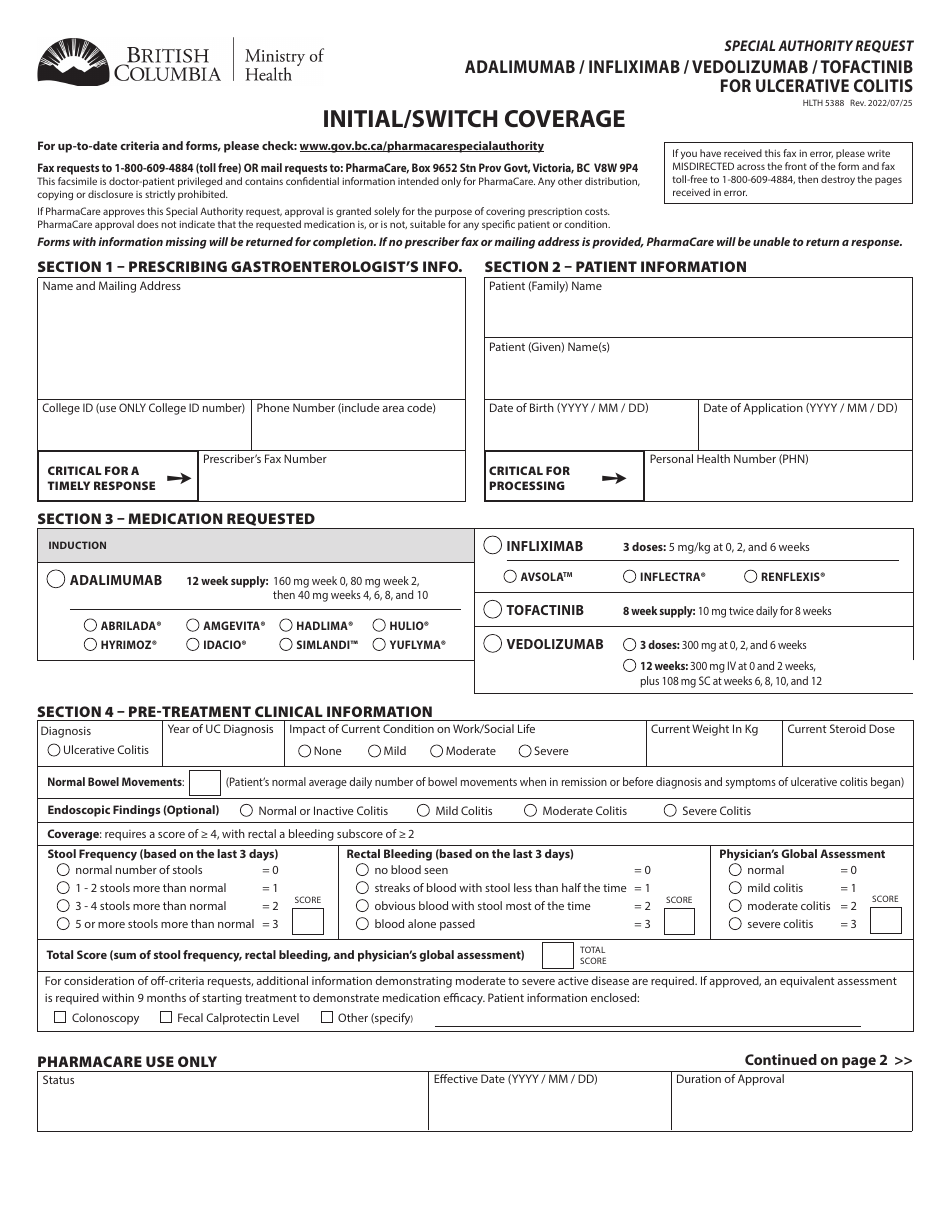
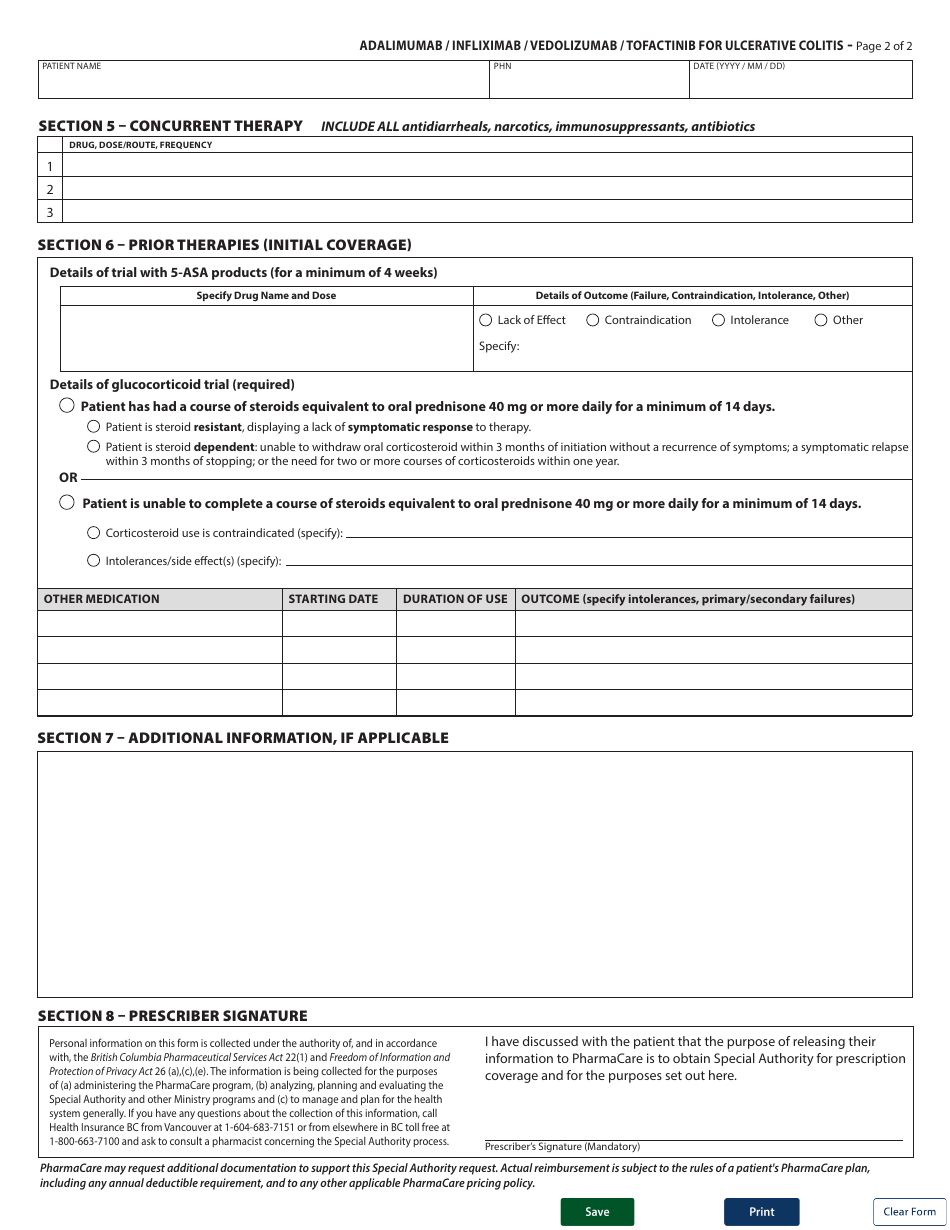
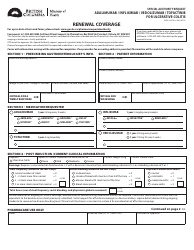
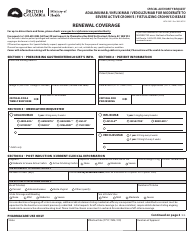
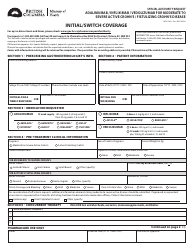
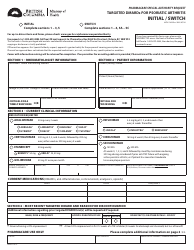
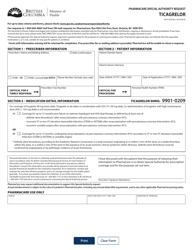
Form HLTH5388 Special Authority Request - Adalimumab / Infliximab / Vedolizumab / Tofactinib for Ulcerative Colitis - Initial / Switch Coverage - British Columbia, Canada
Form HLTH5388 Special Authority Request - Adalimumab/Infliximab/Vedolizumab/Tofactinib for Ulcerative Colitis - Initial/Switch Coverage - British Columbia, Canada is used to request special authorization for coverage of specific medications (Adalimumab, Infliximab, Vedolizumab, or Tofactinib) for the treatment of Ulcerative Colitis in British Columbia, Canada. This form is used when a patient requires these medications and their coverage needs to be approved by the provincial health authorities.
The Form HLTH5388 Special Authority Request - Adalimumab/Infliximab/Vedolizumab/Tofactinib for Ulcerative Colitis - Initial/Switch Coverage in British Columbia, Canada, is typically filed by the prescribing physician or healthcare provider.
FAQ
Q: What is the purpose of this form?
A: The form is for requesting special authority coverage for the medications Adalimumab, Infliximab, Vedolizumab, and Tofacitinib for the treatment of Ulcerative Colitis in British Columbia, Canada.
Q: Who can use this form?
A: This form can be used by healthcare professionals in British Columbia, Canada who are requesting special authority coverage for their patients with Ulcerative Colitis.
Q: Which medications can be requested using this form?
A: The medications Adalimumab, Infliximab, Vedolizumab, and Tofacitinib can be requested using this form.
Q: What is Ulcerative Colitis?
A: Ulcerative Colitis is a chronic inflammatory bowel disease that affects the large intestine and rectum.
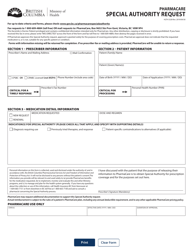
Q: What is special authority coverage?
A: Special authority coverage is a process through which healthcare professionals can request coverage for medications that are not automatically covered under a provincial healthcare plan.
Q: Who is eligible for special authority coverage?
A: Patients with specific medical conditions, as determined by the provincial healthcare authority, may be eligible for special authority coverage.
Q: What information is required on this form?
A: The form requires information about the patient's diagnosis, previous treatments, and relevant medical history, as well as information about the healthcare professional submitting the request.
Q: Is there a cost associated with this form?
A: There may be costs associated with the medications requested, depending on the patient's coverage and the specific healthcare plan.
Q: Are there any limitations on coverage?
A: Coverage for these medications may have certain limitations, such as specific criteria for eligibility or limitations on dosage or duration of treatment.