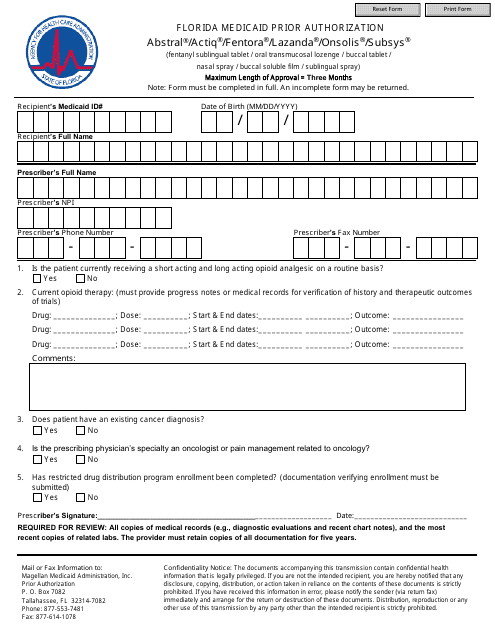
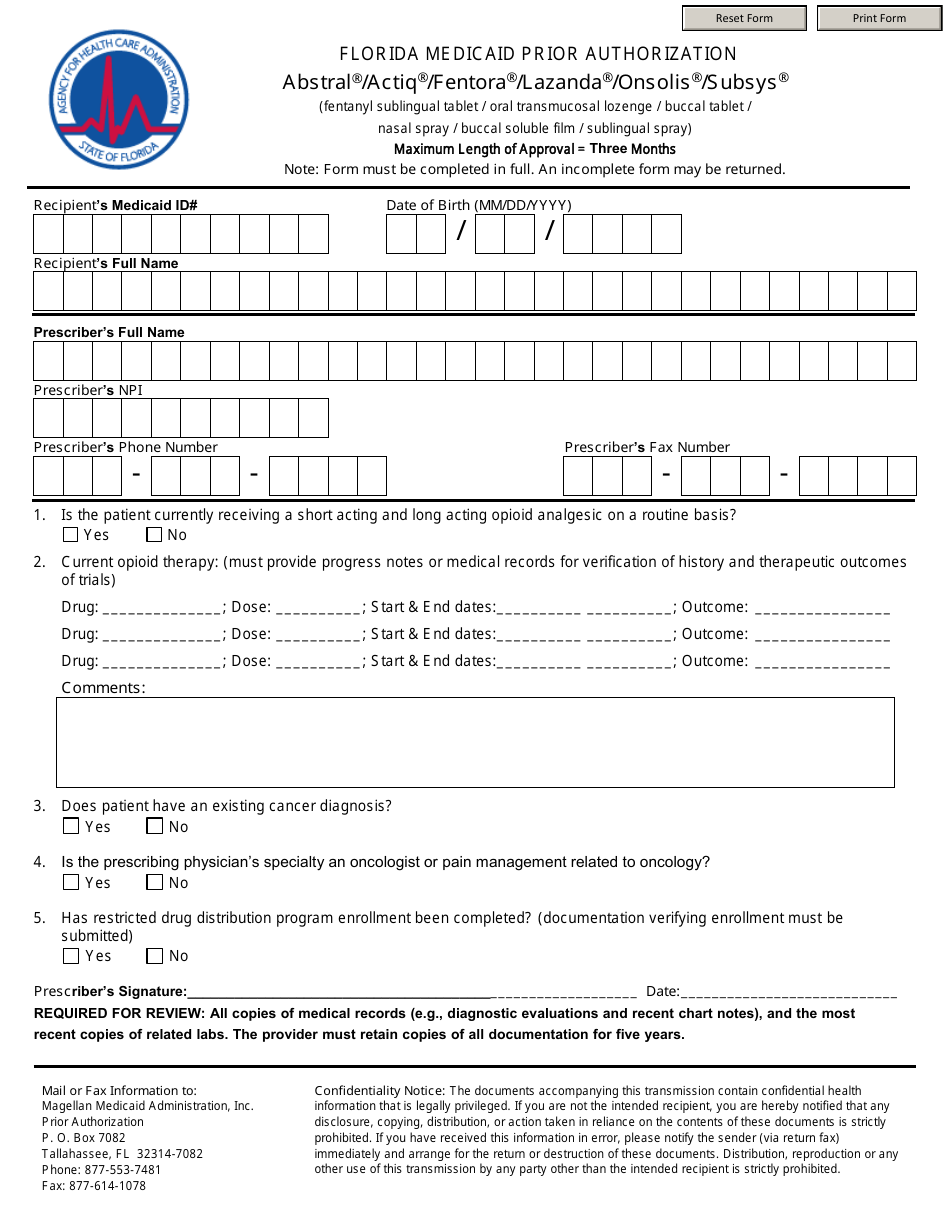
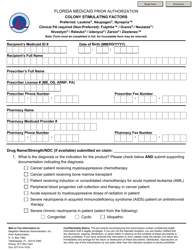
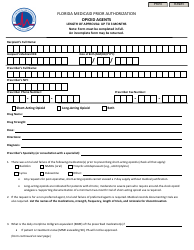
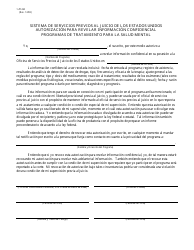
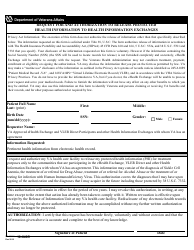
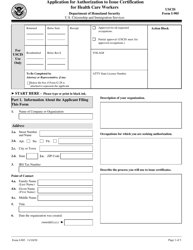
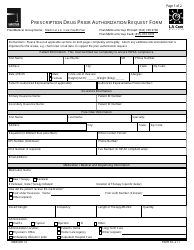
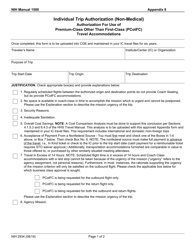
Florida Medicaid Prior Authorization - Abstral / Actiq / Fentora / Lazanda / Onsolis / Subsys - Florida
Florida Medicaid Prior Authorization - Abstral/Actiq/Fentora/Lazanda/Onsolis/Subsys is a legal document that was released by the Florida Agency For Health Care Administration - a government authority operating within Florida.
FAQ
Q: What is Medicaid?
A: Medicaid is a government health insurance program that provides healthcare coverage to eligible low-income individuals and families.
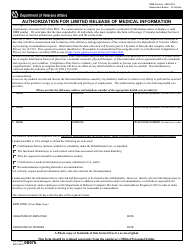
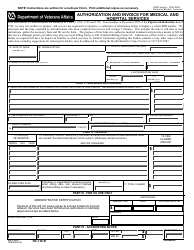
Q: What is prior authorization?
A: Prior authorization is a process by which healthcare providers must obtain approval from Medicaid before certain medications or treatments can be covered.
Q: What are Abstral, Actiq, Fentora, Lazanda, Onsolis, and Subsys?
A: Abstral, Actiq, Fentora, Lazanda, Onsolis, and Subsys are brand names for different forms of fentanyl, a strong opioid medication used to treat severe pain.
Q: Why is prior authorization required for these medications?
A: Prior authorization helps ensure that these potent opioids are prescribed appropriately and are medically necessary for the patient's condition.
Q: How can I get prior authorization for these medications?
A: To get prior authorization for Abstral, Actiq, Fentora, Lazanda, Onsolis, or Subsys, your healthcare provider will need to submit a request to Florida Medicaid and provide supporting documentation.
Q: What happens if prior authorization is not obtained?
A: If prior authorization is not obtained, Florida Medicaid may not cover the cost of these medications and you may have to pay for them out-of-pocket.
Q: Are there any alternative medications that do not require prior authorization?
A: Your healthcare provider can help you explore alternative medications that may be covered by Florida Medicaid without the need for prior authorization.
Form Details:
- The latest edition currently provided by the Florida Agency For Health Care Administration;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Florida Agency For Health Care Administration.