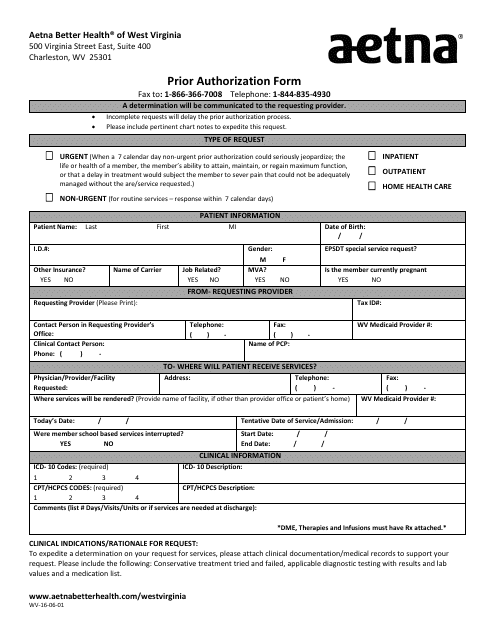
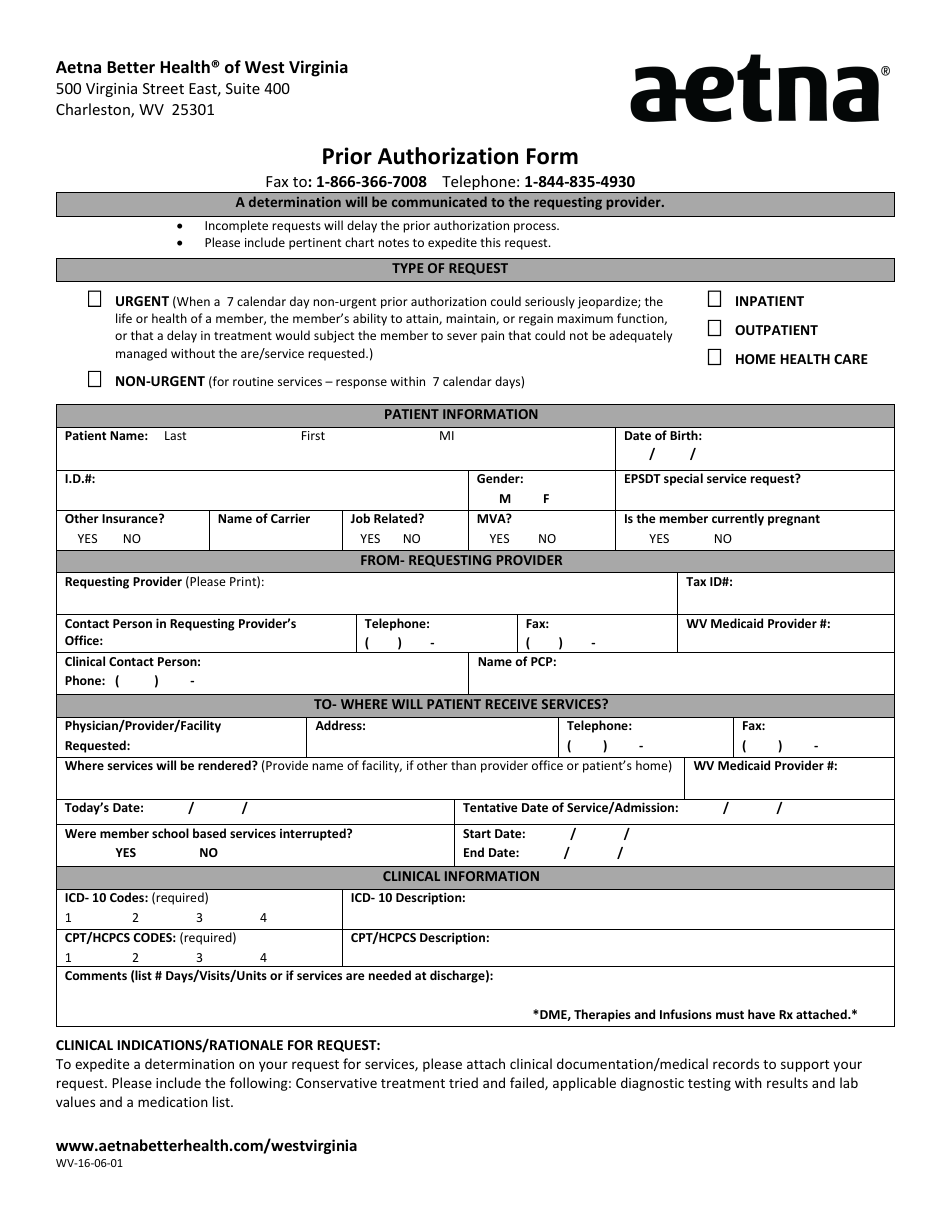
Form WV-16-06-01 Prior Authorization Form - Aetna - Charleston, West Virginia
The Form WV-16-06-01 Prior Authorization Form is used by Aetna, a healthcare insurance company, in Charleston, West Virginia. It is used to request prior authorization for certain medical procedures, treatments, or medications.
The health care provider or the patient files the Form WV-16-06-01 Prior Authorization Form with Aetna in Charleston, West Virginia.
FAQ
Q: What is WV-16-06-01 Prior Authorization Form?
A: WV-16-06-01 Prior Authorization Form is a specific form used by Aetna in Charleston, West Virginia for obtaining prior authorization for certain medical services or treatments.
Q: What is the purpose of the Prior Authorization Form?
A: The purpose of the Prior Authorization Form is to request approval from Aetna for specific medical services or treatments that may require prior authorization.
Q: Why is prior authorization required?
A: Prior authorization is required to ensure that certain medical services or treatments meet the necessary criteria for coverage and to maintain the quality and cost-effectiveness of healthcare services.
Q: How long does it take to get a prior authorization approved?
A: The time taken to get a prior authorization approved may vary depending on the complexity of the request and the specific requirements of the insurance provider. It is best to contact Aetna for an estimated timeline.