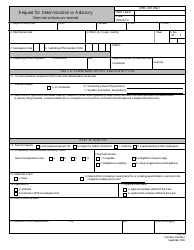
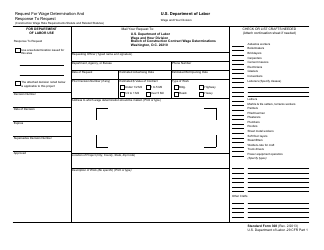
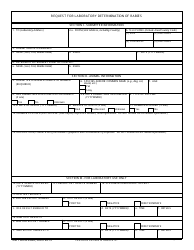
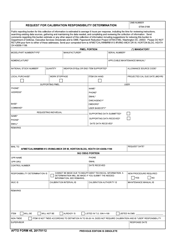
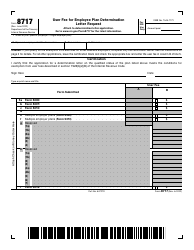
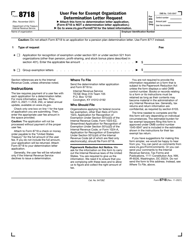
Instructions for Request for Coverage Determination
This document contains official instructions for Request for Coverage Determination , a legal form released by the U.S. Pension Benefit Guaranty Corporation. The up-to-date fillable form can be downloaded through this link.
FAQ
Q: What is a Request for Coverage Determination?
A: A Request for Coverage Determination is a formal request you make to your insurance company to determine if a specific medical treatment or service is covered under your insurance plan.
Q: Why would I need to make a Request for Coverage Determination?
A: You would need to make a Request for Coverage Determination if you have a medical treatment or service that you believe should be covered by your insurance plan, but your insurance company has not yet made a decision on the coverage.
Q: How do I make a Request for Coverage Determination?
A: To make a Request for Coverage Determination, you typically need to fill out a form provided by your insurance company. This form will require details about the medical treatment or service, including supporting documentation from your healthcare provider.
Q: What information should I include in my Request for Coverage Determination?
A: You should include details about the medical treatment or service you are requesting coverage for, as well as any supporting documentation from your healthcare provider. It's important to be as specific and detailed as possible.
Q: How long does it take to receive a decision on a Request for Coverage Determination?
A: The time it takes to receive a decision on a Request for Coverage Determination can vary. In some cases, you may receive a decision within a few days, while in other cases it may take several weeks.
Q: What should I do if my Request for Coverage Determination is denied?
A: If your Request for Coverage Determination is denied, you have the right to appeal the decision. Your insurance company should provide information on how to initiate an appeal.
Q: Can I get assistance with making a Request for Coverage Determination?
A: Yes, you can seek assistance from your healthcare provider or a representative from your insurance company's customer service department to help you with the process of making a Request for Coverage Determination.
Q: Are there any costs associated with making a Request for Coverage Determination?
A: It depends on your insurance plan. Some plans may charge a fee for processing a Request for Coverage Determination, while others may not. You should check with your insurance company to understand any associated costs.
Instruction Details:
- These 6-page instructions are available for download in PDF;
- The latest version provided by the issuing department;
- Up-to-date, printable, and free to use.
Download your copy of the instructions by clicking the link below or browse more forms, instructions and templates in our online library.