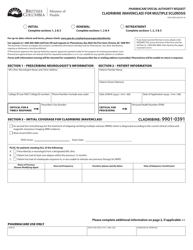
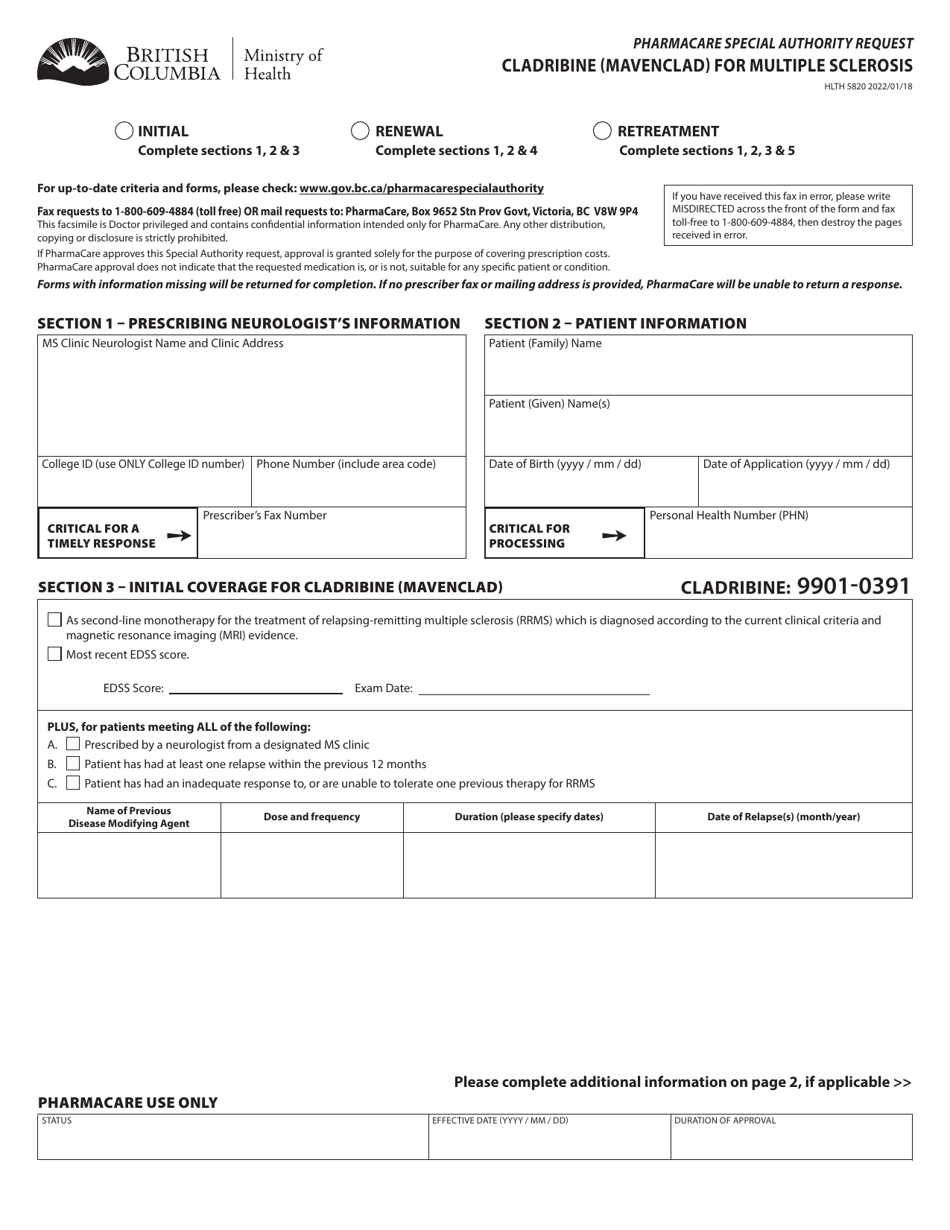
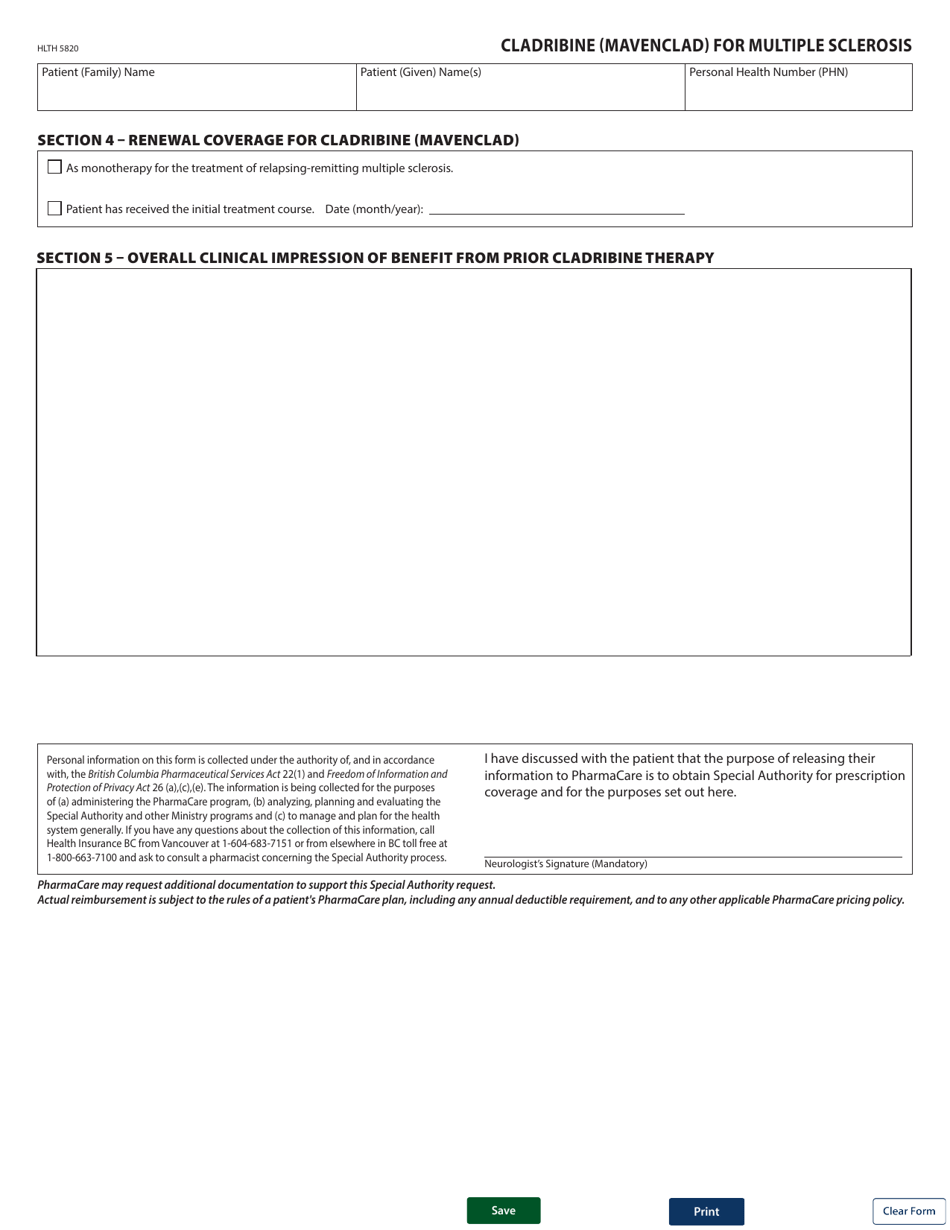
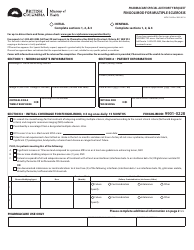
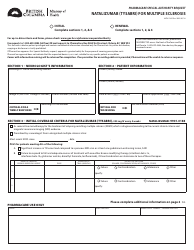
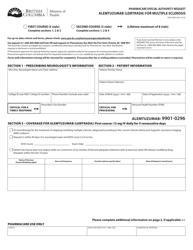
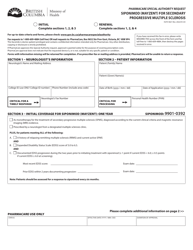
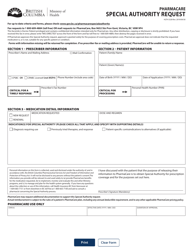
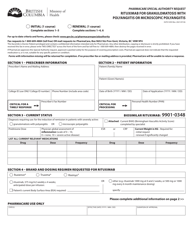
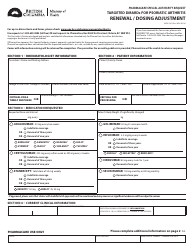
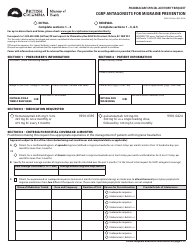
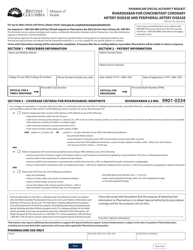
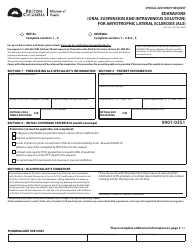
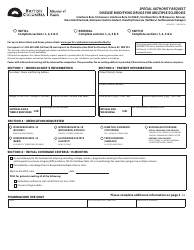
Form HLTH5820 Pharmacare Special Authority Request - Cladribine (Mavenclad) for Multiple Sclerosis - British Columbia, Canada
Form HLTH5820 Pharmacare Special Authority Request - Cladribine (Mavenclad) for Multiple Sclerosis - British Columbia, Canada is used to request special authority coverage for the medication Cladribine, also known as Mavenclad, for the treatment of Multiple Sclerosis in the province of British Columbia, Canada.
The Form HLTH5820 Pharmacare Special Authority Request for Cladribine (Mavenclad) for Multiple Sclerosis in British Columbia, Canada is typically filed by the patient or their healthcare provider.
FAQ
Q: What is a Special Authority Request?
A: A Special Authority Request is a request made by a healthcare provider to obtain coverage for a specific medication or treatment that may not be covered under the regular drug plan.
Q: What is Cladribine (Mavenclad)?
A: Cladribine, also known as Mavenclad, is a medication used for the treatment of multiple sclerosis.
Q: What is Multiple Sclerosis?
A: Multiple sclerosis is a chronic disease that affects the central nervous system, causing a variety of symptoms such as fatigue, difficulty walking, and problems with coordination and balance.
Q: Who can submit a Special Authority Request for Cladribine?
A: A healthcare provider, such as a doctor or specialist, can submit a Special Authority Request for Cladribine on behalf of their patient.
Q: Why would someone need to submit a Special Authority Request for Cladribine?
A: Someone may need to submit a Special Authority Request for Cladribine if the medication is not covered under their regular drug plan or if they do not meet the specific criteria for coverage.
Q: Who determines the approval or denial of a Special Authority Request?
A: The approval or denial of a Special Authority Request is determined by the relevant healthcare authority, such as the Pharmacare program in British Columbia, Canada.
Q: What happens if a Special Authority Request is approved?
A: If a Special Authority Request is approved, the medication or treatment requested will be covered under the patient's drug plan, and they will be able to obtain it at no or reduced cost.
Q: What happens if a Special Authority Request is denied?
A: If a Special Authority Request is denied, the patient may have to explore other options for obtaining the medication or treatment, such as private insurance or financial assistance programs.