This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
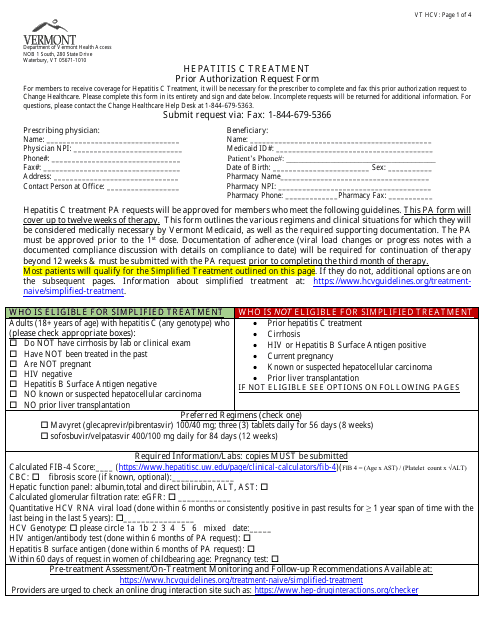
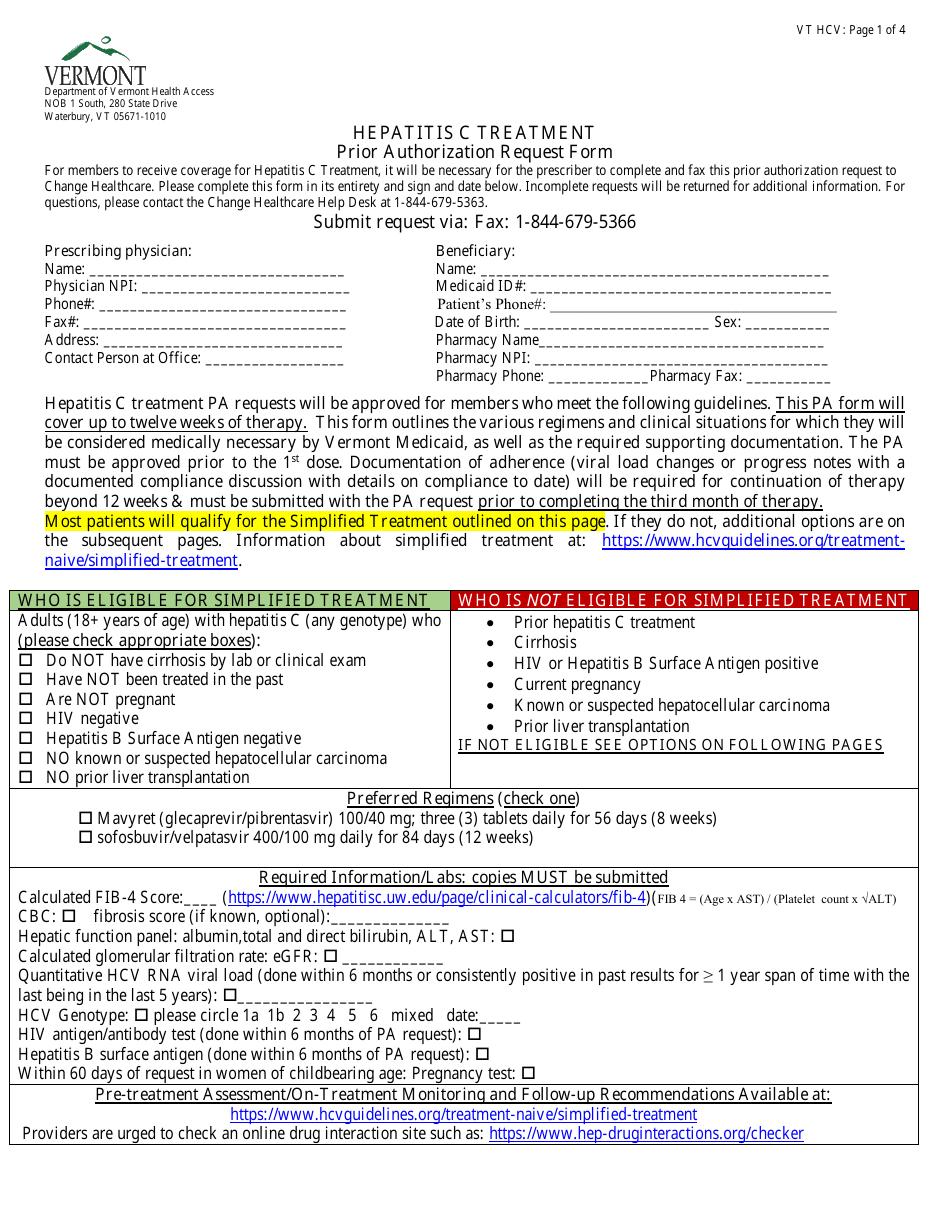
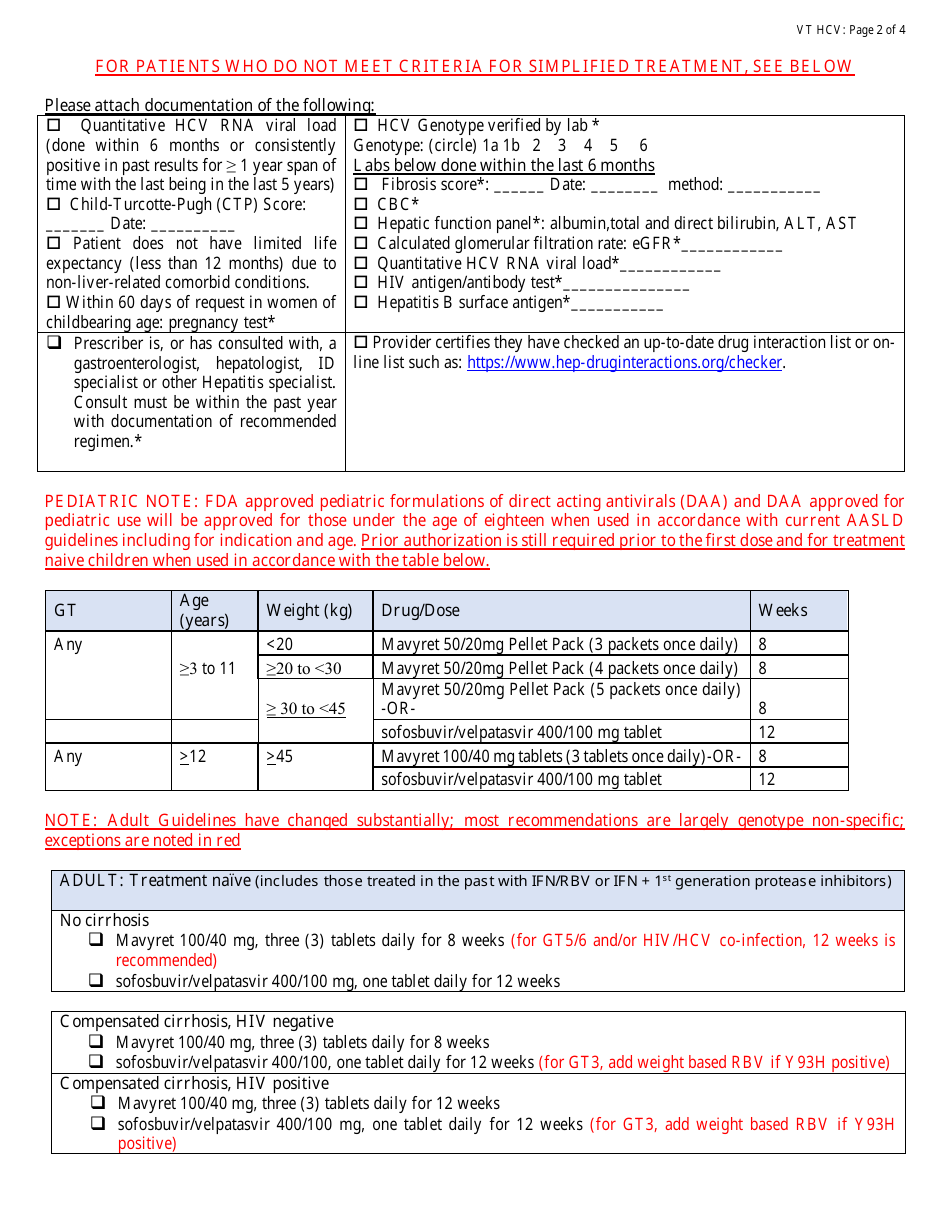
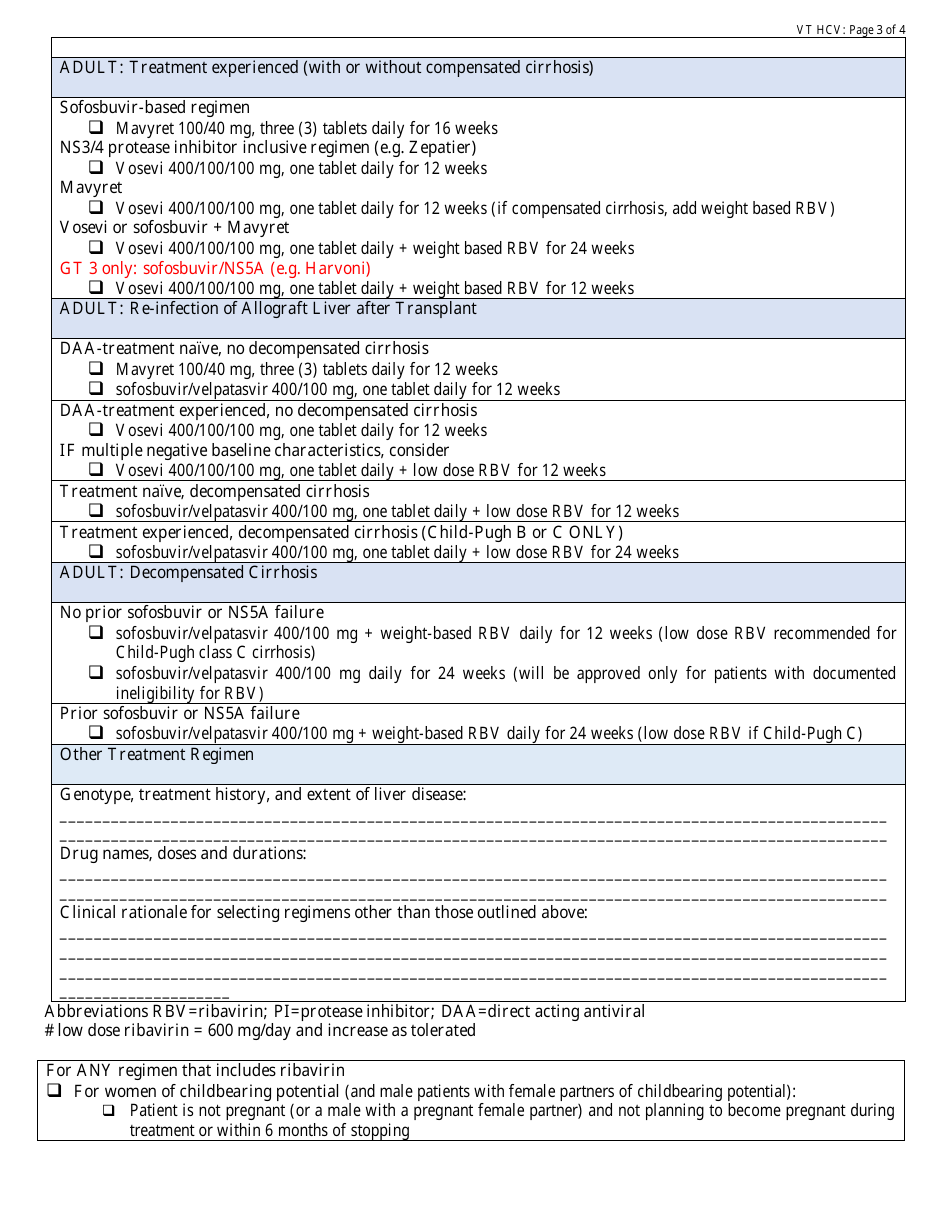
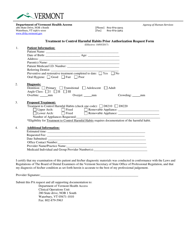
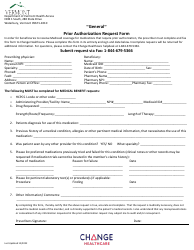
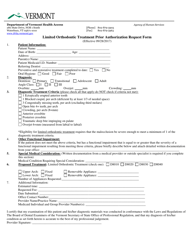
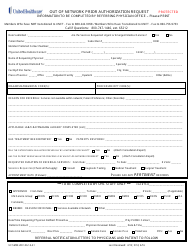
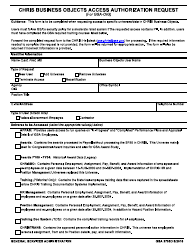
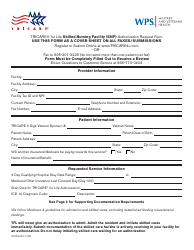
Hepatitis C Treatment Prior Authorization Request Form - Vermont
Hepatitis C Treatment Prior Authorization Request Form is a legal document that was released by the Department of Vermont Health Access - a government authority operating within Vermont.
FAQ
Q: What is the Hepatitis C Treatment Prior Authorization Request Form?
A: The Hepatitis C Treatment Prior Authorization Request Form is a document used in Vermont to request authorization for the treatment of Hepatitis C.
Q: Why is prior authorization required for Hepatitis C treatment?
A: Prior authorization is required for Hepatitis C treatment to ensure appropriate and cost-effective use of medications.
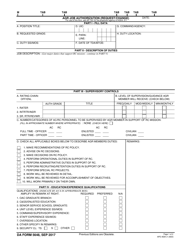
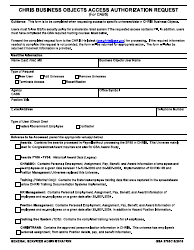
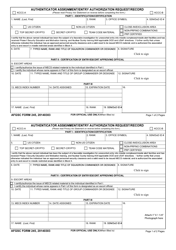
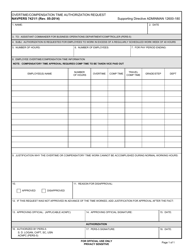
Q: What information is required in the form?
A: The form typically requires information about the patient, healthcare provider, medication, medical history, and supporting documentation.
Q: How long does it take to process the prior authorization request?
A: The processing time for a prior authorization request can vary, but it is usually within a few days to a couple of weeks.
Q: Can my healthcare provider help me with the form?
A: Yes, your healthcare provider can assist you in completing the Hepatitis C Treatment Prior Authorization Request Form.
Q: Does prior authorization guarantee coverage for Hepatitis C treatment?
A: Prior authorization does not guarantee coverage, but it is a necessary step to determine eligibility and obtain coverage for Hepatitis C treatment.
Q: What should I do if my prior authorization request is denied?
A: If your prior authorization request is denied, you can appeal the decision or explore alternative treatment options with your healthcare provider.
Q: Is there a cost associated with submitting the prior authorization request?
A: There may be a cost associated with submitting the prior authorization request, such as copayments or deductibles, depending on your insurance coverage.
Form Details:
- The latest edition currently provided by the Department of Vermont Health Access;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Department of Vermont Health Access.