This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
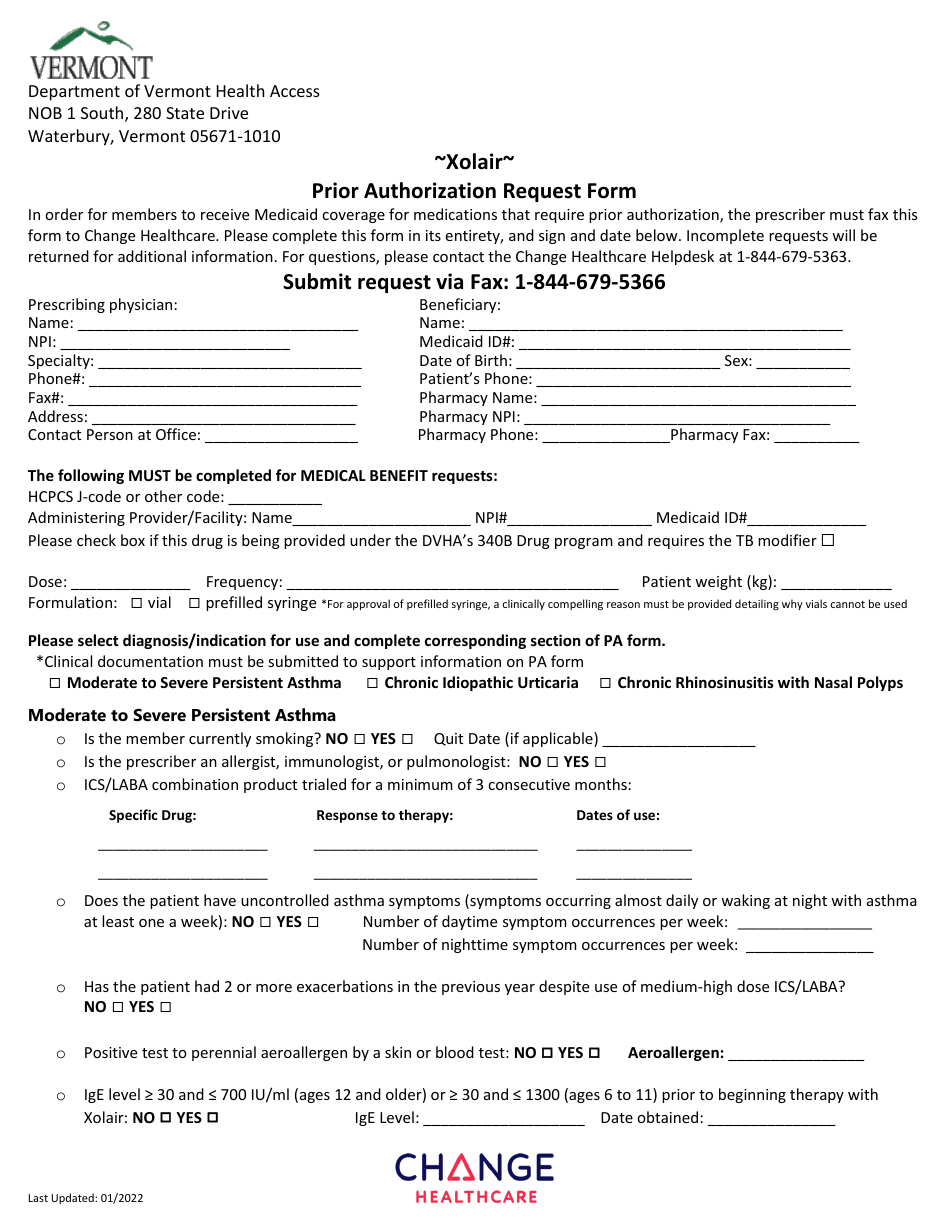
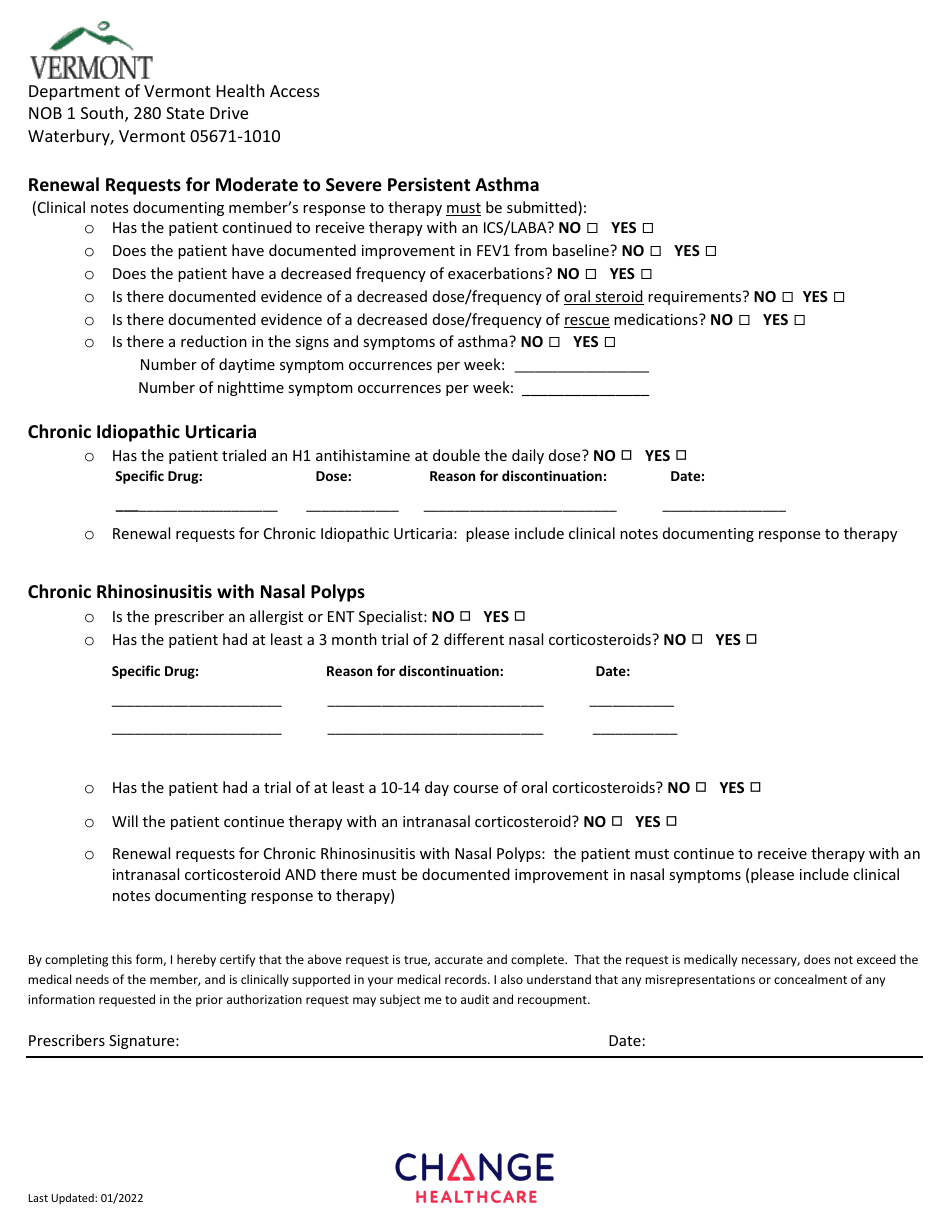
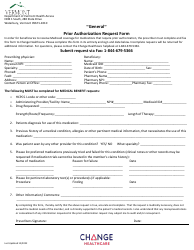
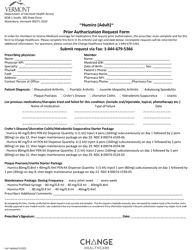
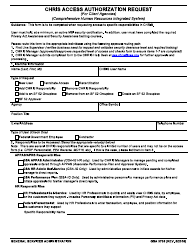
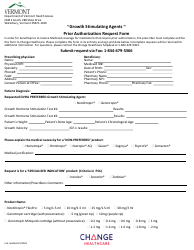
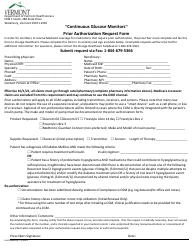
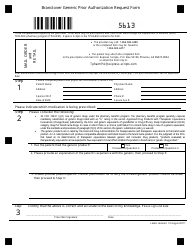
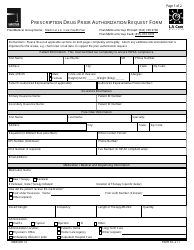
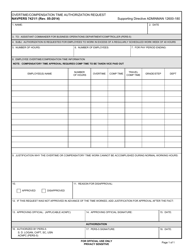
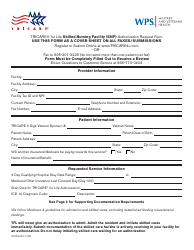
Xolair Prior Authorization Request Form - Vermont
Xolair Prior Authorization Request Form is a legal document that was released by the Department of Vermont Health Access - a government authority operating within Vermont.
FAQ
Q: What is Xolair?
A: Xolair is a medication used to treat severe asthma and chronic hives.
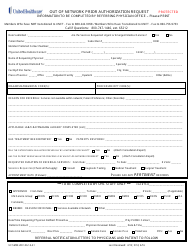
Q: What is a prior authorization request?
A: A prior authorization request is a process where your healthcare provider asks your insurance company to approve coverage for a specific medication or treatment.
Q: Why is a prior authorization necessary?
A: Prior authorization helps insurance companies ensure that the medication or treatment being requested is medically necessary and appropriate.
Q: Who needs to fill out the Xolair prior authorization request form?
A: Your healthcare provider will need to fill out the Xolair prior authorization request form on your behalf.
Q: What information is required on the Xolair prior authorization request form?
A: The Xolair prior authorization request form will ask for information such as your personal details, medical history, and the reason why Xolair is being prescribed.
Q: How long does it take for a prior authorization request to be approved?
A: The time it takes for a prior authorization request to be approved can vary, but it typically takes about 1-2 weeks.
Q: What should I do if my prior authorization request is denied?
A: If your prior authorization request is denied, you can work with your healthcare provider and insurance company to submit an appeal or explore other treatment options.
Form Details:
- Released on January 1, 2022;
- The latest edition currently provided by the Department of Vermont Health Access;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Department of Vermont Health Access.