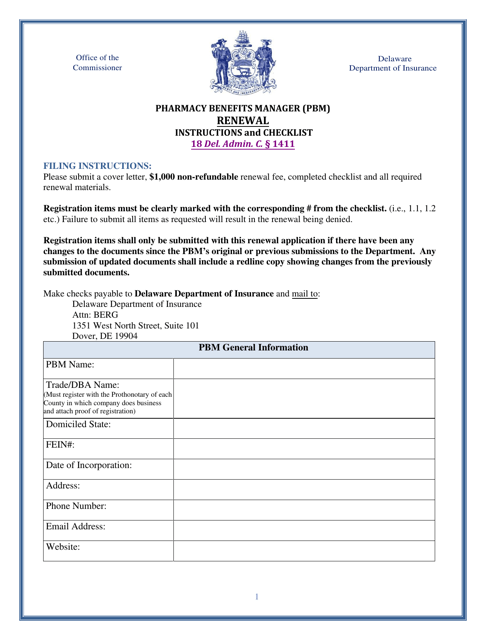
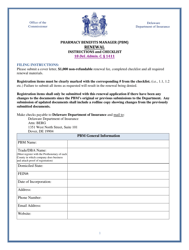
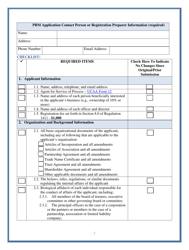
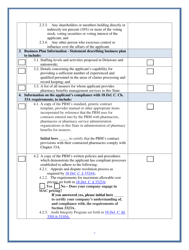
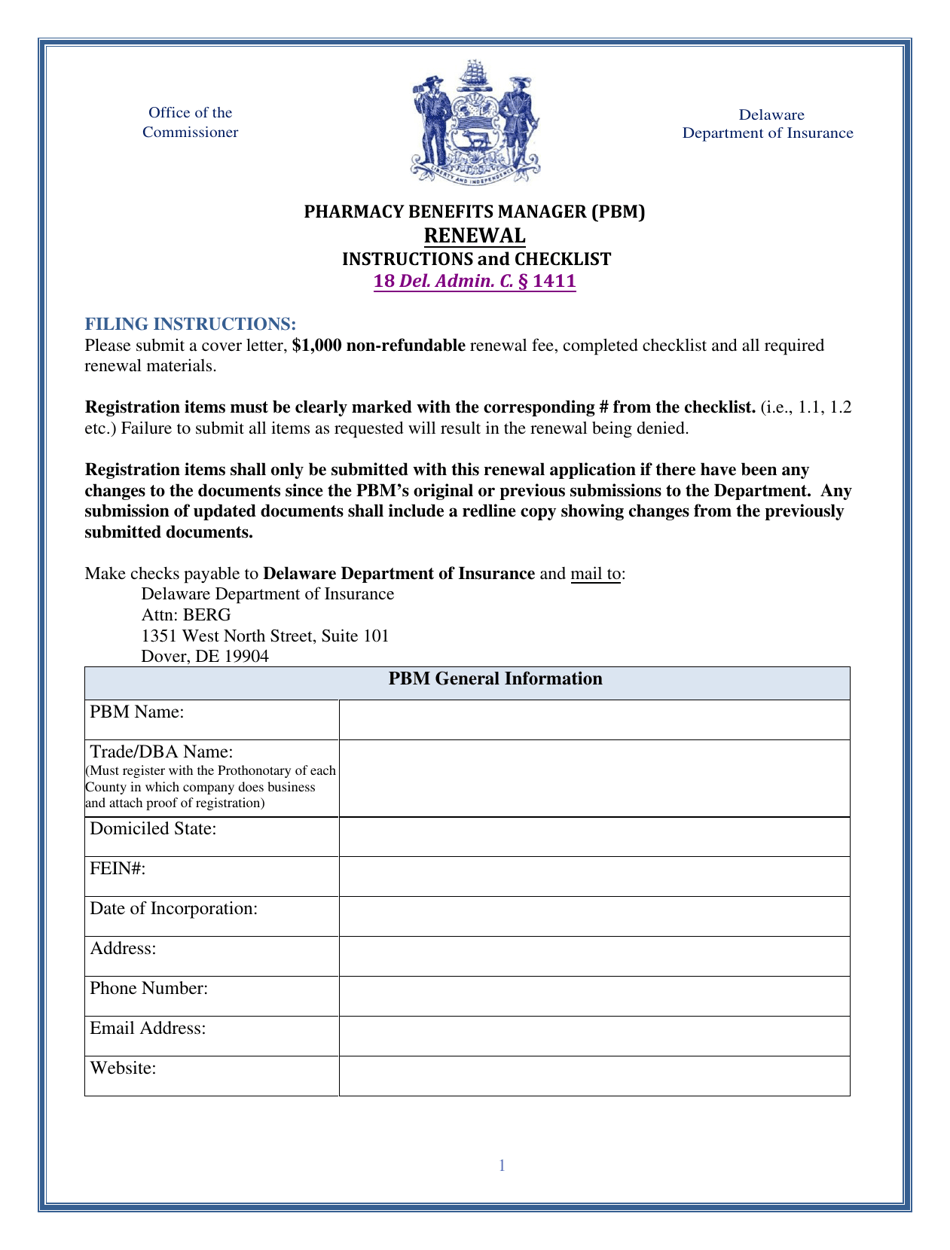
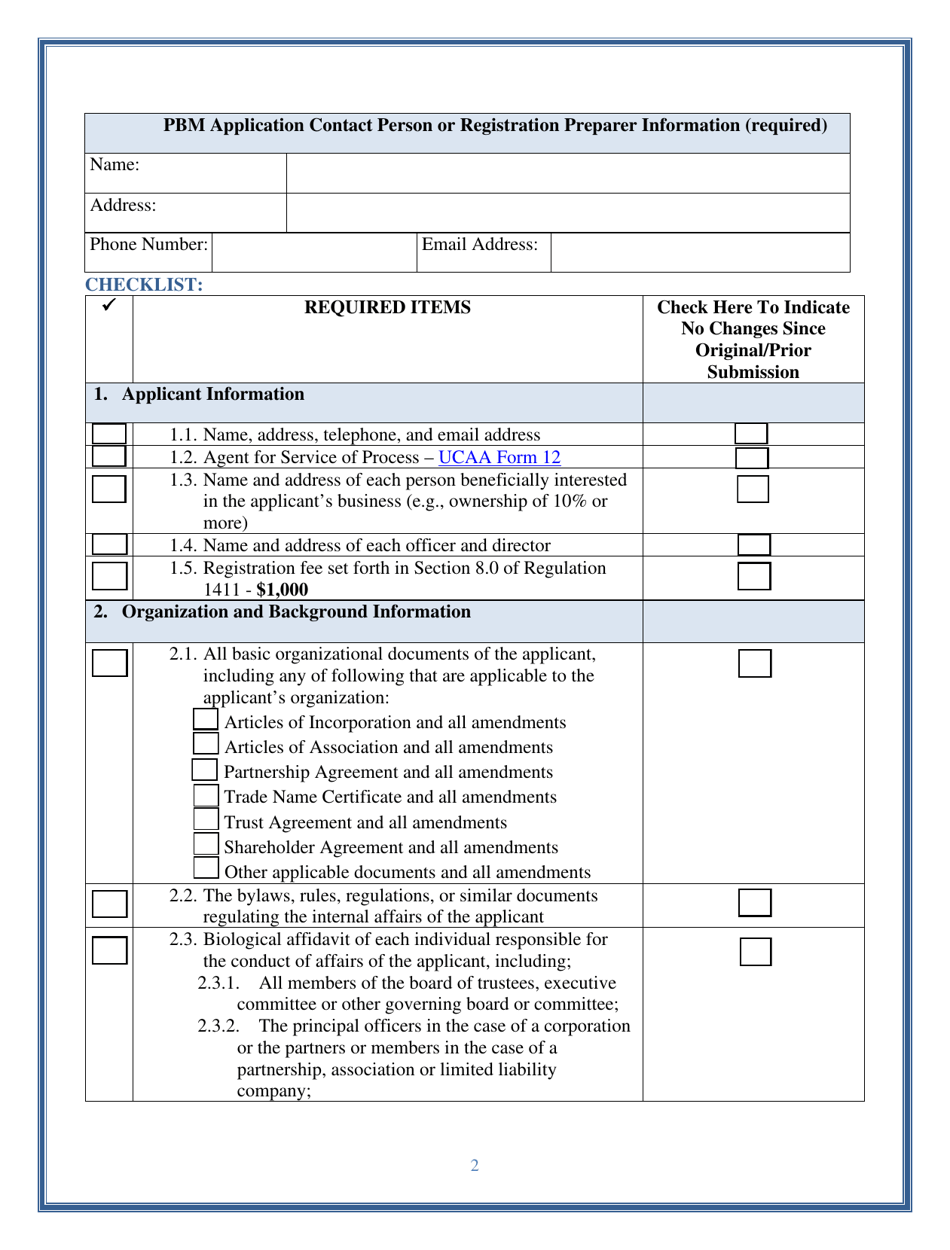
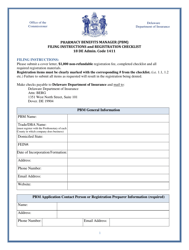
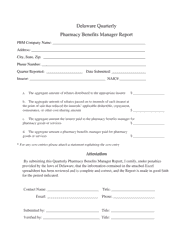
Pharmacy Benefits Manager (Pbm) Renewal - Delaware
Pharmacy Benefits Manager (Pbm) Renewal is a legal document that was released by the Delaware Department of Insurance - a government authority operating within Delaware.
FAQ
Q: What is a Pharmacy Benefits Manager (PBM)?
A: A Pharmacy Benefits Manager (PBM) is a third-party administrator that manages prescription drug benefits on behalf of health insurance plans.
Q: What does a PBM do?
A: A PBM negotiates with drug manufacturers, establishes pharmacy networks, processes and pays prescription claims, and manages formularies.
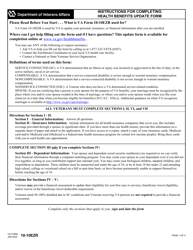
Q: Why is PBM renewal important?
A: PBM renewal is important because it ensures continued access to affordable and quality prescription drug benefits for plan participants.
Q: How often does PBM renewal occur?
A: PBM renewal typically occurs on an annual basis.
Q: Who is responsible for PBM renewal?
A: The entity that contracts with the PBM, such as a health insurance plan or employer, is responsible for PBM renewal.
Q: What should be considered during PBM renewal?
A: During PBM renewal, factors such as pricing, network adequacy, formulary coverage, and customer service should be considered.
Q: Are there any specific considerations for PBM renewal in Delaware?
A: Specific considerations for PBM renewal in Delaware may vary depending on the individual contract and the needs of the plan or employer.
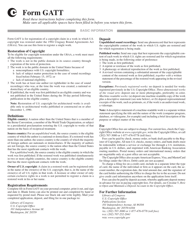
Form Details:
- The latest edition currently provided by the Delaware Department of Insurance;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Delaware Department of Insurance.