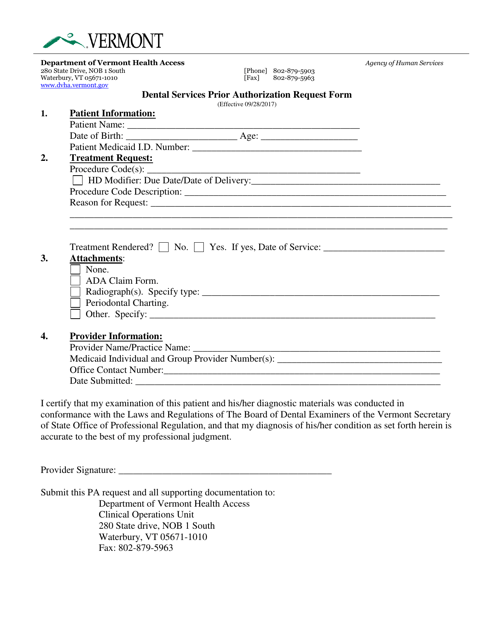
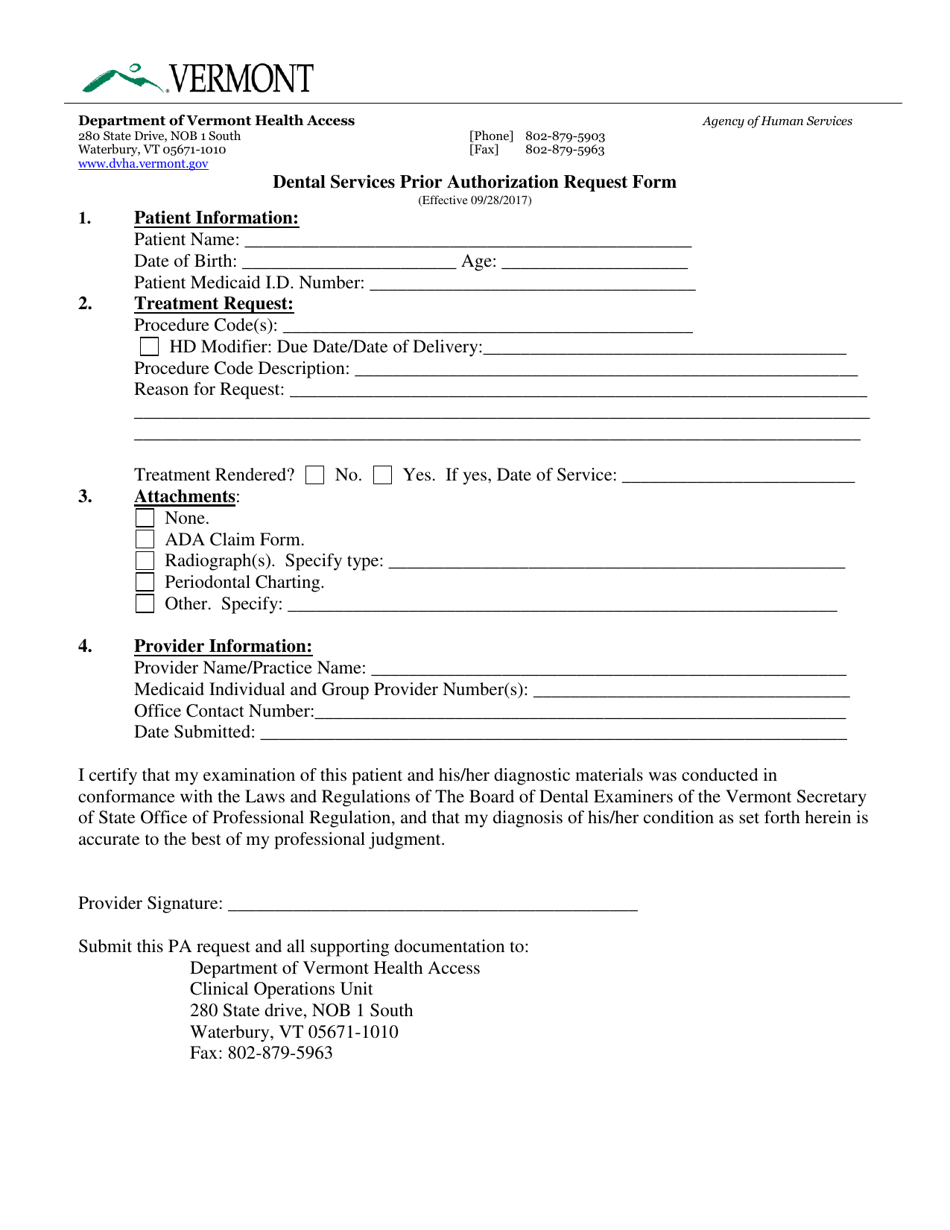
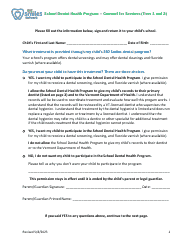
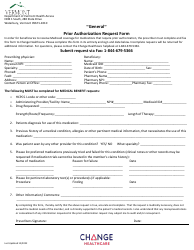
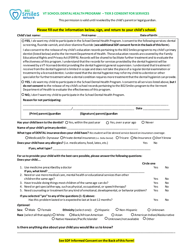
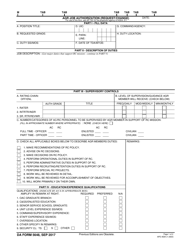
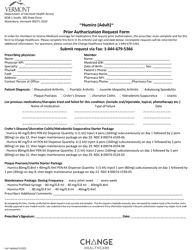
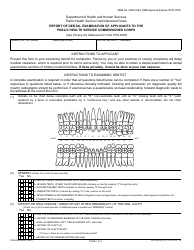
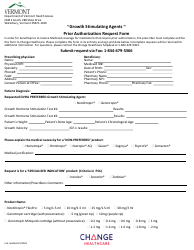
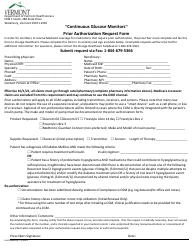
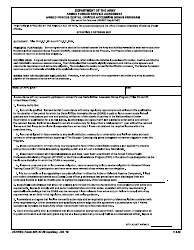
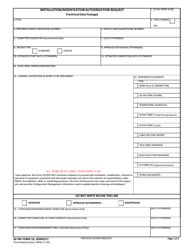
Dental Services Prior Authorization Request Form - Vermont
Dental Services Prior Authorization Request Form is a legal document that was released by the Department of Vermont Health Access - a government authority operating within Vermont.
FAQ
Q: What is the Dental Services Prior Authorization Request Form?
A: The Dental Services Prior Authorization Request Form is a form used in Vermont to request prior authorization for dental services.
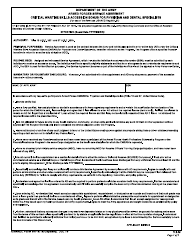
Q: Who needs to complete the Dental Services Prior Authorization Request Form?
A: Dental providers or their representatives need to complete the form.
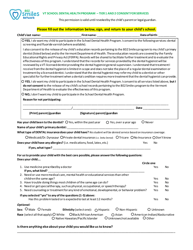
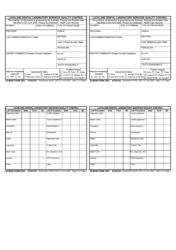
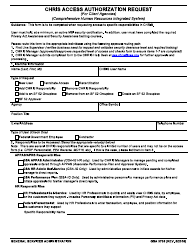
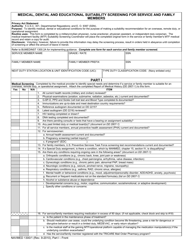
Q: What information is required on the Dental Services Prior Authorization Request Form?
A: The form requires information such as patient details, provider information, dental treatment details, and supporting documentation.
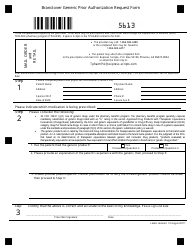
Q: Why is prior authorization necessary for dental services?
A: Prior authorization is necessary to ensure that the dental services are medically necessary and covered by the insurance provider.
Q: How long does it take to get a response to a Dental Services Prior Authorization Request?
A: The response time may vary, but it is typically within 10 business days.
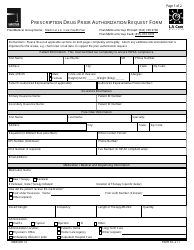
Q: What happens after a Dental Services Prior Authorization Request is approved?
A: Once approved, the dental provider can proceed with the authorized services and bill the insurance provider.
Q: What happens if a Dental Services Prior Authorization Request is denied?
A: If the request is denied, the dental provider may appeal the decision or explore other options for coverage or payment.
Form Details:
- Released on September 28, 2017;
- The latest edition currently provided by the Department of Vermont Health Access;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Department of Vermont Health Access.