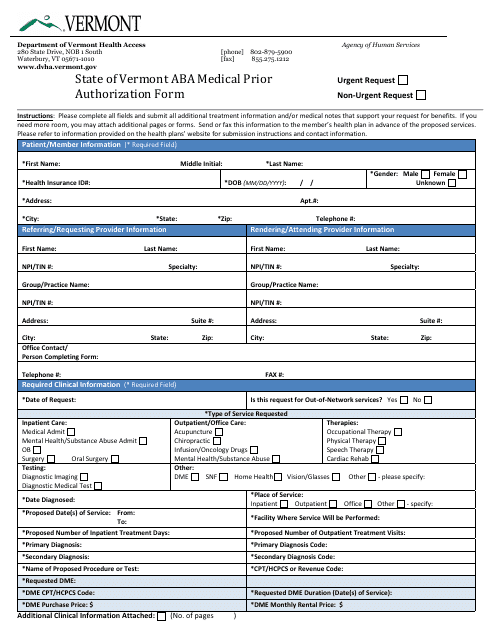
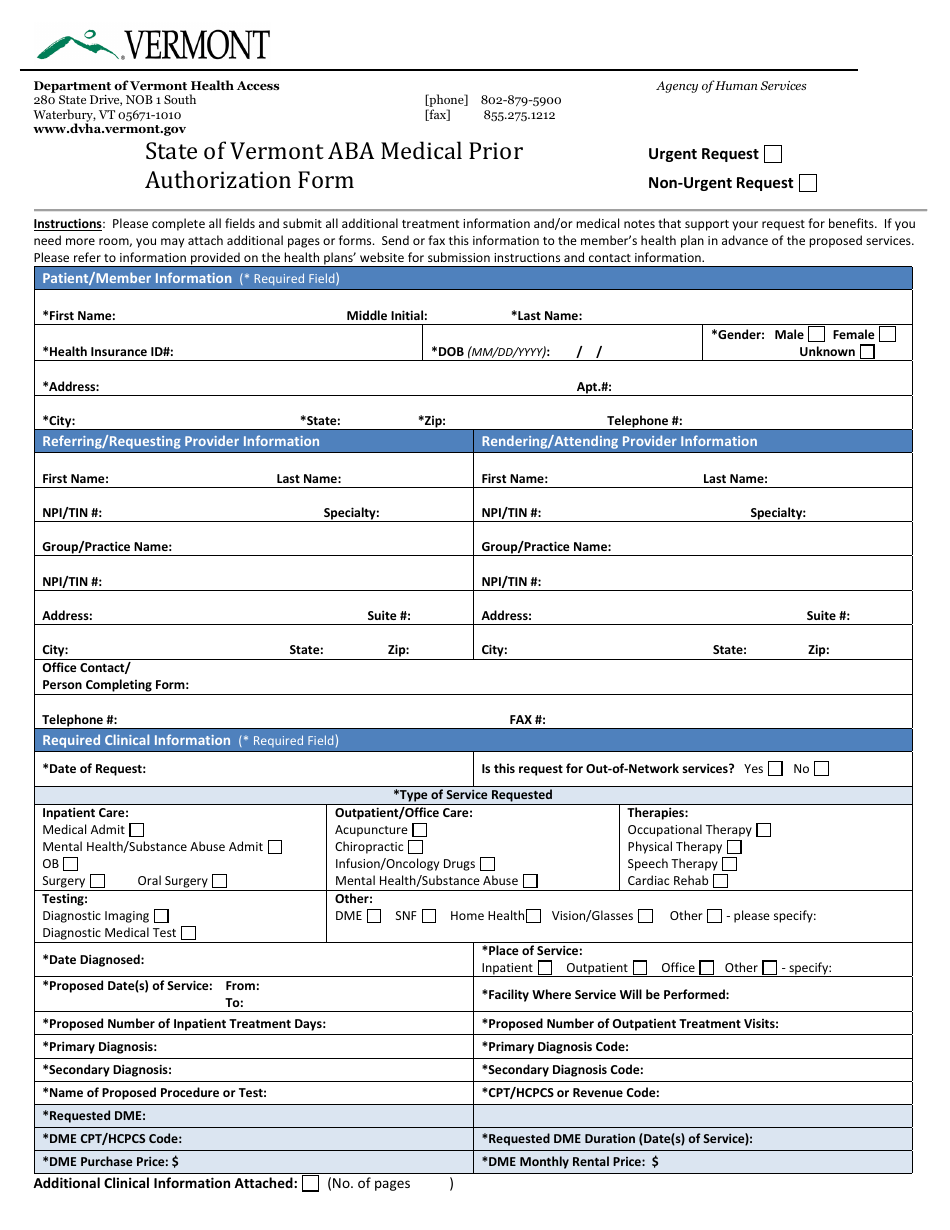
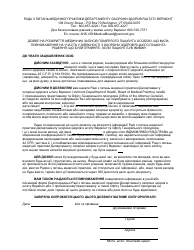
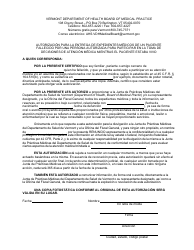
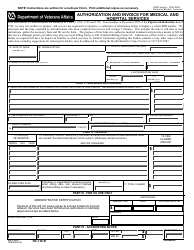
Aba Medical Prior Authorization Form - Vermont
Aba Medical Prior Authorization Form is a legal document that was released by the Department of Vermont Health Access - a government authority operating within Vermont.
FAQ
Q: What is an ABa medical prior authorization form?
A: An ABa medical prior authorization form is a document used to request approval from an insurance company before receiving certain medical treatments or procedures.
Q: Why is a prior authorization form needed?
A: A prior authorization form is needed to confirm that the medical treatment or procedure is medically necessary and covered by the insurance plan.
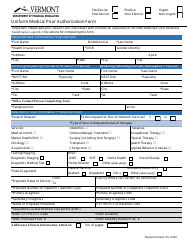
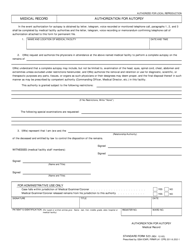
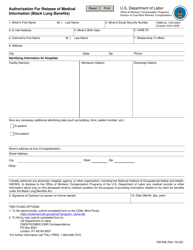
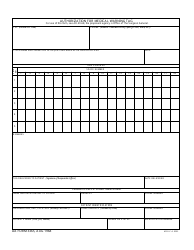
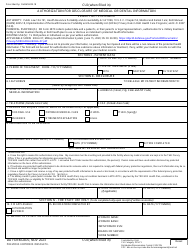
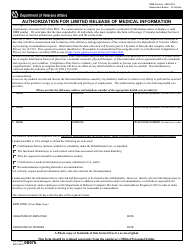
Q: What information is required on the ABa medical prior authorization form?
A: The ABa medical prior authorization form typically requires information such as the patient's personal details, the healthcare provider's information, the specific treatment or procedure being requested, and any supporting documentation.
Q: What should I do after completing the ABa medical prior authorization form?
A: After completing the ABa medical prior authorization form, you should submit it to your health insurance provider for review and wait for their decision.
Q: How long does the prior authorization process take?
A: The prior authorization process can vary in length, but it typically takes a few days to a few weeks for the insurance provider to review the form and make a decision.
Q: What happens if the ABa medical prior authorization request is denied?
A: If the ABa medical prior authorization request is denied, you can appeal the decision and provide additional supporting documentation to support your case.
Q: Are there any alternatives to the ABa medical prior authorization process?
A: Yes, there may be alternative options such as requesting a peer-to-peer review or exploring other treatment options that do not require prior authorization.
Q: Can I still receive the medical treatment or procedure without prior authorization?
A: In some cases, you may still be able to receive the medical treatment or procedure without prior authorization, but you may be responsible for paying the full cost out of pocket.
Q: Is the ABa medical prior authorization process the same across all insurance providers?
A: The ABa medical prior authorization process can vary slightly between different insurance providers, so it's important to carefully review the specific requirements of your insurance plan.
Form Details:
- The latest edition currently provided by the Department of Vermont Health Access;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Department of Vermont Health Access.